
伤口世界

- 星期二, 17 6月 2025
Contrasting somatic mutation patterns in aging human neurons and oligodendrocytes
Javier Ganz,1,2,3,8,9 Lovelace J. Luquette,4,8 Sara Bizzotto,1,2,3,5,8 Michael B. Miller,1,3,6 Zinan Zhou,1,2,3 Craig L. Bohrson,4
Hu Jin,4 Antuan V. Tran,4 Vinayak V. Viswanadham,4 Gannon McDonough,6 Katherine Brown,6 Yasmine Chahine,1
Brian Chhouk,1 Alon Galor,4 Peter J. Park,4,7,* and Christopher A. Walsh1,2,3,10,*
1 Division of Genetics and Genomics, Manton Center for Orphan Disease Research, Department of Pediatrics, and Howard Hughes Medical Institute, Boston Childrens Hospital, Boston, MA 02115, USA
2 Departments of Pediatrics and Neurology, Harvard Medical School, Boston, MA 02115, USA
3 Broad Institute of MIT and Harvard, Cambridge, MA 02142, USA
4 Department of Biomedical Informatics, Harvard Medical School, Boston, MA 02115, USA
5 Sorbonne Universite´ , Institut du Cerveau (Paris Brain Institute) ICM, Inserm, CNRS, Hoˆ pital de la Pitie´ Salpeˆ trie`re, 75013 Paris, France
6 Department of Pathology, Brigham and Womens Hospital, Harvard Medical School, Boston, MA 02115, USA
7 Division of Genetics, Brigham and Womens Hospital, Boston, MA 02115, USA
8 These authors contributed equally
9 Present address: Merck Research Laboratories, Cambridge, MA 02142, USA
10 Lead contact
*Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (P.J.P.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (C.A.W.)
https://doi.org/10.1016/j.cell.2024.02.025
SUMMARY
Characterizing somatic mutations in the brain is important for disentangling the complex mechanisms of aging, yet little is known about mutational patterns in different brain cell types. Here, we performed wholegenome sequencing (WGS) of 86 single oligodendrocytes, 20 mixed glia, and 56 single neurons from neurotypical individuals spanning 0.4–104 years of age and identified >92,000 somatic single-nucleotide variants (sSNVs) and small insertions/deletions (indels). Although both cell types accumulate somatic mutations linearly with age, oligodendrocytes accumulated sSNVs 81% faster than neurons and indels 28% slower than neurons. Correlation of mutations with single-nucleus RNA profiles and chromatin accessibility from the same brains revealed that oligodendrocyte mutations are enriched in inactive genomic regions and are distributed across the genome similarly to mutations in brain cancers. In contrast, neuronal mutations are enriched in open, transcriptionally active chromatin. These stark differences suggest an assortment of active mutagenic processes in oligodendrocytes and neurons.

- 星期一, 16 6月 2025
Contrasting somatic mutation patterns in aging human neurons and oligodendrocytes
an Yang1 Xinyuan Zhang2 Hua Wang1 Miao Guo1 Jinlong Zhang1 Xuejiao Feng3 Jiayi Yu3 Jiahui Yang3 Jinjin Zhu4 Yiyu Wang3
1 Research & Development Center, Mageline Biology Tech Co., Ltd, Wuhan, Hubei, China
2 Shanghai Skinshield Clinical Testing and Technological Research Ltd., Shanghai, China
3 Department of Dermatology, Air Force Medical Center, PLA, Beijing, China
4 Department of Dermatology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (HUST), Wuhan, China
Correspondence
Jinjin Zhu, Department of Dermatology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (HUST), Wuhan, 430022, China.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Yiyu Wang, Department of Dermatology, Air Force Medical Center, PLA, Beijing, China.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Abstract
Background: The delicate periorbital region is susceptible to skin dehydration, wrinkles, and loss of elasticity. Thus, targeted and effective anti-aging interventions are necessary for the periorbital area.
Aim: To evaluate the efficacy and safety of a new anti-aging eye cream formulated with the active complex (Yeast/rice fermentation filtrate, N-acetylneuraminic acid, palmityl tripeptide-1, and palmitoyl tetrapeptide-7).
Methods: The cell viability and expressions of key extracellular matrix (ECM) components of the active complex were evaluated using a human skin fibroblast model. In the 12-week clinical trial, skin hydration, elasticity, facial photographs, and collagen density following eye cream application were assessed using Corneometer, Cutometer, VISIA, and ultrasound device, respectively. Dermatologists and participants evaluated clinical efficacy and safety at baseline, and after 4, 8, and 12 weeks.
Results: PCR and immunofluorescent analyses revealed that the active complex significantly stimulated fibroblast proliferation (p < 0.05) and markedly promote the synthesis of collagen and elastin. Clinical findings exhibited a substantial enhancement in skin hydration (28.12%), elasticity (18.81%), and collagen production (54.99%) following 12 weeks of eye cream application. Dermatological evaluations and participants’ assessments reported a significant improvement in skin moisture, roughness, elasticity, as well as fine lines and wrinkles by week 8.
Conclusion: The new anti-aging eye cream, enriched with the active complex, demonstrates comprehensive rejuvenating effects, effectively addressing aging concerns in the periorbital area, coupled with a high safety profile.
KEYWORDS
anti-aging, collagen, elastin, extracellular matrix, eye cream, wrinkle

- 星期五, 13 6月 2025
A Comprehensive Review of Stem Cell Conditioned Media Role for Anti-Aging on Skin
yatulloh Alquraisy1 , Gofarana Wilar 2 , Ahmed Fouad Abdelwahab Mohammed3 , Ali El-Rayyes4 , Cecep Suhandi 1, Nasrul Wathoni 1
1 Department of Pharmaceutics and Pharmaceutical Technology, Faculty of Pharmacy, University of Padjadjaran, Sumedang, 45363, Indonesia;
2 Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, University of Padjadjaran, Sumedang, 45363, Indonesia; 3 Department of Pharmaceutics, Faculty of Pharmacy, Minia University, Minia, 61519, Egypt; 4 Department of Chemistry, College of Science, Northern Border University, Arar, Saudi Arabia
Correspondence: Nasrul Wathoni, Email 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Abstract: Various studies have been widely conducted on conditioned medium for the development of anti-aging preparations, including the utilization of stem cells, which present a promising alternative solution. This narrative review aims to understand the latest developments in various conditioned medium stem cell applications for anti-aging on the skin. A search of the Scopus database yielded publications of interest. The research focused on articles published without restrictions on the year. After finding 68 articles in the search results, they moved on to the checking phase. Upon comprehensive literature review, 23 articles met the inclusion criteria, while 45 articles were deemed ineligible for participation in this research. The results of the review indicate that conditioned medium from various stem cells has demonstrated success in reducing risk factors for skin aging, as proven in various tests. The successful reduction of the risk of skin aging has been established in vitro, in vivo, and in clinical trials. Given the numerous studies on the progress of exploring and utilizing conditioned medium, it is expected to provide a solution to the problem of skin aging.
