文献精选
2.1 引言
挥发油是芳香植物中次生代谢形成的具有挥发性的天然混合物,具有强烈的香气。挥发油最初在中世纪由阿拉伯人通过水蒸气蒸馏获得。由于其具有杀菌、抗病毒、抑制微生物繁殖的特性,被用于食品保存、抗微生物、止痛、镇静、抗炎、解痉挛和局部麻醉。直至今天,这些性质并没有很大变化,只是在作用机制方面的研究更加深入,尤其是在抗微生物领域的研究。
在自然界,挥发油在保护植物方面有着重要的作用,如抗微生物、抗病毒、抗真菌、杀虫、降低食草动物的食欲。
挥发油为传统药典中的一个重要部分,外观为澄清液体,具有挥发性,通常密度小于水。所有的植物器官都能提取挥发油,如花蕾、花、叶、茎、小分支、种子果实、根、树干或树皮。提取挥发油的方法有多种,如超临界流体取、微波辅助萃取、水蒸气蒸馏、有机溶剂萃取。由于挥发油具有抗微生物和杀灭真菌的活性能够取代化学杀菌剂而在制药和食品领域得到越来越广泛的应用。在这种情况下,水蒸气蒸馏法和压榨法常被使用,如柑橘挥发油的提取。在香精领域,常常运用超临界流体萃取和水蒸气蒸馏法提取挥发油。提取的挥发油会因为植物的生长气候、土壤环境、植物器官、生长年龄和周期的不同而在挥发油含量、质量和化学成分上存在差异[1-2]。因此,为了获得成分基本一致的挥发油,通常选择植物的相同部位进行提取,且这些植物的土壤环境一样、生长气候一样、采摘季节一样。许多商品化的挥发油都要用气相色谱和质谱联用来分析成分。通过分析报告来保证挥发油的质量[3]
本章采用提取挥发油最常用的水蒸气蒸馏法,提取丁香花蕾油、香茅油、山苍子油,并用GC、GC-MS分析每种挥发油的成分,确定各种油的主要成分的相对含量。
2.2 材料和方法
2.2.1 主要原料及试剂
丁香花蕾:2009年采摘于中国广东,室温条件下自然风干;香茅:2009年采摘于中国广东,室温条件下自然风干;山苍子果实:2009年采摘于中国广东,室温条件下自然风干;无水硫酸钠(国药集团化学试剂有限公司);正构烷烃C8~C40(北京百灵威科技有限公司)。
2.2.2 主要仪器
气质联用仪(ThermoTrace GC/Ultra-DSQI );油水分离器(武汉大学科教仪器厂);气相色谱仪(Thermo Trace GC ULTRA);密度折光联用仪(Antonpaar股份有限公司);电热套(巩义市予华仪器有限公司)。
