While dressings play a key role in the management of open wounds and closed surgical incision sites, more specialised interventions are often required; for example, when exudate levels are high or patients are considered to be at high risk for wound complications.
One such intervention is negative pressure wound therapy (NPWT) which, in simple terms, can be described as the topical application of negative (sub-atmospheric) pressure at the wound-dressing interface. This is achieved by covering or filling a wound (depending on depth) with a dressing (typically foam or gauze), creating a seal (with an adhesive dressing or occlusive drape) before applying negative pressure via tubes which connect the dressing to a pump and a fluid-collection canister (Norman et al, 2020).
NPWT is a widely accepted technology for the management of a diverse range of acute and chronic wounds. It removes excess fluid (that may contain bacterial pathogens), reduces soft-tissue oedema, promotes granulation tissue formation (reducing wound volume), as well as providing a moist environment that is conducive to healing (Grant-Freemantle et al, 2020; Jiang et al, 2021; Song et al, 2021).
Closed-incision NPWT, i.e. the application of NPWT to closed surgical incision sites, is increasingly being used as research indicates that it is more effective than conventional postoperative dressings at reducing the occurrence of incision site complications (Sahebally et al, 2018; Shiroky et al, 2020; Ailaney et al, 2021; Boland et al, 2021).
Mechanisms of action of closed-incision NPWT include: the reduction in lateral tension across the wound, the improvement in lymphatic drainage, the reduction in size of seromas and haematomas, and the improvement in perfusion (Davies, 2022).
Historically, the size and weight of the pumps and their reliance on a main electricity source restricted NPWT to acute care settings. However, with portable, single-use negative pressure wound therapy (suNPWT) systems now commercially available that are relatively small, lightweight and powered mechanically or by batteries, NPWT is now a viable intervention for use in post-acute and home care settings (Orlov and Gefen, 2022). The available suNPWT systems are either canister-based (CB) or canister-less (CL). CB suNPWT systems incorporate a canister in their design which enables exudate and infectious material to be continually removed from the dressing that is in contact with the wound, whereas CL suNPWT systems rely solely on the dressings to manage exudate by absorption and evaporation (Henriksson, 2021).
Symposium proceedings
This report details a Mölnlycke-sponsored symposium held during the European Wound Management Association (EWMA) conference in Milan, Italy, on May 4, 2023. The symposium was chaired by Dr Marino Ciliberti and included presentations on the following:
■ Mechanism of action and critical performance measures for NPWT systems — an introduction to the influence zone theory (Prof Amit Gefen)
■ Using a simulated wound model to compare the technical performance of suNPWT systems (Dr Anette Svensson Henriksson)
■ Early clinical experiences of using CB suNPWT systems in the management of closed surgical incision sites (Dr Sanna Kouhia)
■ Use of CB suNPWT systems in the management of open wounds — a focus on perfusion (Dr Marino Ciliberti).
NPWT and the influence zone theory
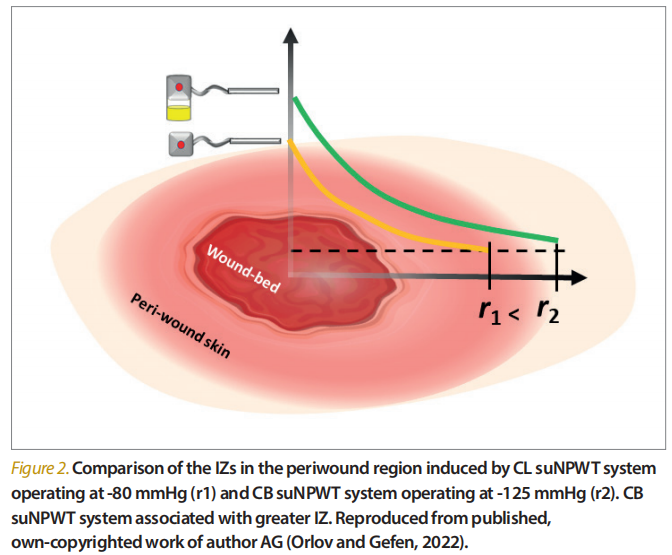
In the first presentation, Amit Gefen introduced the influence zone (IZ) theory in the context of NPWT. The IZ is a quantitative bioengineering performance measure that can be used t indicate the effectiveness of NPWT systems; in particular, how far from the wound bed edges a specific system is able to deliver effective mechano-stimulation into the periwound, and at what intensity [Figures 1 and 2] (Gefen, 2022).
