文献精选
Authors
Victoria Eugenia Martinez-Miguel, Celia Lujan, Tristan Espie–Caullet, ..., Tobias von der Haar, Filipe Cabreiro, Ivana Bjedov
Correspondence
该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (F.C.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (I.B.)
In brief
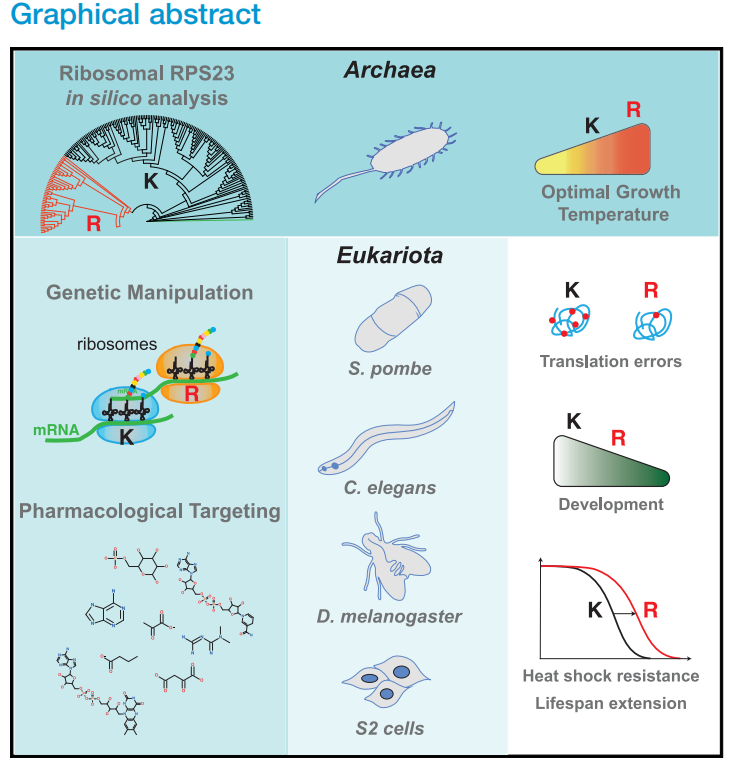
Martinez-Miguel et al. demonstrate that improving translation fidelity by mutating a single amino acid in the decoding center of the ribosome suffices to improve health and longevity in yeast, worms, and flies. This work provides a direct link between fewer errors in translation and longevity.
Highlights
● Evolutionarily selected arginine in RPS23 is present only in hyperthermophilic archaea
● RPS23 K60R mutation in flies leads to improved accuracy of protein synthesis with age
● Yeast, worm, and fly RPS23 K60R mutants are longer-lived, healthier, and heat resistant
● Anti-aging drugs, rapamycin, torin1, and trametinib, increase translation accuracy
Martinez-Miguel et al., 2021, Cell Metabolism 33, 2288–2300 November 2, 2021 ª 2021 The Author(s). Published by Elsevier Inc. https://doi.org/10.1016/j.cmet.2021.08.017
Victoria Eugenia Martinez-Miguel,1 Celia Lujan,1 Tristan Espie–Caullet,1 Daniel Martinez-Martinez,2,3 Saul Moore,2,3 Cassandra Backes,2,3 Suam Gonzalez,4 Evgeniy R. Galimov,2,3 Andre´ E.X. Brown,2,3 Mario Halic,5 Kazunori Tomita,6 Charalampos Rallis,4,11 Tobias von der Haar,7 Filipe Cabreiro,2,3,8, * and Ivana Bjedov1,9,10, *
1 UCL Cancer Institute, Paul O’Gorman Building, University College London, 72 Huntley Street, London WC1E 6DD, UK
2 MRC London Institute of Medical Sciences, Du Cane Road, London W12 0NN, UK
3 Institute of Clinical Sciences, Imperial College London, Hammersmith Hospital Campus, Du Cane Road, London W12 0NN, UK
4 School of Health, Sport and Bioscience, University of East London, Water Lane, London E15 4LZ, UK
5 Department of Structural Biology, St. Jude Children’s Research Hospital, 262 Danny Thomas Place, Memphis, TN 38105, USA
6 Centre for Genome Engineering and Maintenance, College of Health, Medicine and Life Sciences, Brunel University London, London UB8 3PH, UK
7 Kent Fungal Group, School of Biosciences, Division of Natural Sciences, University of Kent, Canterbury CT2 7NJ, UK
8 Cologne Excellence Cluster for Cellular Stress Responses in Aging-Associated Diseases (CECAD), University of Cologne, Joseph Stelzmann Strasse 26, 50931 Cologne, Germany
9 Department of Medical Physics and Biomedical Engineering, University College London, Malet Place Engineering Building, Gower Street, London WC1E 6BT, UK
10 Lead contact
11 Present address: School of Life Sciences, University of Essex, Wivenhoe Park, Colchester CO4 3SQ, UK
*Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (F.C.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (I.B.) https://doi.org/10.1016/j.cmet.2021.08.017
SUMMARY
Loss of proteostasis is a fundamental process driving aging. Proteostasis is affected by the accuracy of translation, yet the physiological consequence of having fewer protein synthesis errors during multi-cellular organismal aging is poorly understood. Our phylogenetic analysis of RPS23, a key protein in the ribosomal decoding center, uncovered a lysine residue almost universally conserved across all domains of life, which is replaced by an arginine in a small number of hyperthermophilic archaea. When introduced into eukaryotic RPS23 homologs, this mutation leads to accurate translation, as well as heat shock resistance and longer life, in yeast, worms, and flies. Furthermore, we show that anti-aging drugs such as rapamycin, Torin1, and trametinib reduce translation errors, and that rapamycin extends further organismal longevity in RPS23 hyperaccuracy mutants. This implies a unified mode of action for diverse pharmacological anti-aging therapies. These findings pave the way for identifying novel translation accuracy interventions to improve aging.
Antoine E. Roux,1 Chunlian Zhang,1 Jonathan Paw,1 Jose´ Zavala-Solorio,1 Evangelia Malahias,1 Twaritha Vijay,1 Ganesh Kolumam,1 Cynthia Kenyon,1 and Jacob C. Kimmel1,2,3, * 1Calico Life Sciences, LLC, 1170 Veterans Blvd, South San Francisco, CA 94080, USA
2Present Address: NewLimit, Inc., 901 Gateway Blvd, South San Francisco, CA 94080, USA
3Lead contact
*Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 https://doi.org/10.1016/j.cels.2022.05.002
SUMMARY
Partial pluripotent reprogramming can reverse features of aging in mammalian cells, but the impact on somatic identity and the necessity of individual reprogramming factors remain unknown. Here, we used single-cell genomics to map the identity trajectory induced by partial reprogramming in multiple murine cell types and dissected the influence of each factor by screening all Yamanaka Factor subsets with pooled single-cell screens. We found that partial reprogramming restored youthful expression in adipogenic and mesenchymal stem cells but also temporarily suppressed somatic identity programs. Our pooled screens revealed that many subsets of the Yamanaka Factors both restore youthful expression and suppress somatic identity, but these effects were not tightly entangled. We also found that a multipotent reprogramming strategy inspired by amphibian regeneration restored youthful expression in myogenic cells. Our results suggest that various sets of reprogramming factors can restore youthful expression with varying degrees of somatic identity suppression. A record of this paper’s Transparent Peer Review process is included in the supplemental information.