Keywords: conditioned medium, stem cell, anti-aging, skin aging

- 星期四, 12 6月 2025
Oral Administration of Nacre Extract from Pearl Oyster Shells Has Anti-Aging Effects on Skin and Muscle, and Extends the Lifespan in SAMP8 Mice
Hana Yamamoto, Nanami Shimomura and Yasushi Hasegawa
College of Environmental Technology, Muroran Institute of Technology, 27-1 Mizumoto, Muroran 050-8585, Japan; 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (H.Y.); 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (N.S.)
* Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。; Tel.: +81-143-46-5745
Abstract: Pearl oysters have been extensively utilized in pearl production; however, most pearl oyster shells are discarded as industrial waste. In a previous study, we demonstrated that the intraperitoneal administration of pearl oyster shell-derived nacre extract (NE) prevented d-galactose-induced brain and skin aging. In this study, we examined the anti-aging effects of orally administered NE in senescence-accelerated mice (SAMP8). Feeding SAMP8 mice NE prevented the development of aging-related characteristics, such as coarse and dull hair, which are commonly observed in aged mice. Additionally, the NE mitigated muscle aging in SAMP8 mice, such as a decline in grip strength. Histological analysis of skeletal muscle revealed that the NE suppressed the expression of aging markers, cyclin-dependent kinase inhibitor 2A (p16) and cyclin-dependent kinase inhibitor 1 (p21), and increased the expression of sirtuin1 and peroxisome proliferator-activated receptor gamma coactivator 1 (PGC1)- α, which are involved