2.2.3 挥发油提取的单因素条件实验
山苍子挥发油提取单因素条件实验:选择优质的山苍子,提取的粒径选择未粉碎、粉碎至20目、粉碎至40目、粉碎至60目、粉碎至80目五个水平;浸泡时间分别采用0小时、2 小时、4 小时、6 小时、8 小时、10 小时和 12小时七个水平;料液比 1:4、1:6、1:8、1:10、1:12、1:14六个水平;提取时间为2小时、4小时、6 小时、8小时、10小时五个水平。分别进行单因素实验
丁香花蕾挥发油提取单因素条件实验:选择优质的丁香花蕾,提取的粒径选择未粉碎、粉碎至 20目、粉碎至40目、粉碎至60目、粉碎至80目五个水平;浸泡时间采用0小时、2 小时、4 小时、6 小时、8 小时、10 小时、12 小时七个水平;料液比 1:4、1:6、1:8、1:10、1:12、1:14 六个水平;提取时间为 2小时、4 小时、6 小时、8 小时、10 小时五个水平。分别进行单因素实验。
香茅叶挥发油提取单因素条件实验:选择优质的香茅叶,提取的粒径选择整叶、剪碎、粉碎至20目、粉碎至40目、粉碎至60目5个水平;浸泡时间采用0小时、2 小时、4 小时、6 小时、8 小时五个水平;料液比 1:4、1:6、1:8、1:10、1:12、1:14 六个水平;提取时间为 2 小时、4 小时、6 小时、8 小时、10小时五个水平。分别进行单因素实验。
挥发油得率(%)=挥发油质量(g)/提取原料质量(g)x100%
2.2.4 最优条件下水蒸气蒸馏法提取挥发油
三种植物挥发油的提取如文献报道[4.5],只做了少量的修改,具体如下所述:山苍子油:取山苍子果300克粉碎,过筛,放入挥发油提取装置,加入10倍质量的1%的氯化钠溶液,浸泡8小时后,水中蒸馏6小时,油水分离器中收集山苍子油。向山苍子油中加入适量的无水硫酸钠,静置2小时,过滤,得到的挥发油称重,然后在 4℃ 冷藏柜中密封避光保存待用。
丁香花蕾油:取丁香花蕾300克粉碎,过,放入挥发油提取装置,加入12倍质量的1%的氯化钠溶液,浸泡6小时后,水中蒸馏6小时,油水分离器中收集丁香花蕾油。向丁香花蕾油中加入适量的无水硫酸钠,静置2小时,过滤,得到的挥发油称重,然后在4℃冷藏柜中密封避光保存待用。