Helen C. Fraser1 | Valerie Kuan2,3,4 | Ronja Johnen5 | Magdalena Zwierzyna6 | Aroon D. Hingorani3,4,6 | Andreas Beyer5,7 | Linda Partridge1,8
1 Department of Genetics, Evolution and Environment, Institute of Healthy Ageing, University College London, London, UK
2 Institute of Health Informatics, University College London, London, UK
3 Health Data Research UK London, University College London, London, UK
4 University College London British Heart Foundation Research Accelerator, London, UK
5 Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD), Medical Faculty & Faculty of Mathematics and Natural
Sciences, University of Cologne, Cologne, Germany
6 Institute of Cardiovascular Science, University College London, UK
7 Centre for Molecular Medicine, University of Cologne, Cologne, Germany
8 Max Planck Institute for Biology of Ageing, Cologne, Germany
Correspondence
Andreas Beyer, Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD), Medical Faculty & Faculty of Mathematics and Natural Sciences, University of Cologne, Cologne, Germany.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Linda Partridge, Institute of Healthy Ageing, Department of Genetics, Evolution and Environment, University College London, London, UK.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Funding information
Bundesministerium für Bildung und Forschung, Grant/Award Number: HiGHmed 01ZZ1802U; UK Medical Research Council, Grant/Award Number: MR/N013867/1; Dunhill Medical Trust, Grant/Award Number: RPGF1806/67; BenevolentAI; Max- Planck-Gesellschaft; Wellcome Trust, Grant/Award Number: WT 110284/Z/15/Z; Deutsche Forschungsgemeinschaft, Grant/Award Number: CRC1310 and 325931972; British Heart Foundation, Grant/Award Number: AA/18/6/34223; European Research Council (ERC)
Abbreviations: AH, Aging hallmark; ARD, Age-related disease; EBI, European Bioinformatics Institute; ERK, Extracellular signal regulated kinase; GO, Gene Ontology; GSEA, Gene set
enrichment analysis; GWA, Genome-wide association; IFNg, Interferon gamma; MeSH, Medical Subject Headings; NCBI, National Centre for Biotechnology Information; NHGRI, National Human Genome Research Institute; PMID, PubMed unique Identifier; SNP, Single-nucleotide Polymorphism.
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
© 2022 The Authors. Aging Cell published by Anatomical Society and John Wiley & Sons Ltd.
Abstract
Genetic, environmental, and pharmacological interventions into the aging process can confer resistance to multiple age-related diseases in laboratory animals, including rhesus monkeys. These findings imply that individual mechanisms of aging might contribute to the co-occurrence of age-related diseases in humans and could be targeted to prevent these conditions simultaneously. To address this question, we text mined 917,645 literature abstracts followed by manual curation and found strong, nonrandom associations between age-related diseases and aging mechanisms in humans, confirmed by gene set enrichment analysis of GWAS data. Integration of these associations with clinical data from 3.01 million patients showed that age-related diseases associated with each of five aging mechanisms were more likely than chance to be present together in patients. Genetic evidence revealed that innate and adaptive immunity, the intrinsic apoptotic signaling pathway and activity of the ERK1/2 pathway were associated with multiple aging mechanisms and diverse age-related diseases. Mechanisms of aging hence contribute both together and individually to age-related disease co-occurrence in humans and could potentially be targeted accordingly to prevent multimorbidity.
KEYWORDS
age-related disease, aging, aging hallmarks, genetics, multimorbidity
Aging is characterized by a progressive loss of physiological integrity, leading to impaired function and increased vulnerability to death. This deterioration is the primary risk factor for major human pathologies, including cancer, diabetes, cardiovascular disorders, and neurodegenerative diseases. Aging research has experienced an unprecedented advance over recent years, particularly with the discovery that the rate of aging is controlled, at least to some extent, by genetic pathways and biochemical processes conserved in evolution. This Review enumerates nine tentative hallmarks that represent common denominators of aging in different organisms, with special emphasis on mammalian aging. These hallmarks are: genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and altered intercellular communication. A major challenge is to dissect the interconnectedness between the candidate hallmarks and their relative contributions to aging, with the final goal of identifying pharmaceutical targets to improve human health during aging, with minimal side effects.