in muscle synthesis. These findings suggest that the oral administration of NE suppresses skeletal muscle aging. Moreover, NE administration suppressed skin aging, including a decline in water content. Interestingly, oral administration of NE significantly extended the lifespan of SAMP8 mice, suggesting that its effectiveness as an anti-aging agent of various tissues including skeletal muscle, skin, and adipose tissue.
Keywords: skeletal muscle aging; nacre extract; lifespan extension; sarcopenia; skin aging
Citation: Yamamoto, H.; Shimomura,
N.; Hasegawa, Y. Oral Administration
of Nacre Extract from Pearl Oyster
Shells Has Anti-Aging Effects on Skin
and Muscle, and Extends the Lifespan
in SAMP8 Mice. Pharmaceuticals 2024,
17, 713. https://doi.org/
10.3390/ph17060713
Academic Editors: Mariia Shanaida,
Geir Bjørklund and Olha
Mykhailenko
Received: 16 May 2024
Revised: 28 May 2024
Accepted: 29 May 2024
Published: 31 May 2024
- 星期二, 10 6月 2025
Macrofungal Extracts as a Source of Bioactive Compounds for Cosmetical Anti-Aging Therapy: A Comprehensive Review(2-2)
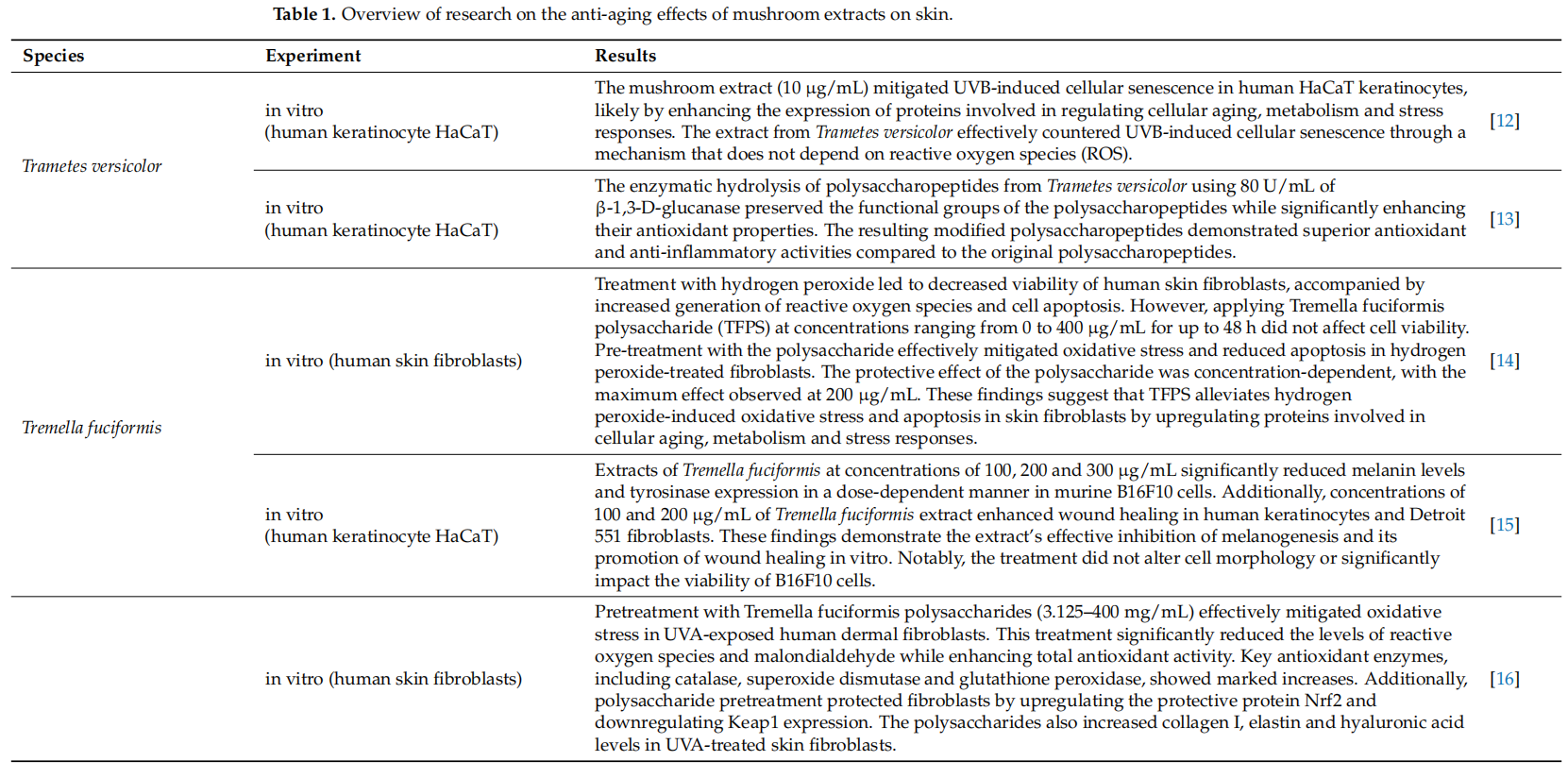
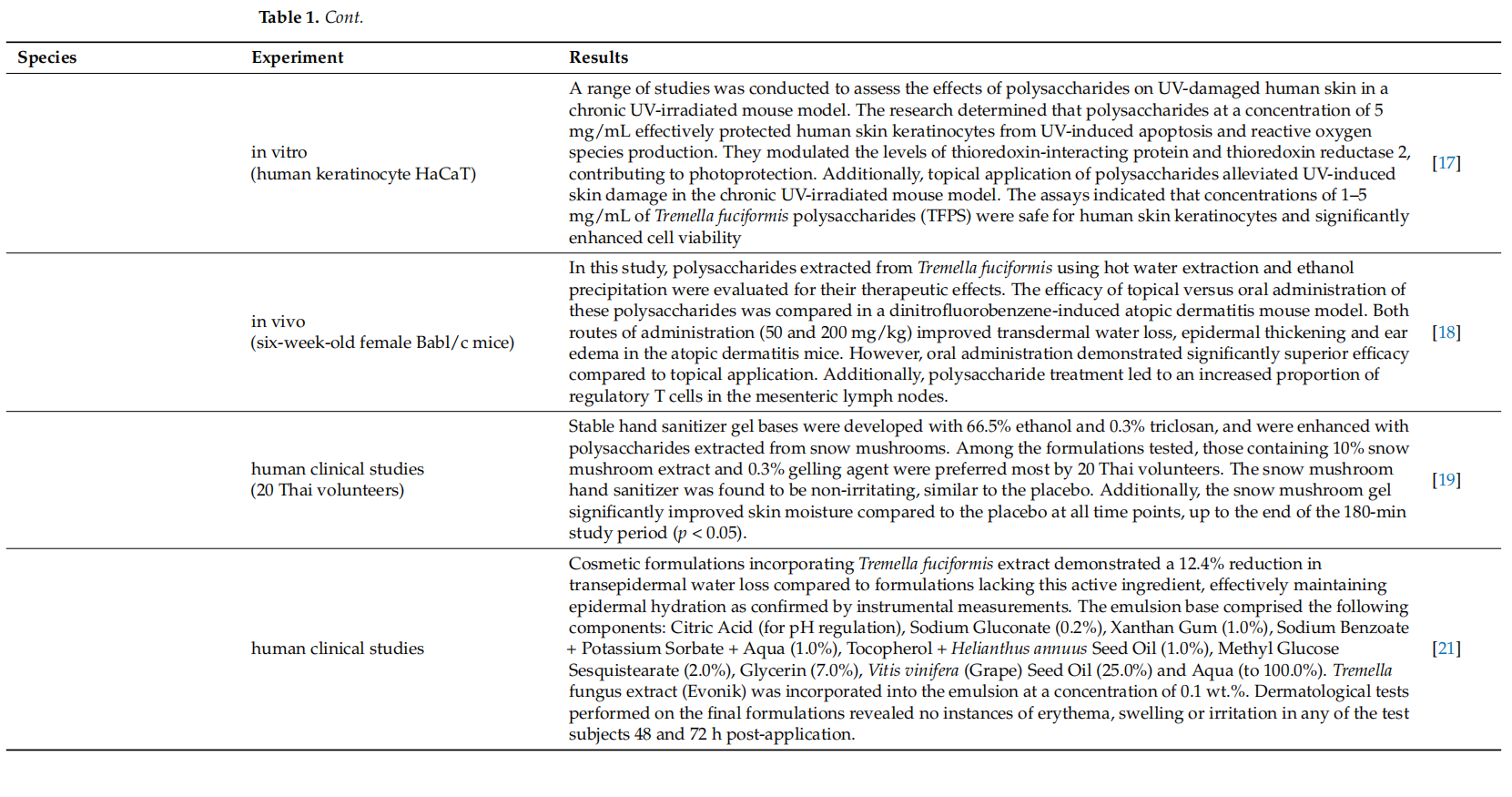
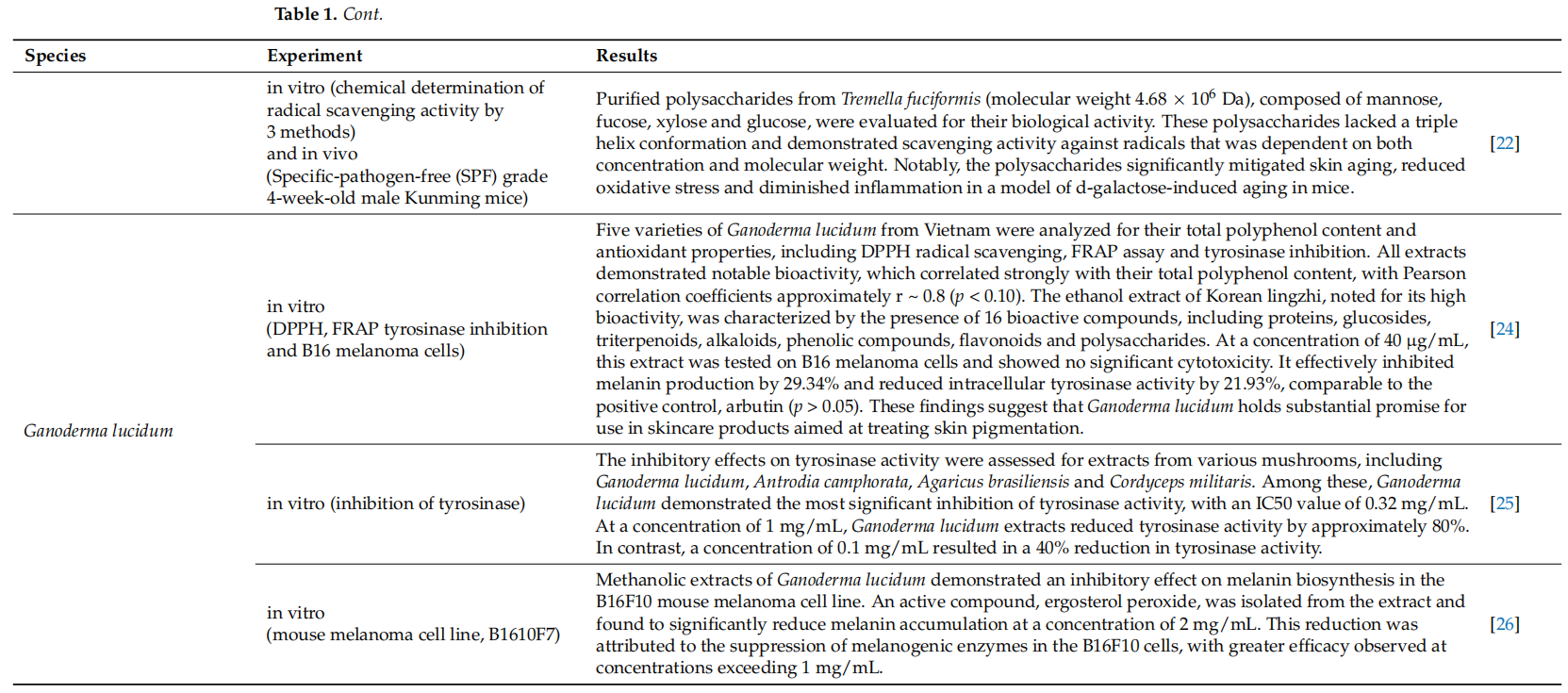
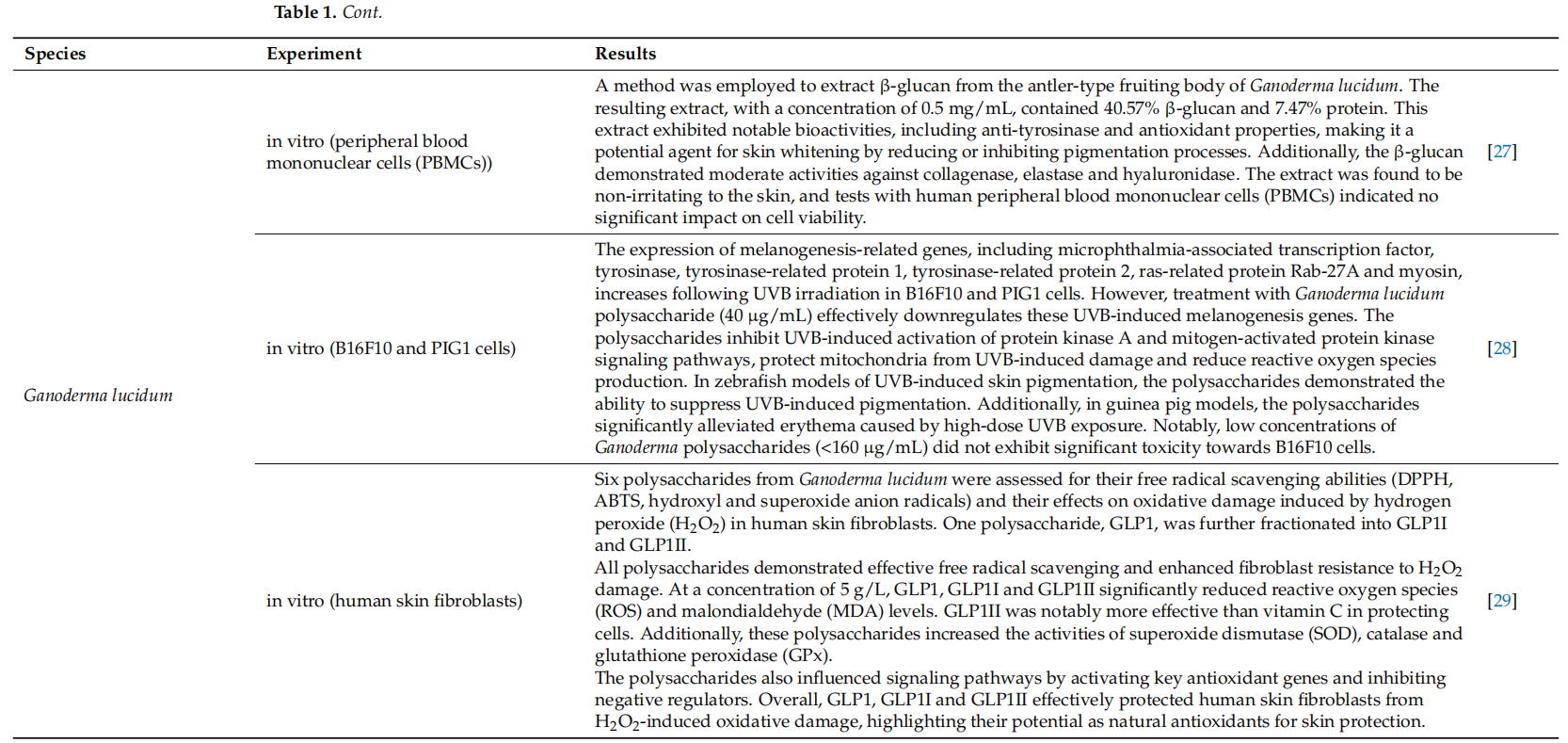
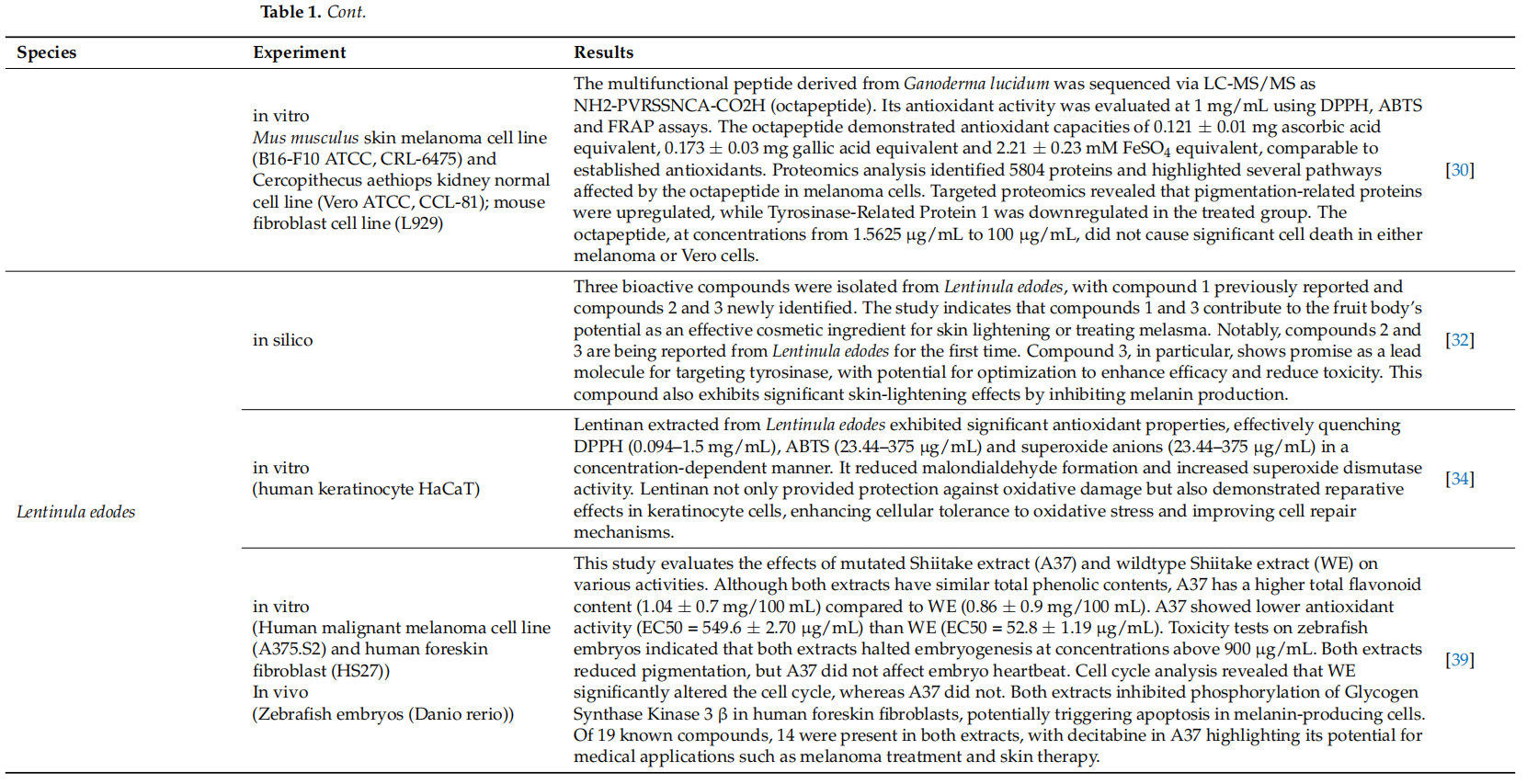
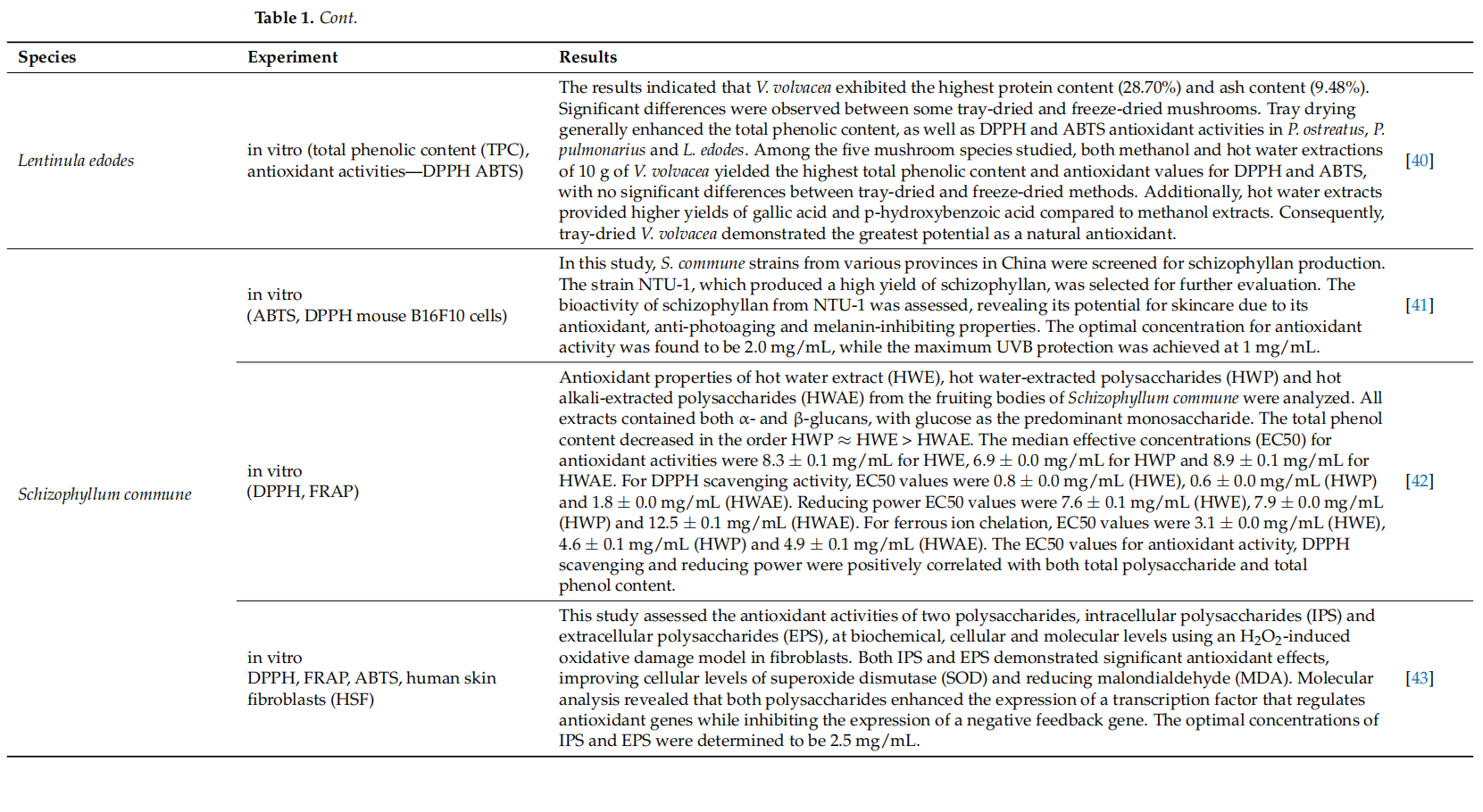
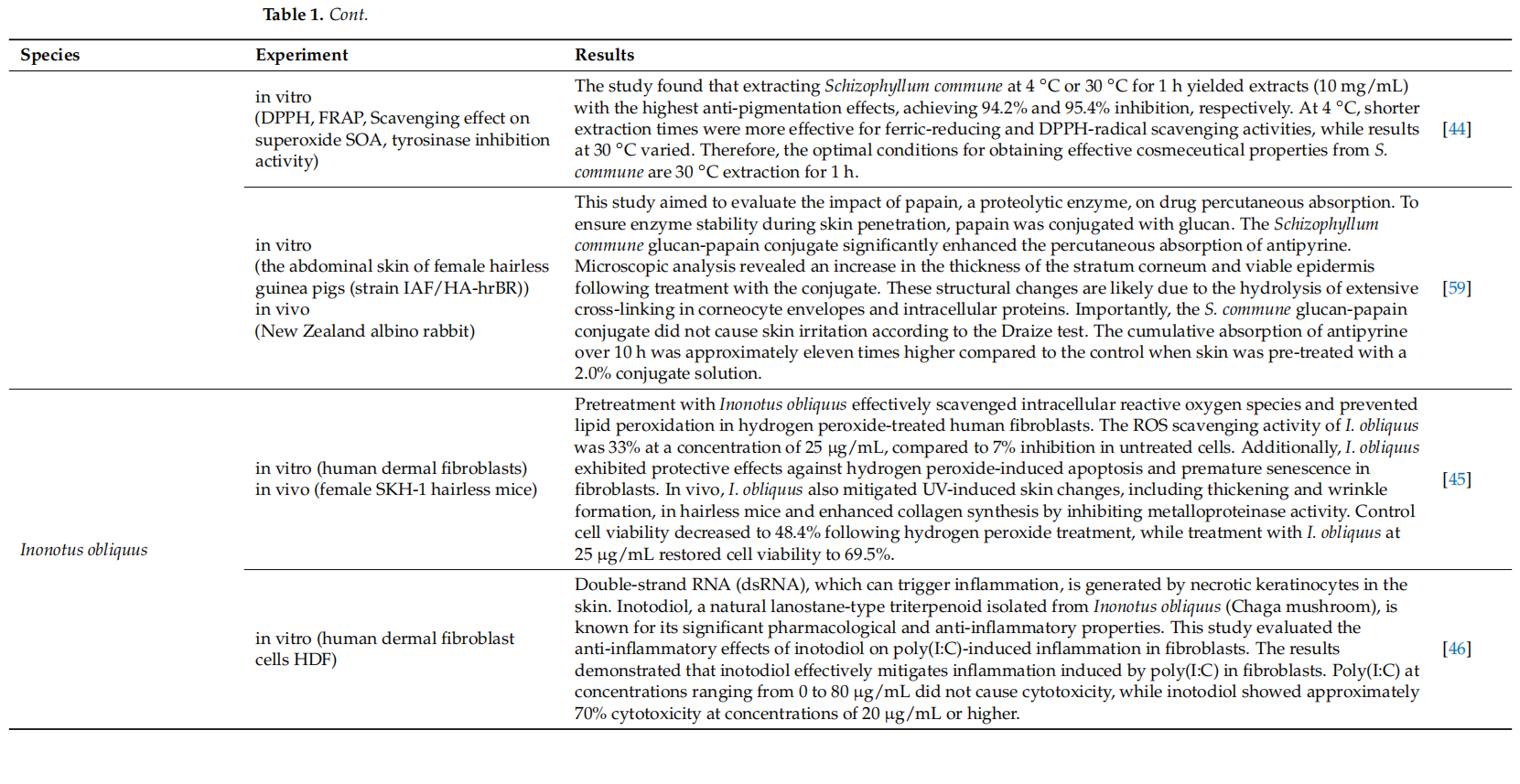
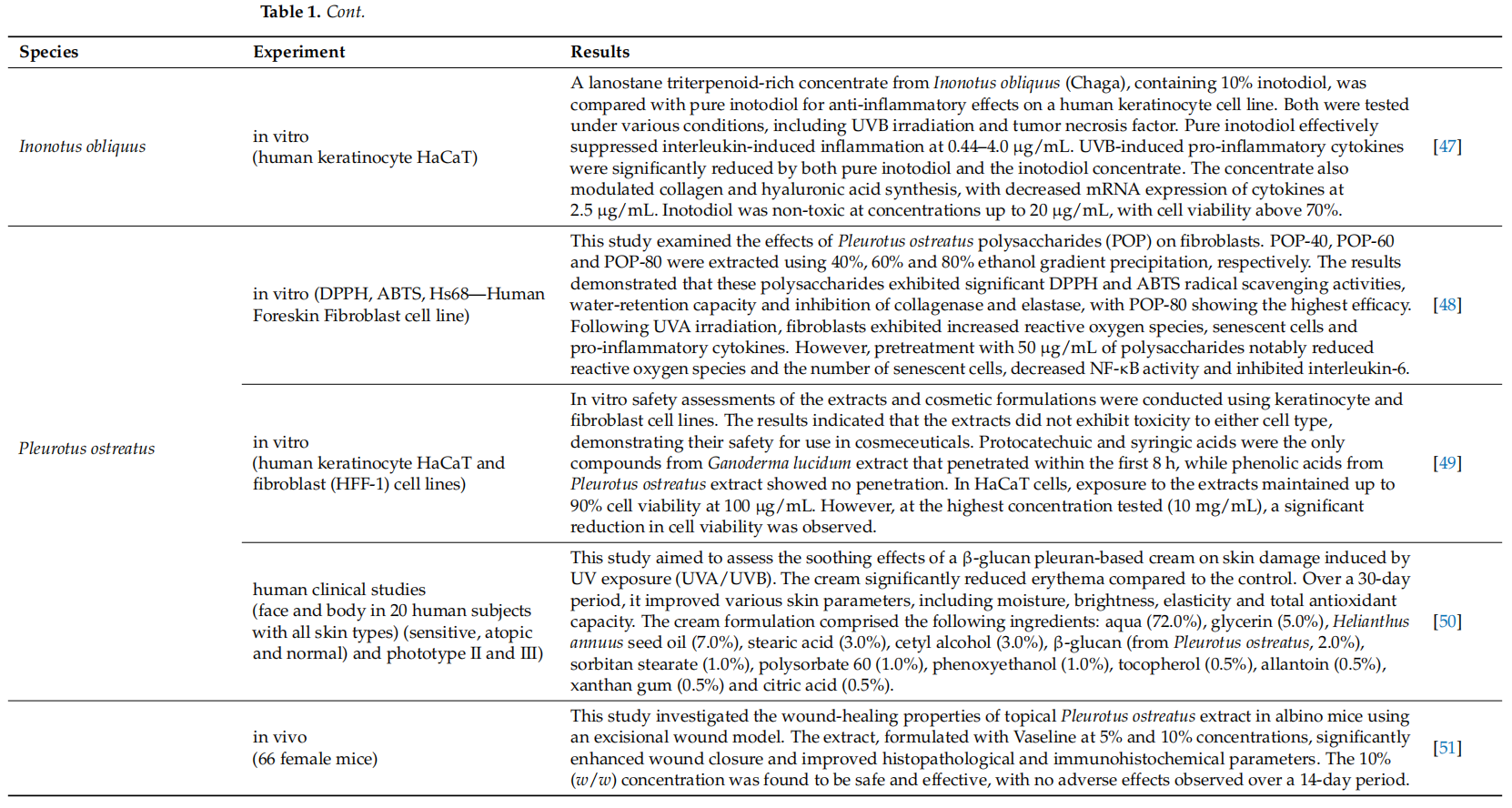
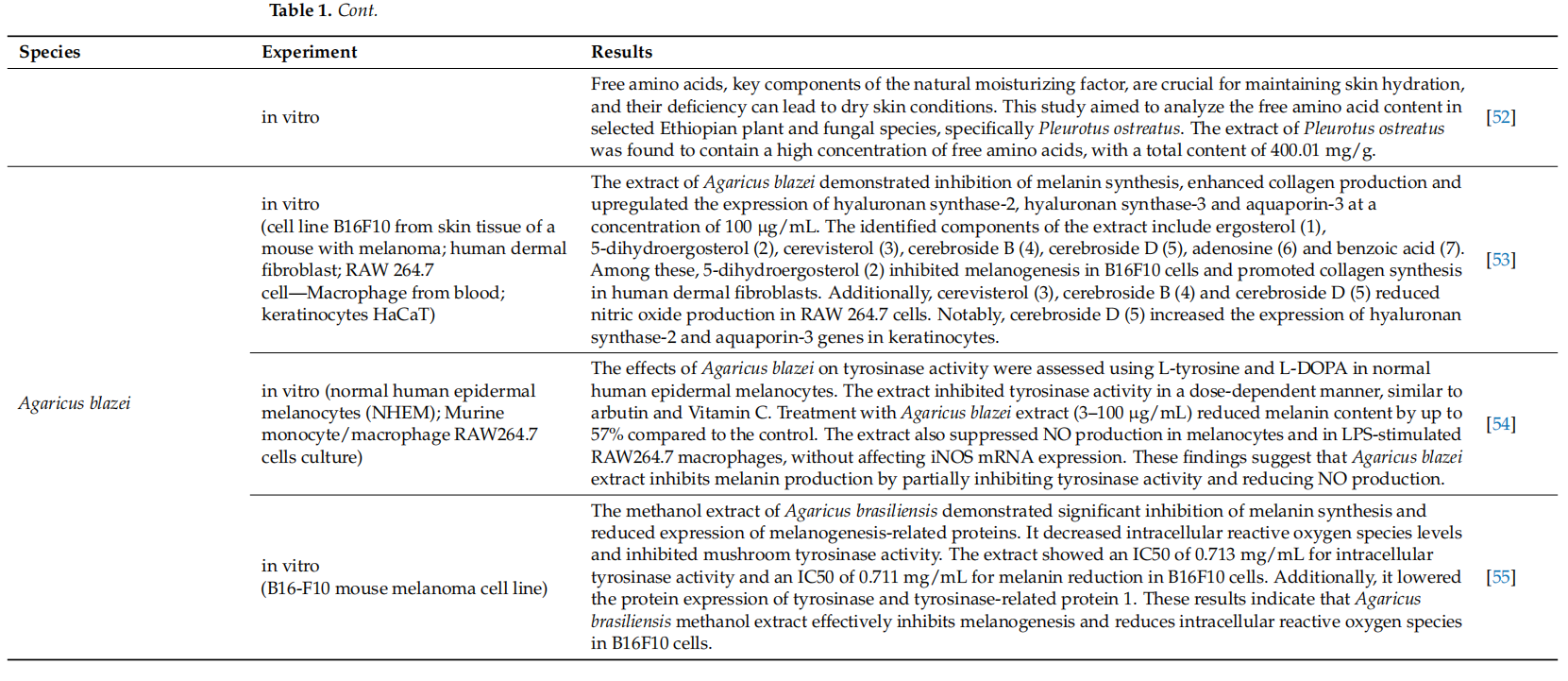
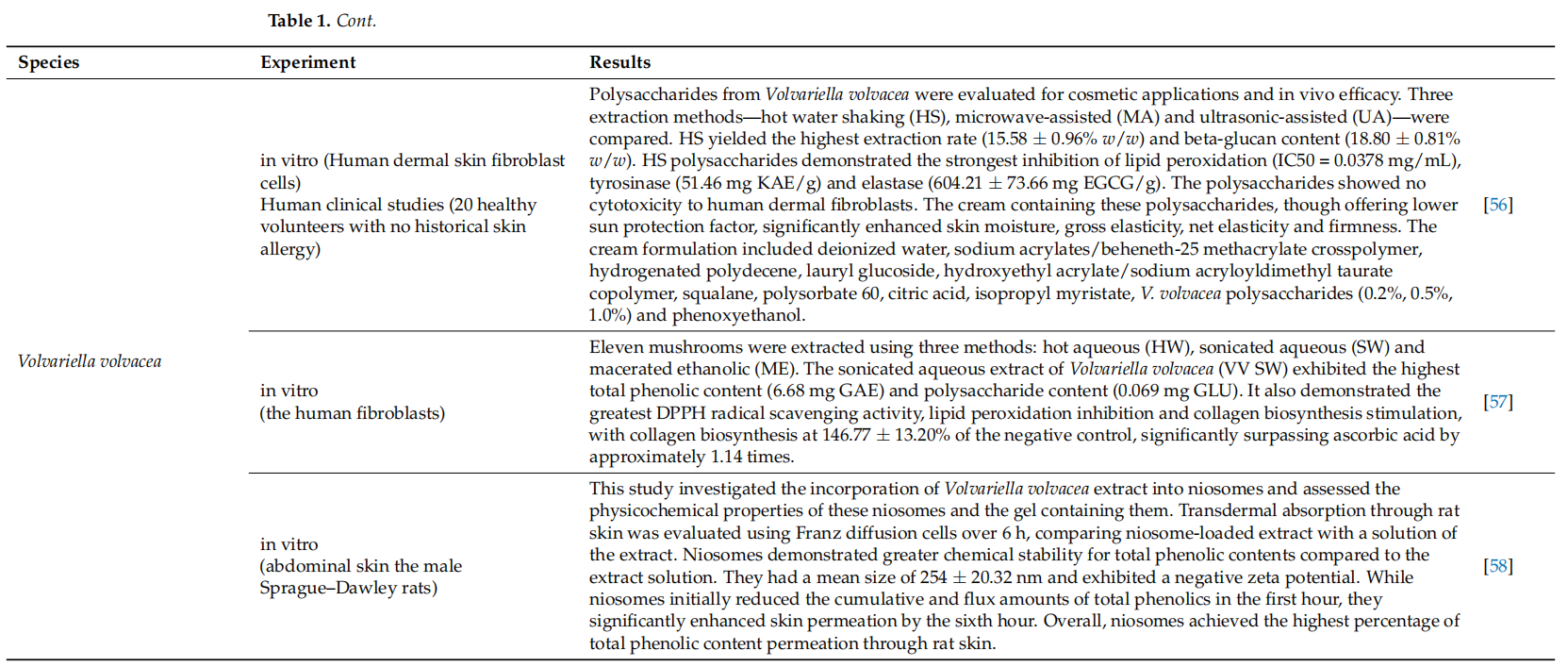
This article is excerpted from the Nutrients 2024, 16, 2810 by Wound World.

- 星期一, 09 6月 2025