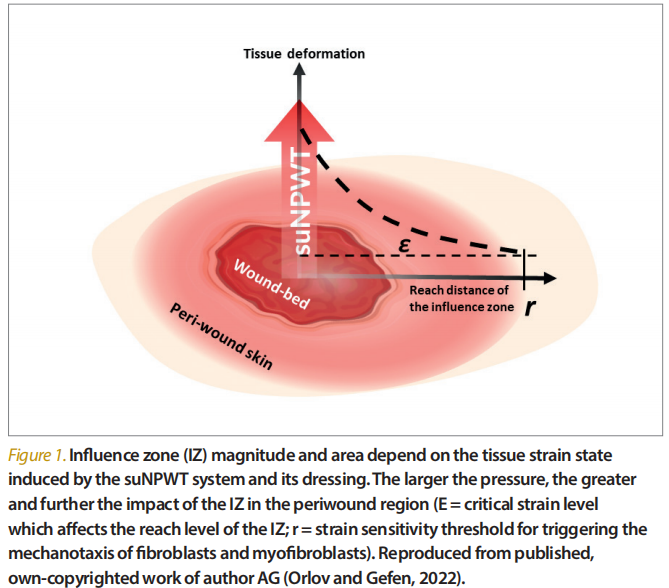
The IZ provides objective and standardised metrics of one of the fundamental modes of action of NPWT systems — the ability to effectively and optimally deform both the wound and periwound macroscopically and microscopically. Most important is the mechanical deformation of the periwound area to activate cells responsible for tissue repair, particularly fibroblasts and myofibroblasts. A larger IZ by a NPWT system means more fibroblasts can be stimulated. However, the level of mechanical stimulation delivered to the periwound area by an NPWT system must be optimal. If the tissue deformations are too low, they will not be sensed by the target cells, or by a significant number of these cells, and may not have a positive impact on the wound healing process. Alternatively, if deformations in the periwound area are excessively high, they may cause damage to cells or tissues, leading to wound deterioration.
It was emphasised that quantifying the effect of NPWT on the periwound area is more important than that on the wound itself.
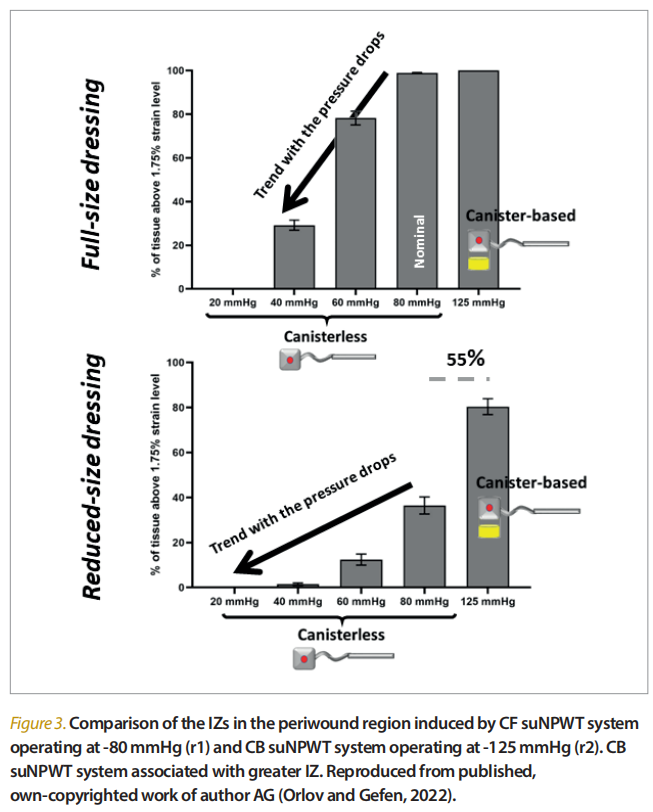
Continuous and consistent delivery of the intended pressure level by an NPWT system is critical for maintaining an effective IZ throughout the period of treatment. In one study, loss of negative pressure at the wound bed below 40mmHg adversely lowered the periwound stimulation, and further pressure decreases to 20mmHg or lower resulted in complete lack of periwound mechanostimulation [Figure 3] (Orlov and Gefen, 2022). Motile cells, including dermal fibroblasts, are mechano-sensitive and tend to migrate towards a sufficiently large (but not damaging) mechanical strain signal. Through some cell migration studies (Orlov and Gefen, 2022), it was found that a 1.75% dermal strain level defined the boundaries of the IZ (i.e. fibroblasts are insensitive to a lower-strain stimulation; Katzengold et al, 2021).
