文献精选





This article is excerpted from the《Frontiers in Neurology》 by Wound World


This article is excerpted from the《Frontiers in Neurology》 by Wound World




This article is excerpted from the《Frontiers in Neurology》 by Wound World
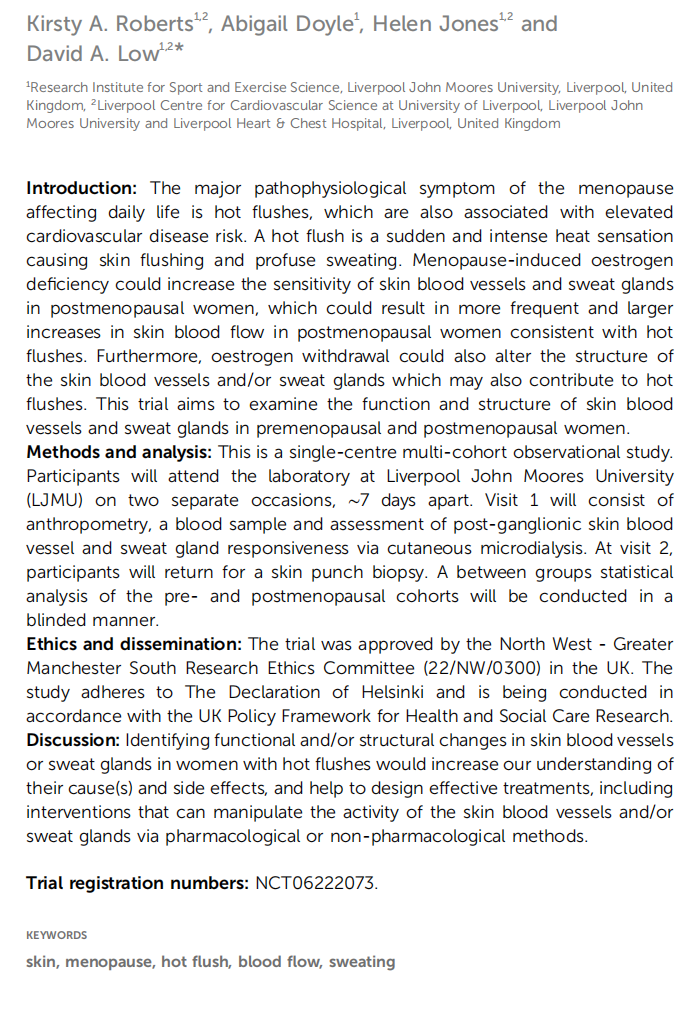


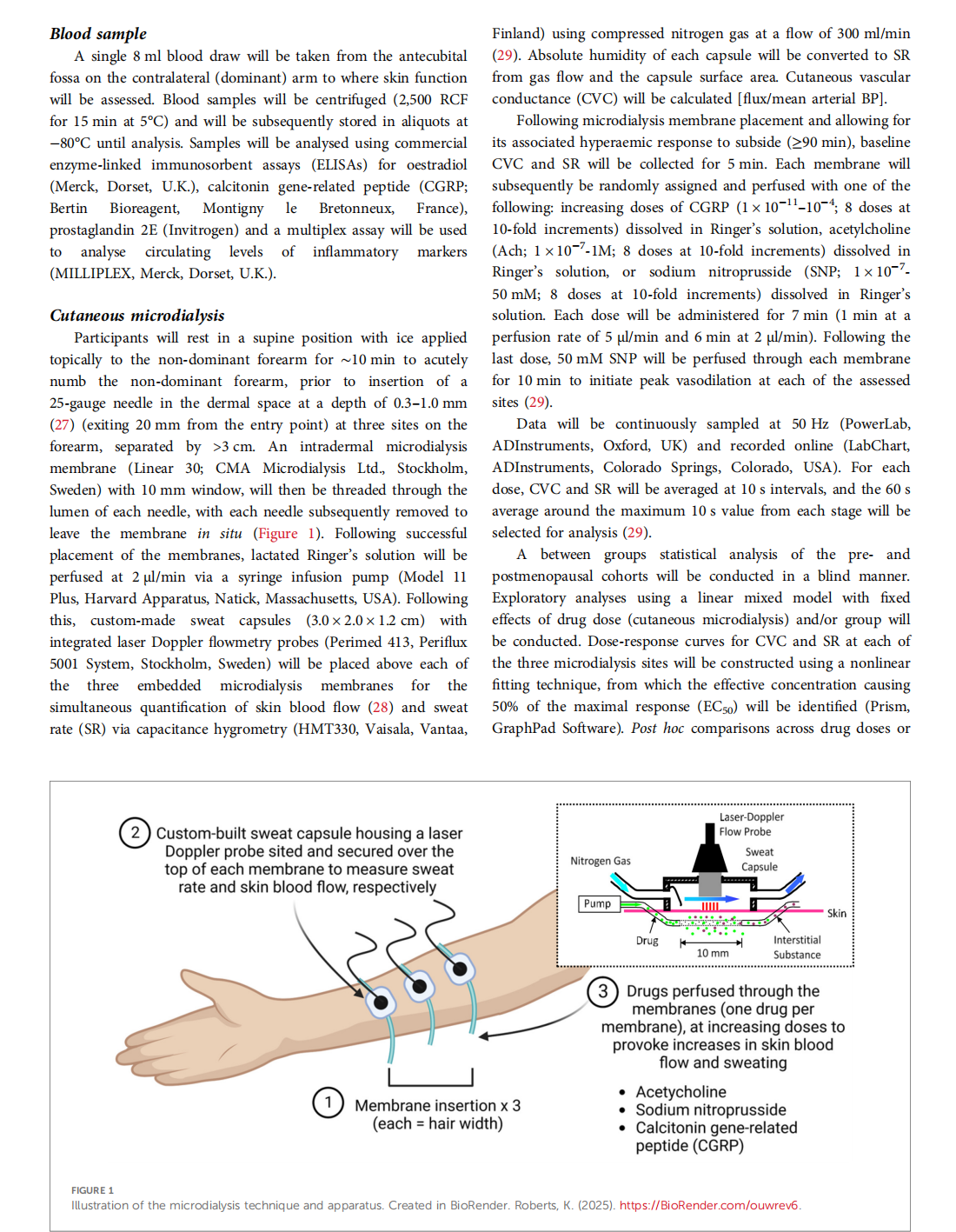

This article is excerpted from the 《Frontiers in Global Women's Health》 by Wound World