香茅油:取香茅叶300克粉碎,过,放入挥发油提取装置,加入8倍质量的1%的氯化钠溶液,浸泡4小时后,水中蒸馏4小时,油水分离器中收集香茅油。向香茅油中加入适量的无水硫酸钠,静置2小时,过滤,得到的挥发油称重,然后在4℃冷藏柜中密封避光保存待用。
2.2.5 挥发油成分分析
GC-MS 分析条件:
毛细管柱:HP5-MS(30mx0.25mmi.d.x0.25 um d.f);进样口温度:250℃;升温程序:起始柱温50℃ ,保持2min,5℃min 升温至250℃,保持15min;载气:He,流速 1.0mL/min;样品用无水乙醇稀释100倍;进样量:1μL,分流比 50:1;质谱接口温度:250℃:电离方式:EI:电离能量:70eV:离子源温度:250℃:质量扫描范围:41-350amu。采用Wiley和Nist谱检索、人工图谱解析以及查对质谱相关文献进行定性。正构烷烃C~C的混合标样用相同的分析条件分析来计算保留指数。
GC-FID 分析条件:
GC-FID分析条件与GC-MS相似,但是载气为氮气。挥发油各组分的相对含量在没有使用矫正因子的条件下通过GC-FID峰面积计算而来。
2.3 实验结果
2.3.1 水蒸气蒸馏法提取挥发油工艺优化
2.3.1.1 水蒸气蒸馏法提取山苍子挥发油工艺优化
2.3.1.1.1 不同提取粒径对山苍子挥发油得率的影响
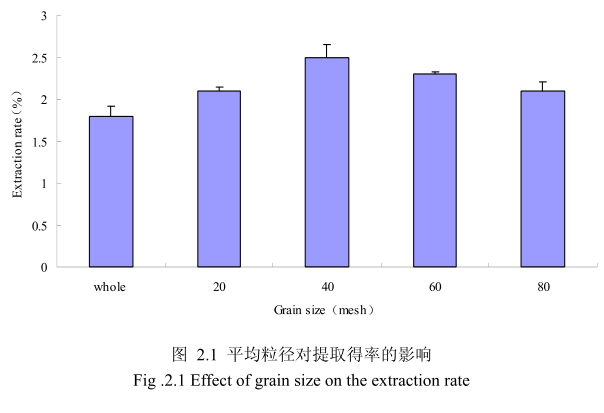
选择提取浸泡时间6小时、料液比1:8(质量比)、提取时间6小时、提取的粉碎粒径为未粉碎、粉碎至20目、粉碎至40目、粉碎至60目、粉碎至80目进行提取实验,实验结果如图2.1所示。从图中可以看出,当山苍子的提取粒径从未粉碎、粉碎至20目到粉碎至40目的过程中,山苍子油的得率随着粉碎粒径的变细而增大,当粉碎粒径为40目时,挥发油的得率最高。该过程中由于山苍子粉碎的越细,比表面积就越大,越有利于挥发油的浸出,所以挥发油的得率随着粉碎粒径的变小而增大。但是,当山苍子的粉碎粒径变为60目和80目时,山苍子油的得率反而下降。这可能是由于粉碎粒径的变小让颗粒比表面积增大的同时,颗粒自身的表面吸附作用增加,从而抑制了挥发油的扩散。同时,挥发油具有较强的挥发性,当粉碎粒径过细时,粉碎过程中会有少量的挥发油挥发损失掉,从而降低了挥发油的最终得率。因此,从本实验可以看出,山苍子的提取平均粒径控制在40目时挥发油的得率最高。