Comparing the technical performance of suNPWT systems using a simulated wound model
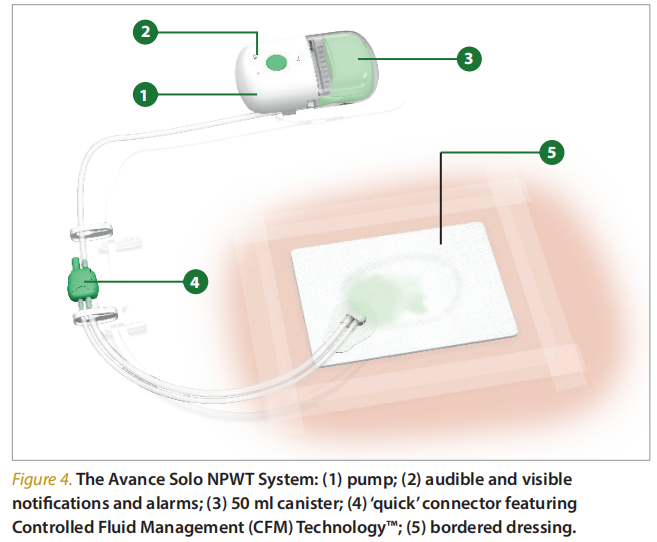
Anette Henriksson began her presentation with an introduction to Avance® Solo (Mölnlycke), a CB suNPWT system. It comprises a pump, which delivers regulated pressure (−125mmHg) to the wound for up to 14 days, audible and visible notifications and alarms which are activated when at risk for loss of therapy, a 50ml canister, and a ‘quick’ connector featuring Controlled Fluid Management (CFM) Technology™ to provide controlled inflow of air [Figure 4]. This allows the transportation of excess exudate to the canister from a bordered dressing. The dressing incorporates a Safetac® (soft silicone adhesive) wound contact surface which ensures minimal trauma and pain at dressing changes. A foam-based wound filler is also supplied with the system.
Due to its light weight and portability, the system allows patients to be mobile while delivering negative pressure (Henriksson, 2021). It is indicated for the removal of low-to-moderate exudate in a variety of wound types, including:
■ Surgically closed incisions
■ Open wounds (chronic, acute, traumatic, subacute and dehisced wounds; ulcers such as diabetes-related, venous or pressure); flaps and grafts).
Unlike CL suNPWT systems, which rely solely on the dressings to manage exudate by absorption and evaporation, with the Avance Solo NPWT System, exudate and infectious material are managed by a combination of absorption in the multilayer bordered dressing, and transport of excess fluid to the canister, thus reducing the risk of the dressing becoming saturated and interrupting the delivery of negative pressure to the wound and potentially decreasing the frequency of dressing changes (Henriksson, 2021; Orlov and Gefen, 2021; Davies, 2022).
