文献精选
Seyeon Oh 1,†, Suk Bae Seo 2,†, Gunpoong Kim 3 , Sosorburam Batsukh 1,4, Chul-Hyun Park 5 , Kuk Hui Son 5,* and Kyunghee Byun 1,4,6,*
1 Functional Cellular Networks Laboratory, Graduate School and Lee Gil Ya Cancer and Diabetes Institute, College of Medicine, Gachon University, Incheon 21999, Republic of Korea
2 SeoAh Song Dermatologic Clinic, Seoul 05557, Republic of Korea
3 VAIM Co., Ltd., Okcheon 29055, Republic of Korea
4 Department of Anatomy & Cell Biology, College of Medicine, Gachon University, Incheon 21936, Republic of Korea
5 Department of Thoracic and Cardiovascular Surgery, Gachon University Gil Medical Center, Gachon University, Incheon 21565, Republic of Korea
6 Department of Health Sciences and Technology, Gachon Advanced Institute for Health & Sciences and Technology (GAIHST), Gachon University, Incheon 21999, Republic of Korea
* Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (K.H.S.); 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (K.B.); Tel.: +82-32-460-3666 (K.H.S.); +82-32-899-6511 (K.B.)
† These authors contributed equally to this work.
Abstract: Poly-D,L-lactic acid (PDLLA) filler corrects soft tissue volume loss by increasing collagen synthesis in the dermis; however, the mechanism is not fully understood. Adipose-derived stem cells (ASCs) are known to attenuate the decrease in fibroblast collagen synthesis that occurs during aging, and nuclear factor (erythroid-derived 2)-like-2 factor (NRF2) increases ASCs survival by inducing M2 macrophage polarization and IL-10 expression. We evaluated the ability of PDLLA to induce collagen synthesis in fibroblasts by modulating macrophages and ASCs in a H2O2 -induced cellular senescence model and aged animal skin. PDLLA increased M2 polarization and NRF2 and IL-10 expression in senescence-induced macrophages. Conditioned media from senescent macrophages treated with PDLLA (PDLLA-CMMΦ) reduced senescence and increased proliferation and expression of transforming growth factor-β (TGF-β) and fibroblast growth factor (FGF) 2 in senescence-induced ASCs. Conditioned media from senescent ASCs treated with PDLLA-CMMΦ (PDLLA-CMASCs) increased the expression of collagen 1a1 and collagen 3a1 and reduced the expression of NF-κB and MMP2/3/9 in senescence-induced fibroblasts. Injection of PDLLA in aged animal skin resulted in increased expression of NRF2, IL-10, collagen 1a1, and collagen 3a1 and increased ASCs proliferation in aged animal skin. These results suggest that PDLLA increases collagen synthesis by modulating macrophages to increase NRF2 expression, which stimulates ASCs proliferation and secretion of TGF-β and FGF2. This leads to increased collagen synthesis, which can attenuate aging-induced soft tissue volume loss.
Keywords: aged skin; NRF2; macrophage; collagen; elastic fiber
Citation: Oh, S.; Seo, S.B.; Kim, G.; Batsukh, S.; Park, C.-H.; Son, K.H.; Byun, K. Poly-D,L-Lactic Acid Filler Increases Extracellular Matrix by Modulating Macrophages and Adipose-Derived Stem Cells in Aged Animal Skin. Antioxidants 2023, 12, 1204. https://doi.org/10.3390/ antiox12061204
Academic Editor: Alessandra Napolitano
Received: 14 April 2023
Revised: 28 May 2023
Accepted: 29 May 2023
Published: 1 June 2023
Copyright: © 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https:// creativecommons.org/licenses/by/ 4.0/).