2.3.1.1.2 不同浸泡时间对山苍子挥发油得率的影响
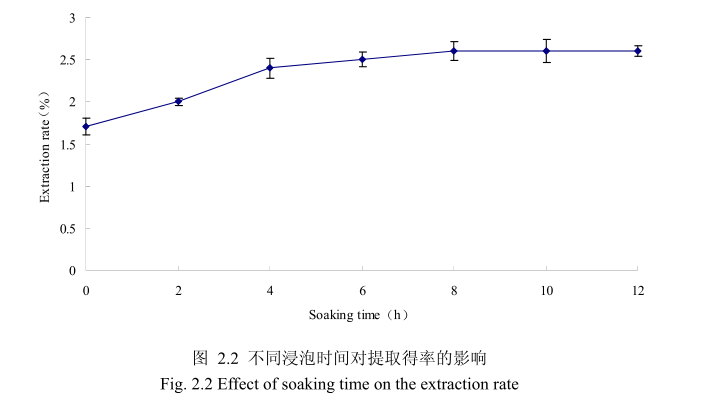
选择提取粒径为40目、料液比1:8(质量比)、提取时间6小时、提取的浸泡时间为0小时、2 小时、4 小时、6 小时、8 小时、10 小时、12 小时进行提取实验,从上图2.2可以看出,浸泡时间在0到8小时时间范围内,山苍子挥发油提取率随着浸泡时间的延长而增大。当浸泡时间为8小时,挥发油的得率达到较大值,随着浸泡时间的进一步延长,挥发油的得率几乎没有变化。造成这种现象的原因可能是由于浸泡过程可以使植物的细胞间隙增大,细胞组织充分膨胀,从而加速细胞内外的液体交换与平衡。由于山苍子质地较为坚硬,吸水性较差,因此需要浸泡较长时间才能让细胞组织充分膨胀。但是当浸泡达到一定时间后,细胞内外液体交换已经达到平衡,所以浸泡时间的进一步延长并不能改变精油的提取率。因此,选择浸泡时间为8小时时提取效率最高。
2.3.1.1.3 不同料液比对山苍子挥发油得率的影响
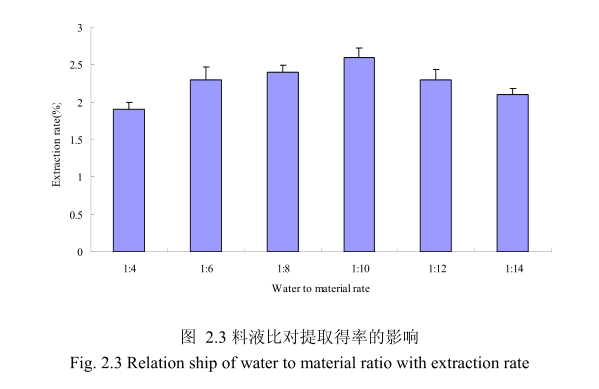
选择提取粒径40目,浸泡时间8小时,提取时间6小时,料液比为 1:4、1:6、1:8、1:10、1:12、1:14进行单因素实验。实验结果如图 2.3 所示,从图中可以发现,料液比从 1:4变化到1:10的过程中山苍子油的得率逐渐增加,料液比为1:10时山苍子油的得率最大。得率增加的原因可能是由于水的增多使山苍子中的山苍子油与水接触面处的浓度差变大,有利于山苍子油从组织中扩散出来。但当料液比从1:10 变化到 1:14 的过程中山苍子油的得率反而逐渐减少。可能由于水的增加,造成挥发油在水中的损耗增加,但是水量增加到一定程度对丁香花蕾油的扩散作用的影响已经不大,所以挥发油的得率降低。因此,当料液比为1:10时山苍子油的得率最高。
2.3.1.1.4 不同提取时间对山苍子挥发油得率的影响
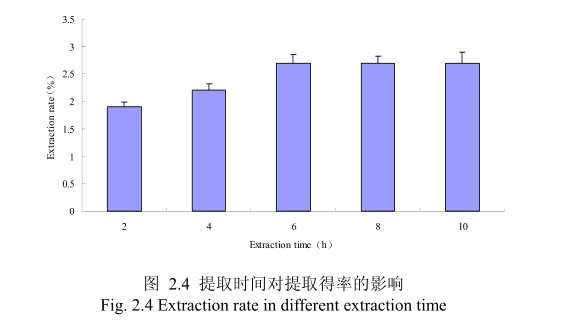
选择提取粒径为40目、料液比1:10(质量比)、浸泡时间8小时、提取时间为2小时、4 小时、6 小时、8小时、10小时进行提取实验,从图 2.4 中可以看出随着提取时间的不断延长,山苍子油的得率显著提高,当提取时间达到6小时时,山苍子油的得率达到较大值,随着提取时间的进一步延长,山苍子油的得率并没有显著的变化。所以可以推测,当山苍子提取到6小时时,体系的渗透压达到平衡,提取率趋于恒定,随着加热时间的延长,挥发油的提取效率并不能提高。