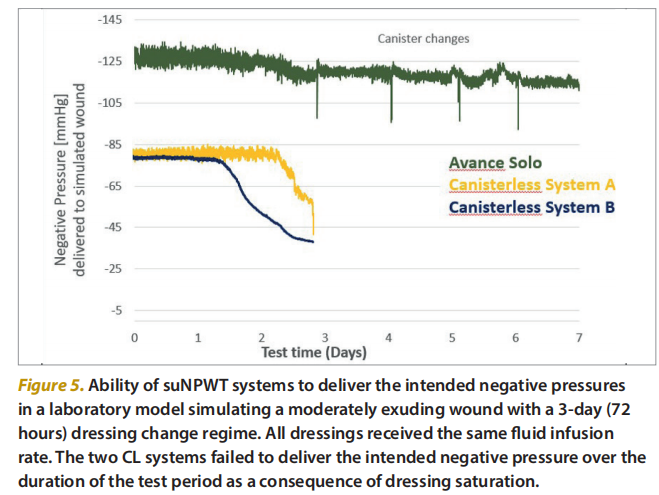
Anette then presented a summary of a study that set out to compare the technical performances of Avance Solo NPWT System (CB; −125mmHg) and two CL suNPWT (−80mmHg) systems in simulated clinical tests utilising a test method which simulated the clinical use of NPWT. The method involved subjecting the NPWT systems to a controlled inflow of simulated wound fluid. The performances of the systems were then assessed by comparing the negative pressure measured as output from the pump and at the simulated wound bed with the intended negative pressure over the duration of the test period (7 days). The CL suNPWT systems were associated with substantial reductions in the delivery of intended negative pressure fairly early on in the test, indicating that the permeability of negative pressure through the wound pad is impacted by accumulating fluid. In contrast, the Avance Solo NPWT system continuously delivered the intended pressure to the simulated wound bed throughout the test period, without any observed saturation of the dressings [Figure 5].
Finally, Anette briefly outlined the findings of an evaluation using pre-clinical wound models (open and closed incision) to compare the performance of Avance Solo NPWT system with that of a CL suNPWT system (−80mmHg). The evaluation focused on local tissue effects, the quality of repaired tissue, and fluid management over a 14-day period.
For the open wound model, there was very good healing progression overall, with the wounds almost completely filled by mature, or close to mature, granulation tissue by day 14. Furthermore, mean wound volume progressively decreased from 4.8 cm3 at day 0 to 0 cm3 at day 14. In terms of fluid management (measured at every dressing change by determining the weight of the dressings and, in the case of Avance Solo, the canister, the fluid collected from wounds was on average higher with Avance Solo than the CL suNPWT system. This observation may explain the observed higher occurrence of maceration, infection and protruding granulation tissue in the wounds that had the CL suNPWT system applied.
With regard to the closed incision model, histopathological analysis of the tissue samples undertaken at the end of the study period qualitatively demonstrated an overall faster onset of epidermalisation, more rapid epidermal differentiation and adherence to underlying granulation tissue for the incision wounds that had Avance Solo applied.
Use of suNPWT on closed surgical incisions
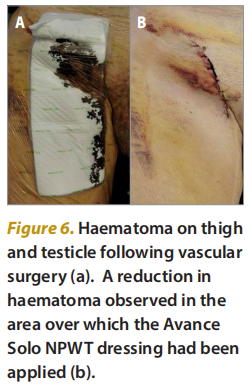
Having listened to the first two speakers talking about pre-clinical research, Dr Kouhia began her presentation by focussing on the key objectives of closed surgical incision care, i.e. to reduce oedema, minimise the risk of complications such as infection, dehiscence and haematomas, and, ultimately, heal the wound in a timely manner. She then pointed out that the appropriate use of closed incision NPWT can play a key role in achieving these goals [Figure 6].