Macrofungal Extracts as a Source of Bioactive Compounds for Cosmetical Anti-Aging Therapy: A Comprehensive Review(2-1)
Maja Paterska 1 , Bogusław Czerny 2,3 and Judyta Cielecka-Piontek 4,*
1 Department of Pharmacology and Phytochemistry, Institute of Natural Fibres and Medicinal Plants, Wojska Polskiego 71b, 60-630 Poznan, Poland; 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
2 Department of Stem Cells and Regenerative Medicine, Institute of Natural Fibres and Medicinal Plants, 62-064 Plewiska, Poland; 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
3 Department of General Pharmacology and Pharmacoeconomics, Pomeranian Medical University in Szczecin, 71-210 Szczecin, Poland
4 Department of Pharmacognosy and Biomaterials, Faculty of Pharmacy, Poznan University of Medical Sciences, Rokietnicka 3, 60-806 Poznan, Poland
* Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Citation: Paterska, M.; Czerny, B.;
Cielecka-Piontek, J. Macrofungal
Extracts as a Source of Bioactive
Compounds for Cosmetical
Anti-Aging Therapy: A
Comprehensive Review. Nutrients
2024, 16, 2810. https://doi.org/
10.3390/nu16162810
Academic Editors: Arrigo Cicero and
Akiko Kojima-Yuasa
Received: 26 June 2024
Revised: 21 August 2024
Accepted: 22 August 2024
Published: 22 August 2024
Abstract: For centuries, mushrooms have been used as a component of skincare formulations. Environmental stresses and a modern lifestyle expose the skin to accelerated aging. To slow down this process, natural anti-aging skincare ingredients are being sought. In this review, 52 scientific publications about the effects of chemical compounds extracted from the fruiting bodies of macrofungi on skin cells were selected. The effects of extracts from nine species that are tested for anti-aging effects have been described. According to available literature data, macrofungi contain many polysaccharides, phenolic compounds, polysaccharide peptides, free amino acids, sterols, proteins, glycosides, triterpenes, alkaloids, which can have an anti-aging effect on the skin by acting as antioxidants, photoprotective, skin whitening, moisturizing, anti-inflammatory and stabilizing collagen, elastin and hyaluronic acid levels in the skin.
Keywords: anti-aging; Trametes versicolor; Schizophyllum commune; Tremella fuciformis; Pleurotus ostreatus; Agaricus subrufescens; Volvariella volvacea; Ganoderma lucidum; Letinula edodes; Inonotus obliquus; mushrooms; macrofungi