2.3.1.2 水蒸气蒸馏法提取丁香花蕾挥发油工艺优化
2.3.1.2.1 不同提取粒径对丁香花蕾挥发油得率的影响
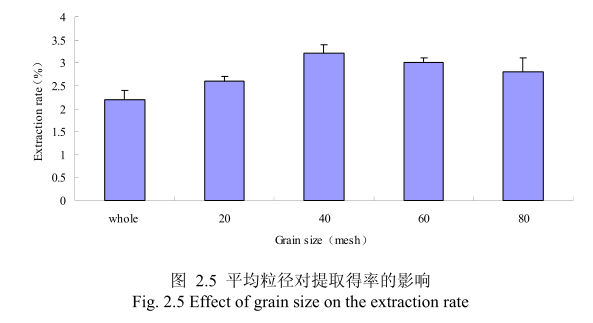
选择提取浸泡时间6小时、料液比1:8(质量比)、提取时间6小时、丁香花蕾的粉碎粒径分别为未粉碎、20目、40目、60目、80 目时进行提取实验,实验结果如图2.5所示。从图中可以看出,当丁香花蕾的提取粒径从未粉碎、粉碎至20目到粉碎至40目的过程中,丁香花蕾油的得率随着粒径的变细而增大,当粉碎粒径为 40目时,挥发油的得率最高。该过程中由于丁香花蕾粉碎的越细,比表面积就越大,越有利于挥发油的浸出,所以挥发油的得率随着粉碎粒径的变小而增大。但是,当丁香花蕾的粉碎粒径变为60目和80目时,丁香花蕾挥发油的得率反而下降。这可能是由于粉碎粒径的变小让颗粒比表面积增大的同时,颗粒自身的表面吸附作用增加,从而抑制了挥发油的扩散。同时,挥发油具有较强的挥发性当粉碎粒径过细时,粉碎过程中会有少量的挥发油挥发损失掉,从而降低了挥发油的最终得率。因此,从本实验可以看出,丁香花蕾的提取平均粒径控制在40目时挥发油的得率最高。
2.3.1.2.2 不同浸泡时间对丁香花蕾挥发油得率的影响
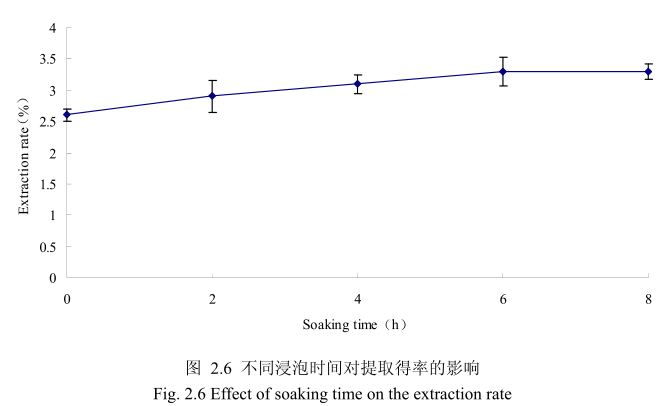
选择丁香花蕾粒径为40目、料液比1:8(质量比)、提取时间6小时。提取的浸泡时间分别为0小时、2小时、4 小时、6小时、8 小时进行提取实验,从图 2.6可以看出,浸泡时间在0到6小时时间范围内,丁香花蕾挥发油提取率随着浸泡时间的延长而增大。当浸泡时间为6小时时,挥发油的得率达到较大值,随着浸泡时间的进一步延长,挥发油的得率几乎没有变化。造成这种现象的原因可能是由于浸泡过程可以使植物的细胞间隙增大,细胞组织充分膨胀,从而加速细胞内外的液体交换与平衡。但是当浸泡达到一定时间后,细胞内外液体交换已经达到平衡,所以浸泡时间的进一步延长并不能改变挥发油的提取率。因此,选择浸泡时间为6小时时提取效率最高。
2.3.1.2.3 不同料液比对丁香花蕾挥发油得率的影响