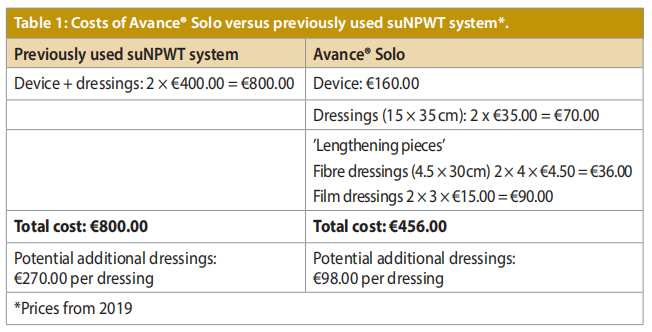
In the next part of her presentation, Dr Kouhia presented a simple cost comparison of the Avance Solo NPWT System with a previously used NPWT device. The comparison was made based on a typical 2-week treatment period for a single patient and revealed a cost saving of approximately €350 per patient with the use of Avance Solo [Table 1]. Dr Kouhia then referred to a recently published Cochrane review (Norman et al, 2022) relating to the use of NPWT for surgical wound healing by primary closure which concluded that there is moderatecertainty evidence that NPWT probably results in fewer SSIs that treatment with standard dressings after surgery. While acknowledging the robustness of the methodology used in systematic reviews, Dr Kouhia suggested that the pooling of data from divergent patient groups and the generalisations made from the subsequent analyses means that such reviews should not be used in isolation to decide on treatment strategies. Instead, healthcare professionals should “know their own data” and take into consideration patient risk