胡 康1,张 伟2 ( 1广东冠昊生物医用材料开发有限公司,广东省广州市 510530;2冠昊生物科技股份有限公司,再生型医用植入器械国家工程实验室,广东省广州市 510530)
DOI:10.3969/j. issn.2095-4344.0650 ORCID: 0000-0002-7923-2706(胡康)
胡康,男,1992 年生,湖北省仙桃市人,汉族,2017年华南理工大学毕业,硕士,主要从事医用生物材料的研究与开发研究。
通讯作者:张伟,中级工程师,冠昊生物科技股份有限公司研发部,广东省广州市 510530
文题释义:
胶原蛋白:是生物高分子材料,为动物结缔组织的主要成分,是哺乳动物体内含量最多、分布最广的功能性蛋白,占蛋白质总量的 30%左右;具有良好的生物相容性、低免疫原性和组织可降解吸收性,在创面止血、愈合,缺损组织的填充、修复及重建,药物载体和组织工程等方面有广泛应用,是理想的医用生物材料。医用生物材料:是用来对生物体进行诊断、治疗、修复,或替换其病损组织、器官及增进其功能的材料,包括金属、陶瓷、高分子、复合材料等。
摘要
背景:胶原蛋白因具有低免疫原性,良好的生物相容性和生物降解性,在医用生物材料方面得到广泛应用。
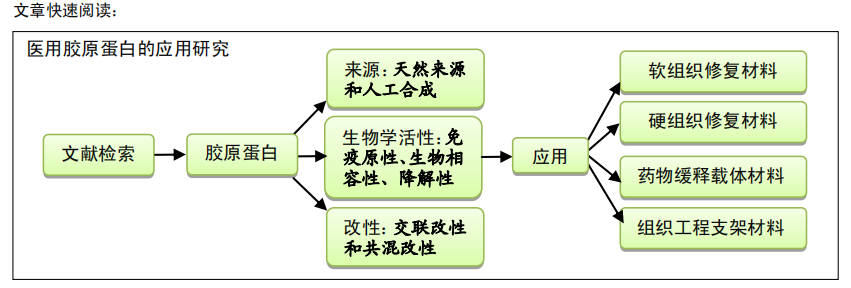
目的:综述近年来国内外胶原蛋白的来源、生物活性、改性及其在医用生物材料方面的应用进展。
方法:通过计算机检索 2010 至 2018 年 PubMed、Elsevier、Springerlink、中国知网等数据库发表的相关文章,英文检索词为“collagen,crosslinking,immunogenicity,biocompatibility,tissue engineering”,中文检索词为“胶原蛋白,交联,免疫原性,生物相容性,组织工程”。
结果与结论:胶原蛋白主要从动物肌腱、皮肤、尾巴等组织中提取获得的,具有良好生物相容性、低免疫原性和降解性等特性,但缺乏足够的机械强度。交联改性或与其他生物材料复合使用均可改善胶原蛋白的机械性能。目前,胶原蛋白已被广泛应用于止血剂与创面敷料、生物补片、骨修复材料、药物释放载体及作为组织工程支架等方面;临床使用显示,胶原蛋白对缺损组织的修复、再生及重建有着显著促进作用。
关键词:
胶原蛋白;免疫原性;生物相容性;生物降解性;交联;组织工程;生物材料
主题词:
胶原;交联试剂;组织工程
中图分类号:R459.9;R318
基金资助:
国家重点研究计划生物医用材料研发与组织器官修复替代重点专项(2016YFC1103202)
Collagen as a medical biomaterial in tissue repair, regeneration and reconstruction
Hu Kang1 , Zhang Wei2 ( 1Guangdong Guanhao Biomedical Materials Development Co., Ltd., Guangzhou 510530, Guangdong Province, China; 2Guanhao Biotech Co., Ltd., National Engineering Laboratory for Regenerative and Implantable Medical Devices, Guangzhou 510530, Guangdong Province, China)
Hu Kang, Master, Guangdong Guanhao Biomedical Materials Development Co., Ltd., Guangzhou 510530, Guangdong Province, China
Corresponding author:Zhang Wei, Mid-level engineer, Guanhao Biotech Co., Ltd., National Engineering Laboratory for Regenerative and Implantable Medical Devices, Guangzhou 510530, Guangdong Province, China
collagen. Nowadays, collagen is widely used as hemostatic and wound dressing, biological repair patches, bone repairing materials, drug
release carriers and tissue engineering scaffolds, which has a significant role in the clinical repair, regeneration and reconstruction of tissue
Subject headings: Collagen; Cross-Linking Reagents; Tissue Engineering
Funding: the Major Project of the National Key Research Plan for Biomedical Materials Development and Tissue Organ Repair, Replacement, No. 2016YFC1103202
叶滔 1,2,项琪 1,2,3,杨艳 1,2,4*,黄亚东 1,2,3,4*
1 暨南大学生命科学技术学院,广东 广州 510632
2 暨南大学生物医药研究院 广东省生物工程药物重点实验室,广东 广州 510632
3 广州暨南大学医药生物技术研究开发中心有限公司,广东 广州 510632
4 暨南大学-肽源化妆品创新研究院,广东 广州 511447
叶滔, 项琪, 杨艳, 黄亚东. 胶原蛋白的开发与应用研究进展[J]. 生物工程学报, 2023, 39(3): 942-960.
YE Tao, XIANG Qi, YANG Yan, HUANG Yadong. Research, development and application of collagen: a review[J]. Chinese Journal of Biotechnology, 2023, 39(3): 942-960.