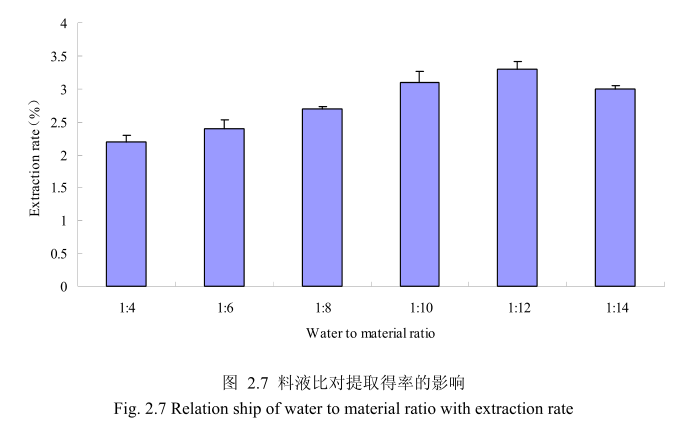
选择丁香花蕾粒径40目,浸泡时间6小时,提取时间6小时,料液比为1:4、1:6、1:8、1:10、1:12、1:14进行单因素实验。实验结果如图 2.7 所示,从图中可以发现,料液比从1:4变化到1:12的过程中丁香花蕾油的得率逐渐增加,料液比为1:12时丁香花蕾油的得率最大。得率增加的原因可能是由于水的增多使丁香花蕾中的丁香花蕾油与水接触面处的浓度差变大,有利于丁香花蕾油从组织中扩散出来。但当料液比从1:12变化到1:14的过程中,丁香花蕾油的得率反而逐渐减少。可能由于水的增加,造成挥发油在水中的损耗增加,但是水量增加到一定程度对了香花蕾油的扩散作用的影响已经不大,所以挥发油的得率降低。因此,当料液比为1:12时丁香花蕾油的得率最高。
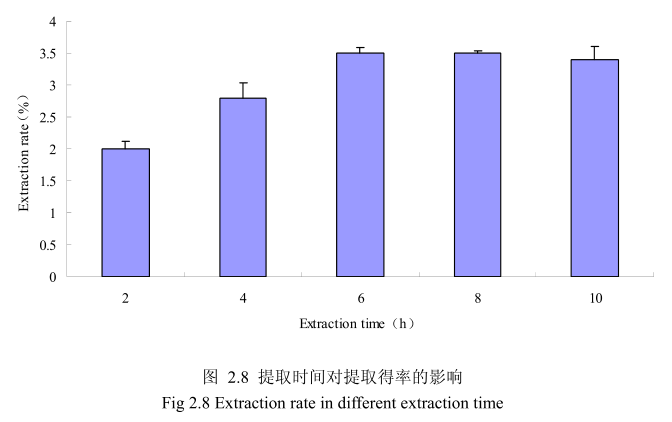
2.3.1.2.4 不同提取时间对丁香花蕾挥发油得率的影响
选择丁香花蕾粒径为40目、料液比1:12(质量比)、浸泡时间6小时、提取时间为2小时、4 小时、6小时、8小时、10 小时进行提取实验,从图2.8中可以看出随着提取时间的不断延长,丁香花蕾挥发油的得率显著提高,当提取时间达到6小时时,丁香花蕾挥发油的得率达到较大值,随着提取时间的进一步延长,丁香花蕾挥发油的得率并没有显著的变化。所以可以推测,当丁香花蕾提取到6时时体系的渗透压达到平衡,提取率趋于恒定,随着加热时间的延长,挥发油的提取效率并不能提高。
2.3.1.3 水蒸气蒸馏法提取香茅叶挥发油工艺优化
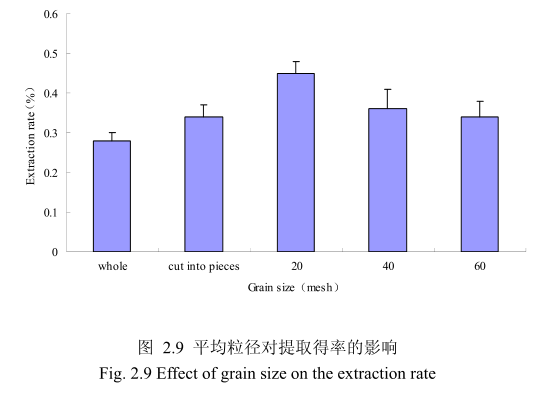
2.3.1.3.1 不同提取粒径对香茅叶挥发油得率的影响
不同提取粒径对香茅叶挥发油的提取得率有一定的影响。选择提取浸泡时间6小时、料液比 1:10(质量比)、提取时间6小时、提取的粉碎粒径为整叶、剪碎、粉碎至20目、粉碎至40目、粉碎至60目进行提取实验,实验结果如图2.9所示。从图中可以看出,当香茅叶的提取粒径从整叶、剪碎到粉碎至 20目的过程中,香茅油的得率随着粉碎粒径的变细而增大,当粉碎粒径为20目时,挥发油的得率最高。该过程中由于香茅叶粉碎的越细,比表面积就越大,越有利于挥发油的浸出,所以挥发油的得率随着粉碎粒径的变小而增大。