stratification, procedure risk stratification and the specific challenges of different surgical sub-specialities when making informed decisions about the use of NPWT on closed surgical incisions.
Dr Kouhia finished her presentation by describing two case studies, one of which involved the use of Avance Solo NPWT System on a post-amputation incision site with significant lateral tension across the wound evidence. Four weeks after the commencement of Avance Solo NPWT System, the incision site had improved dramatically [Figure 7].

Use of suNPWT on open wounds
Dr Ciliberti spoke about the use of the Avance Solo suNPWT system in practice and presented data from a variety of cases involving different types of wounds (see Boxes 1–3 for summarised case studies).
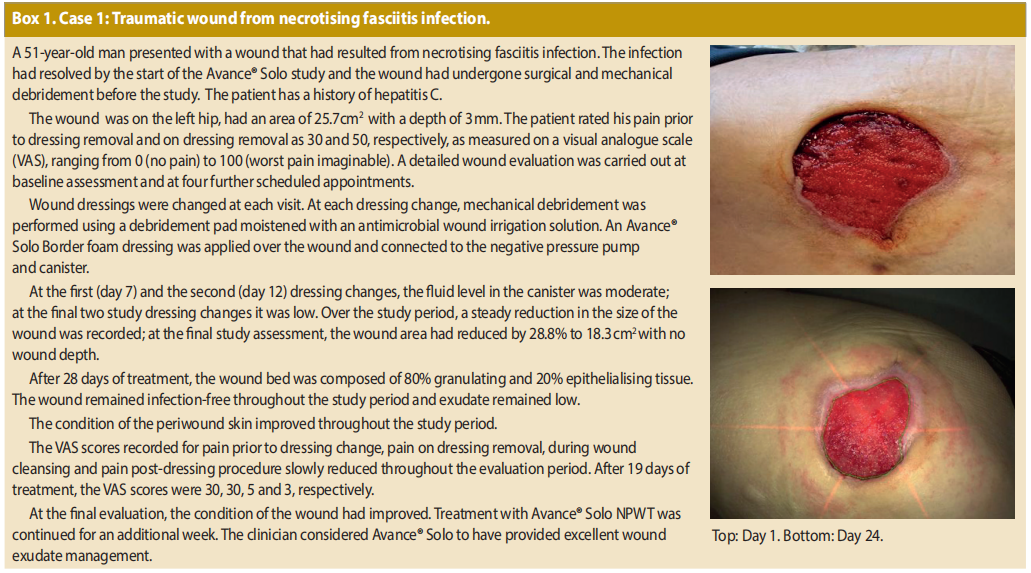
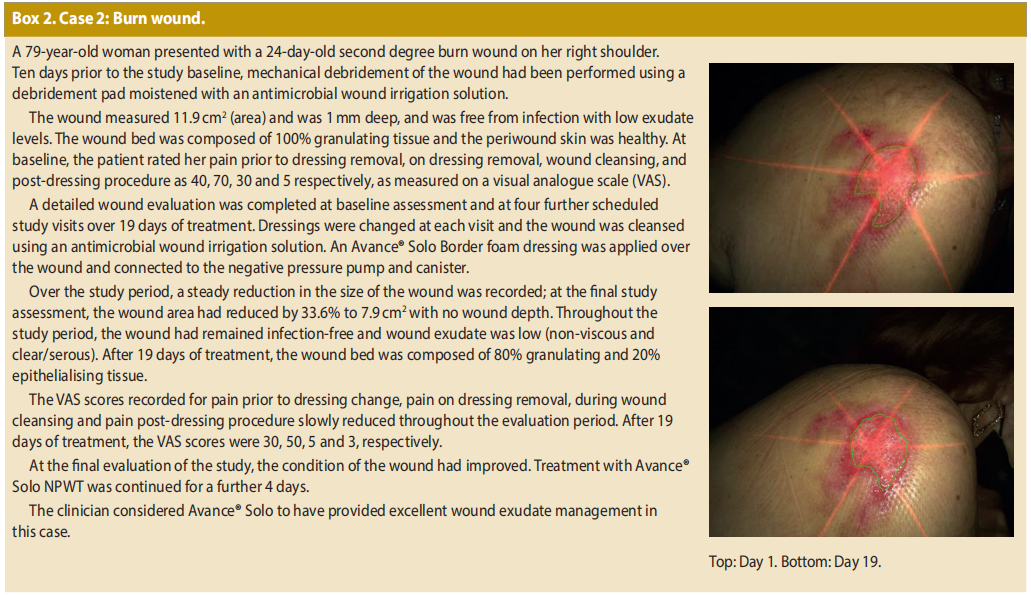
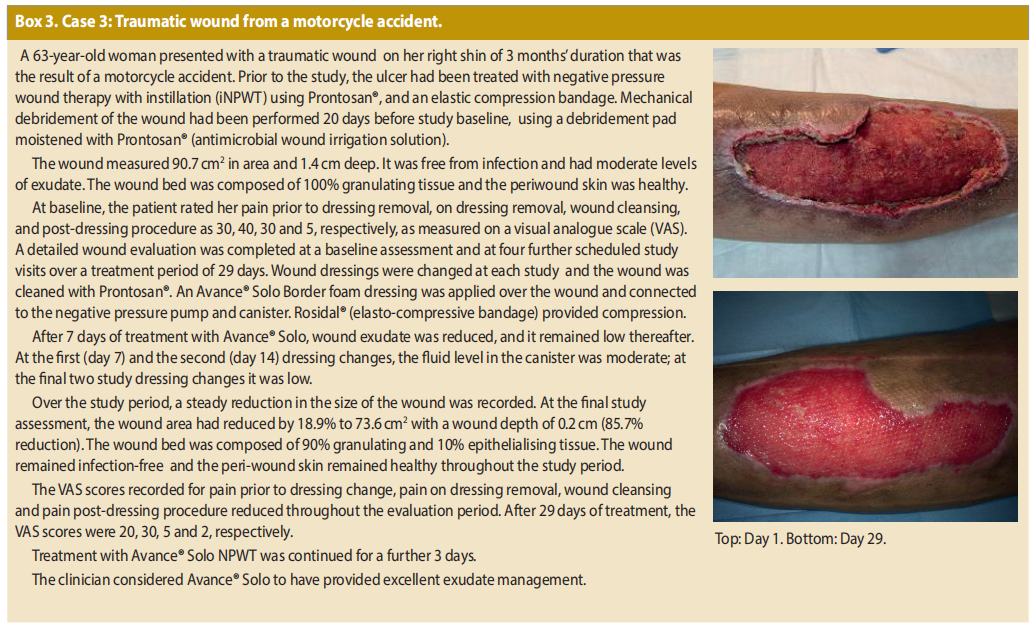
Dr Ciliberti outlined the pilot study undertaken at his hospital with the aim of focussing on the levels of exudate encountered in the wounds and the stimulation of perfusion when Avance Solo was used on a variety of open wounds.