摘 要:胶原蛋白(collagen)是一类哺乳动物细胞外基质中的主要结构蛋白,广泛地存在于皮肤、骨骼、肌肉等组织中,主要参与细胞的增殖、分化、迁移和信号传递等生理生化行为,对组织细胞等起着支撑、修复、保护的作用。由于胶原蛋白具有良好的生物学特性,其在组织工程、临床医学、食品工业、包装材料、化妆品、医学美容、生物材料以及医疗器械等方面都有着广泛的应用。本文综述了胶原蛋白的生物学特性及其在国内外生物工程研究开发中的研究进展,并对胶原蛋白未来开发的前景进行了展望。
关键词:胶原蛋白;生物工程;开发与应用;研究进展
Research, development and application of collagen: a review
YE Tao1,2, XIANG Qi1,2,3, YANG Yan1,2,4*, HUANG Yadong1,2,3,4*
1 College of Life Science and Technology, Jinan University, Guangzhou 510632, Guangdong, China
2 Guangdong Provincial Key Laboratory of Bioengineering Medicine, Institute of Biomedicine, Jinan University, Guangzhou 510632, Guangdong, China
3 Biopharmaceutical Research and Development Center of Jinan University, Guangzhou 510632, Guangdong, China
4 Jinan University & TYRAN Cosmetics Innovation Research Institute, Guangzhou 511447, Guangdong, China
Abstract: Collagen, which widely exists in skin, bone, muscle and other tissues, is a major structural protein in mammalian extracellular matrix. It participates in cell proliferation, differentiation, migration and signal transmission, plays an important role in tissue support and repair and exerts a protective effect. Collagen is widely used in tissue engineering, clinical medicine, food industry, packaging materials, cosmetics and medical beauty due to its good biological characteristics. This paper reviews the biological characteristics of collagen and its application in bioengineering research and development in recent years. Finally, we prospect the future application of collagen as a biomimetic material.
Keywords: collagen; biotechnology; development and application; research progress
资助项目:广东省重点领域研发计划(2022B1111080007);广东省基础与应用基础研究基金自然科学基金项目
(2021A1515012480);广州市重点领域研发计划专项(202103030003);广东省高校创新专项(2019KTSCX011)
This work was supported by the Guangdong Key Areas Research and Development Program (2022B1111080007), the Natural Science Foundation of Guangdong Basic and Applied Basic Research Foundation (2021A1515012480), the Guangzhou Key Areas Research and Development Program (202103030003), and the Guangdong University Innovation Project (2019KTSCX011).
*Corresponding authors. E-mail: YANG Yan, 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。; HUANG Yadong, 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Received: 2022-06-09; Accepted: 2022-10-08
刘龙飞1 ,王献珍2*
1 青海大学研究生院,青海 西宁
2 青海大学附属医院,青海 西宁
收稿日期:2022年3月22日;录用日期:2022年4月16日;发布日期:2022年4月26日
摘 要
由于感染的参与和严重程度,创面愈合一直是外科医生所关注的问题。因此,创面的愈合总是需要付出额外的努力来管理并随后从伤口部位去除瘢痕。创面处理的基本原则是保持创面清洁、无污染,减轻创面疼痛,减少创面渗出与水肿,预防创面损伤加重,防止创面感染以及促进创面早期愈合。多年以来,外科医师一直在寻找符合上述治疗原则的材料或药物。近年来,生物材料在慢性创面治疗中的作用已得到充分证实。其中一种生物材料是胶原蛋白,它被认为是大多数用于创面愈合配方的关键成分。在这里,我们主要介绍基于胶原蛋白的生物材料用于创面愈合的最新进展,以期为创面愈合的临床研究提供可靠的理论依据和治疗理念。
关键词
胶原蛋白,生物材料,创面愈合
Research Progress of Collagen Material on Wound Healing
Longfei Liu1, Xianzhen Wang2*
1 Graduate School of Qinghai University, Xining Qinghai
2 The Affiliated Hospital of Qinghai University, Xining Qinghai
Received: Mar. 22nd, 2022; accepted: Apr. 16th, 2022; published: Apr. 26th, 2022
Abstract
Because of the involvement and severity of infection, wound healing has always been a concern of surgeons. As a result, wound healing always requires extra effort to manage and then remove the scar from the wound site. The basic principle of wound treatment is to keep the wound clean and pollution-free, relieve the wound pain, reduce the wound exudation and edema, prevent the aggravation of wound injury, prevent wound infection and promote the early healing of wound. For years, surgeons have been searching for materials or drugs that fit these principles. In recent years, the role of biomaterials in the treatment of chronic wounds has been fully confirmed. One such biomaterial is collagen, which is considered a key ingredient in most wound healing formulations. Here, we mainly introduce the latest progress of collagen-based biomaterials for wound healing, in order to provide reliable theoretical basis and therapeutic concept for clinical research on wound healing.
Keywords
Collagen, Biomaterials, Wound Healing