但是,当香茅叶的粉碎粒径变为40目和60目时,香茅挥发油的得率反而下降。这可能是由于粉碎粒径的变小让颗粒比表面积增大的同时,颗粒自身的表面吸附作用增加,从而抑制了挥发油的扩散。同时,挥发油具有较强的挥发性,当粉碎粒径过细时,粉碎过程中会有少量的挥发油挥发损失掉,从而降低了挥发油的最终得率。因此,从本实验可以看出,香茅叶提取平均粒径控制在20目时挥发油的得率最高。
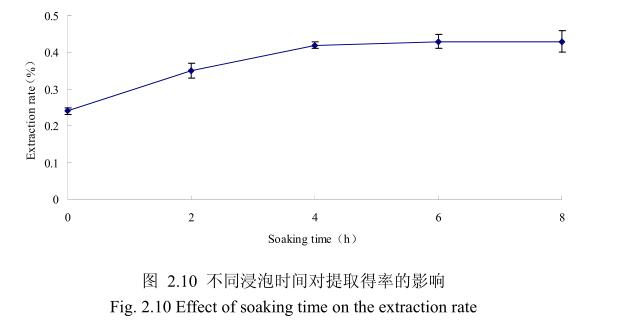
2.3.1.3.2 不同浸泡时间对香茅叶挥发油得率的影响
选择香茅叶粒径为20目、料液比1:10(质量比)、提取时间6小时、提取的浸泡时间分别为0小时、2小时、4 小时、6 小时、8 小时进行提取实验。从图2.10可以看出,在0到4时时间范围内,香茅叶挥发油提取率随着浸泡时间的延长而增大,在4小时时,挥发油的得率达到较大值,随着浸泡时间的进步延长,挥发油的得率几乎没有变化。造成这种现象的原因可能是由于浸泡过程可以使植物的细胞间隙增大,细胞组织充分膨胀,从而加速细胞内外的液体交换与平衡。但是当浸泡达到一定时间后,细胞内外液体交换已经达到平衡,所以浸泡时间的进一步延长并不能明显改变挥发油的提取率。因此,选择浸泡时间为4小时,此时提取效率最高。
2.3.1.3.3 不同料液比对香茅叶挥发油得率的影响
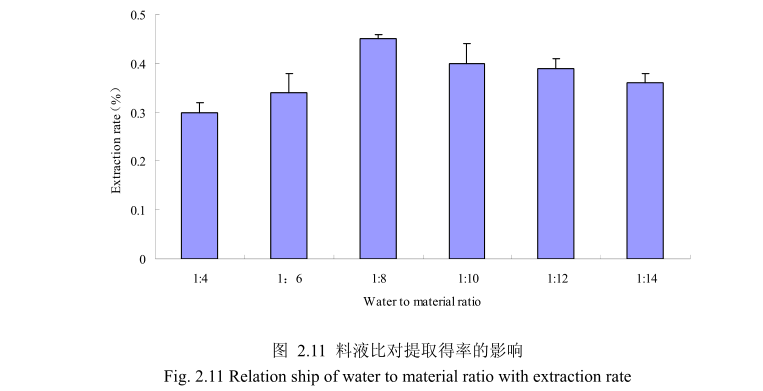
选择香茅叶粒径20目,浸泡时间4小时,提取时间6小时,料液比为1:4、1:6、1:8、1:10、1:12、1:14进行单因素实验。实验结果如图,从图中可以发现,料液比从1:4变化到1:8的过程中香茅叶油的得率逐渐增加,料液比为1:8时香茅叶油的得率最大。得率增加的原因可能是由于水的增多使香茅叶中的香茅油与水接触面处的浓度差变大,有利于香茅油的从叶片中扩散出来。但当料液比从1:8变化到1:14的过程中香茅油的得率反而逐渐减少。可能由于水的增加,造成挥发油在水中的损耗增加,但是水量增加到一定程度对香茅油的扩散作用的影响已经不大,所以挥发油的得率降低。因此,当料液比为1:8时香茅油的得率最高。
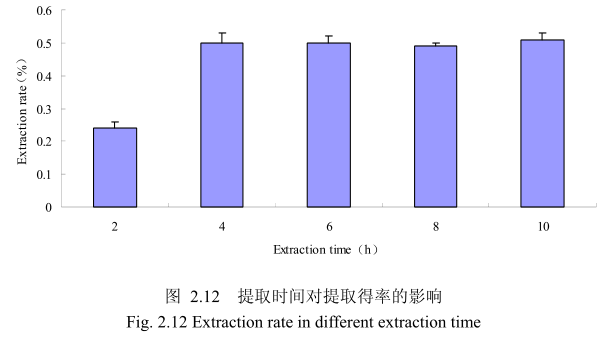
2.3.1.3.4 不同提取时间对香茅叶挥发油得率的影响