Five patients with different aetiologies were treated with the suNPWT for a period of 4 weeks, with Dr Ciliberti and his colleagues measuring the quantity of exudate, as well as the dimensions of the wound and perfusion levels. He explained that perfusion around leg ulcers is commonly “very poor” at the wound bed and he highlighted the perfusion stimulation that took place after using suNPWT through the use of laser doppler imagery [Figure 8]. Before and after images were displayed and in all five cases there was an improvement in wound bed perfusion after treatment with Avance Solo.
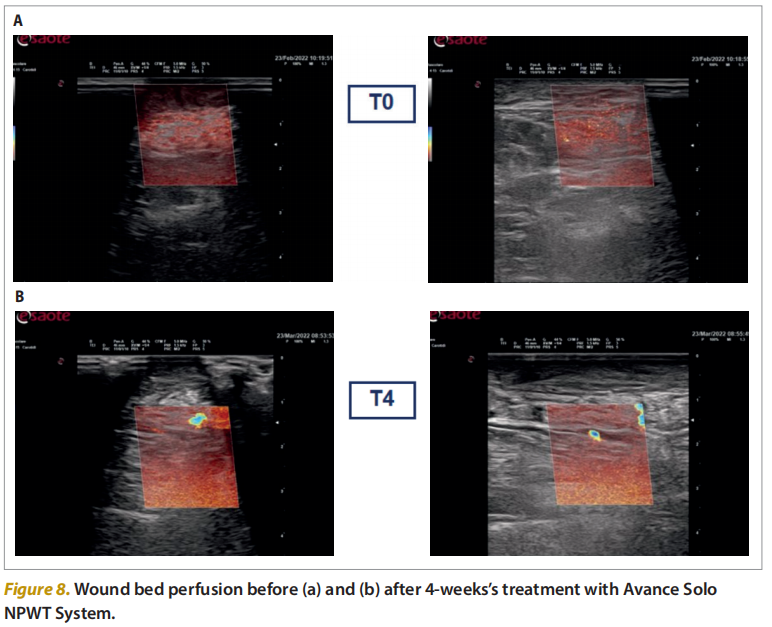
In one case outlined by Dr Ciliberti, a paraplegic patient presented with a decubitus wound to the ankle of 1-year duration. In this patient group, the healing rate is 40% lower when compared people with normal innervation (West et al 2013) but the use of suNPWT played a central role in improving perfusion, lowering exudate and reducing the wound area.
In addition, Avance Solo was found to improve perfusion, lower exudate, and reduce the wound area and depth in an individual with a chronic wound (4 years’ duration), a burn, necrotising fasciitis and a traumatic wound, underlining the flexibility of the suNPWT device when used on a range of wounds. Dr Ciliberti drew the audience’s attention to the performance of the device after 1 week of treatment, using graphs to show that each of the five cases displayed a marked improvement in terms of wound area.
Dr Ciliberti concluded by saying that the cases presented proved power and pressure effectiveness of suNPWT, the canister helped avoid maceration, wound management was effective, patient comfort was optimised and “perfusion is not an illusion”
Conclusion
There are now numerous products available offering viable alternatives to the original re-usable systems, which allow clinicians to select the best system to meet the needs and expectations of their patients.
By using the IZ theory, objective and standardised metrics of one of the fundamental modes of action of NPWT systems can be introduced to wound management. It is important to consider that the wound area and strain intensity characteristics of the IZ depend on the level of negative pressure delivered, in addition to the size, shape and mechanical properties of the suNPWT. A larger IZ created by a suNPWT system results in more fibroblasts being stimulated, which will then help repair the wound.
The importance of the cannister is underlined by the faster onset of epidermisation, epidermal differentiation and adherence to underlying granulation tissue for closed incisions treated by Avance Solo.
In terms of the clinical aspects of suNPWT, the case studies presented demonstrate the flexibility of Avance Solo — it can be used in the treatment of both closed surgical incisions and open wounds. Avance Solo can play an integral role in minimising the risk of complications, such as infection, dehiscence and haematomas, reducing oedema and promoting timely wound healing in closed surgical incisions.
On open wounds, Avance Solo can be expected to improve the condition of the wound bed, reduce exudation and decrease wound size, while stimulating perfusion. Avance Solo also offers a cost-effective alternative to other suNPWT systems.
References
1. Ailaney N, Johns WL, Golladay GJ et al (2021) Closed incision negative pressure wound therapy for elective hip and knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty 36(7): 2402–11
2. Boland PA, Kelly ME, Donlon NE et al (2021) Prophylactic negative pressure wound therapy for closed laparotomy wounds: a systematic review and meta-analysis of randomised controlled trials. Irish J Med Sci 190(1): 261–7
3. Davies P (2022) Closed Incision Negative Pressure Wound Therapy: A Literature Review and an Introduction to Avance® Solo. London: Wounds International
4. Gefen A (2022) The influence zone: a critical performance analysis measure for negative pressure wound therapy systems. Br J Nurs 31(15): S8–12
5. Grant-Freemantle MC, Ryan EJ, Flynn SO et al (2020) The effectiveness of negative pressure wound therapy versus conventional dressing in the treatment of open fractures: a systematic review and metaanalysis. J Orthop Trauma 34(5): 223–30
6. Henriksson AS (2021) Single use negative pressure wound therapy (suNPWT) system with controlled fluid management technology – an evaluation of performance. Wounds International 12(4): 62–8
7. Jiang ZY, Yu XT, Liao XC et al (2021) Negative-pressure wound therapy in skin grafts: a systematic review and meta-analysis of randomized controlled trials. Burns 47(4): 747–55
8. Katzengold R, Orlov A, Gefen A (2021) A novel system for dynamic stretching of cell cultures reveals the mechanobiology for delivering better negative pressure wound therapy. Biomech Model Mechanobiol 20(1): 193–204
9. Norman G, Goh EL, Dunville JC et al (2020) Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev 6(6): CD009261
10. Orlov A, Gefen A (2022) Effective negative pressure wound therapy for open wounds: the importance of consistent pressure delivery. Int Wound J 20(2): 328–44
11. Sahebally SM, McKevitt K, Stephens I et al (2018) Negative pressure wound therapy for closed laparotomy incisions in general and colorectal surgery: a systematic review and meta-analysis. J Am Med Assoc Surg 153(11): e183467
12. Shiroky J, Lillie E, Muaddi H et al (2020) The impact of negative pressure wound therapy for closed surgical incisions on surgical site infection: a systematic review and meta-analysis. Surgery 167(6): 1001–9
13. Song YP, Wang L, Yuan B-F et al (2021) Negative-pressure wound therapy for III/IV pressure injuries: a metaanalysis. Wound Repair Regen 29(1): 20–33
14. West C, Alyahya A, Lather I et al (2013) Peripheral vascular function in spinal cord injury: a systematic review. Spinal Cord 51(1): 10–9
This article is excerpted from the Wounds International 2023 | Vol 14 Issue 4 | by Wound World.