选择香茅叶粒径为20目、料液比1:8(质量比)、浸泡时间4小时、提取时间分别为 2小时、4 小时、6 小时、8 小时、10 小时进行提取实验,从图 2.12中可以看出随着提取时间的不断延长,香茅叶油的得率不断提高,当提取时间达到4小时时,香茅叶油的得率达到较大值,随着提取时间的进一步延长,香茅油的得率并没有显著的变化。所以可以推测,当香茅叶提取到4小时时,体系的渗透压达到平衡,提取率趋于恒定,随着加热时间的延长,挥发油的提取效率并不能提高。因此,当提取时间为4小时时,香茅油得率最高。
2.3.2 三种植物挥发油的物理指标
(1)丁香花蕾油:得率3.5%,澄清淡黄色液体,辛香及丁香酚的特征香气;相对密度 1.045(20/20℃);折光指数 1.5290(20℃)。
(2)山苍子油:得率2.7%,澄清淡黄色液体;感官特征:具有清鲜、甜的果香,类似柠檬油的香气;相对密度0.889(20/20℃);折光指数1.482(20℃)。
(3)香茅油:得率0.5%,澄清淡黄色液体;感官特征:具有轻快、新鲜的清甜果香,有成熟柠檬果皮的香气;相对密度0.889(20/20℃);折光指数 1.486(20℃)。
2.3.3 三种植物挥发油化学成分分析
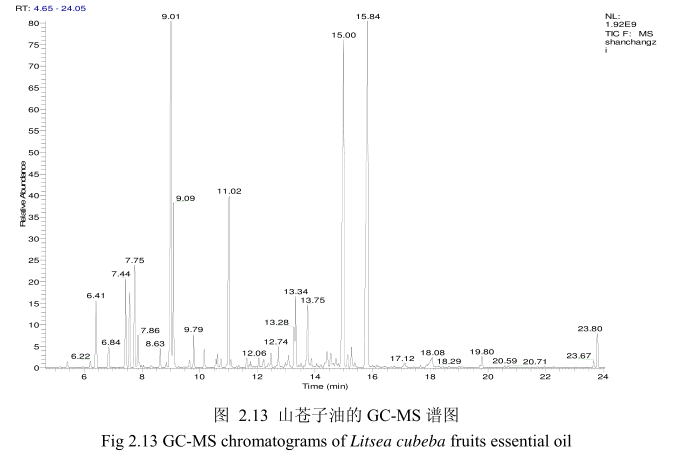
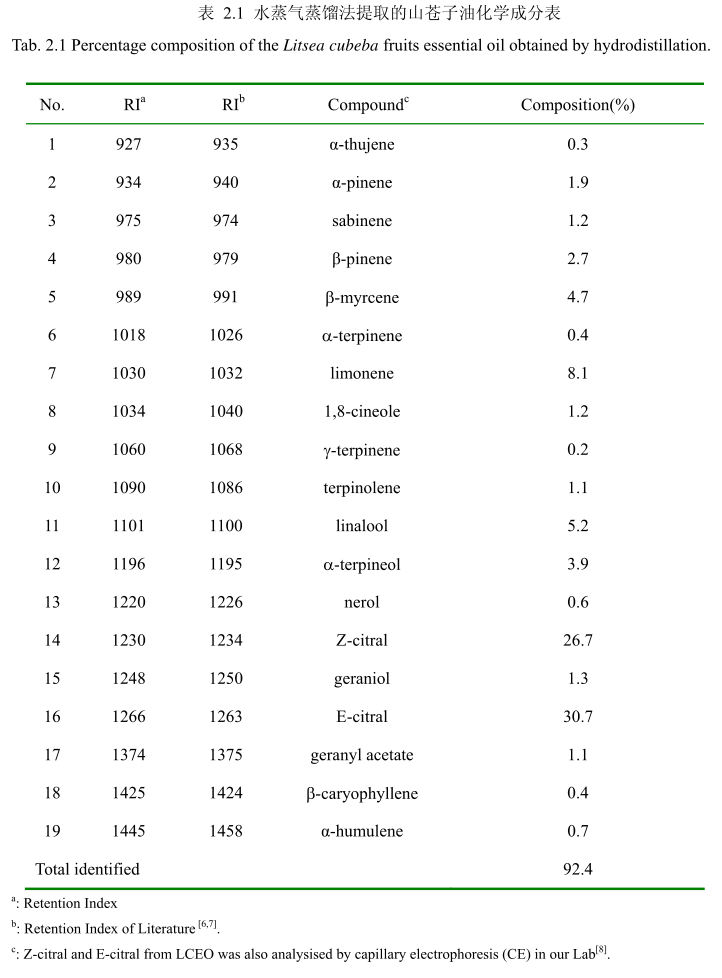
2.3.3.1 山苍子油的化学成分
将最优提取条件下提取的山苍子油进行GC-MS分析。图2.13是山苍子油的GC-MS 图谱。从图2.13可以看出,山苍子油的化学成分较多,其中大多成分集中在保留时间5.0-25分钟之间。通过和标准品或质谱数据库数据比对,鉴定出19种化学成分,占总油含量的92.4%。表2.1为山苍子油成分和含量统计表。从表2.1可看出,广东产的山苍子果挥发油中相对含量较高的成分有E-柠醛(30.7%);Z-柠檬醛(26.7%);柠檬烯(8.1%);芳樟醇(5.2%);B-月桂烯(4.7%);a-松油醇(3.9%);B-蒎烯(2.7%);a-蒎烯(1.9%);香叶醇(1.3%);1.8-桉叶素(1.2%)等。
2.3.3.2 丁香花蕾油的化学成分
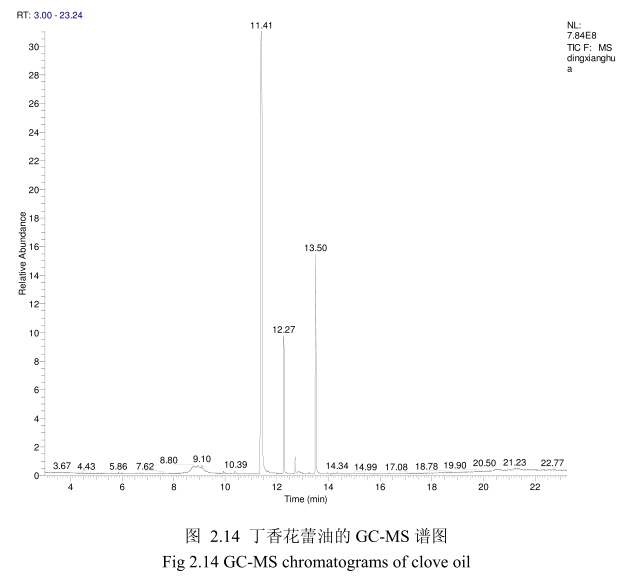
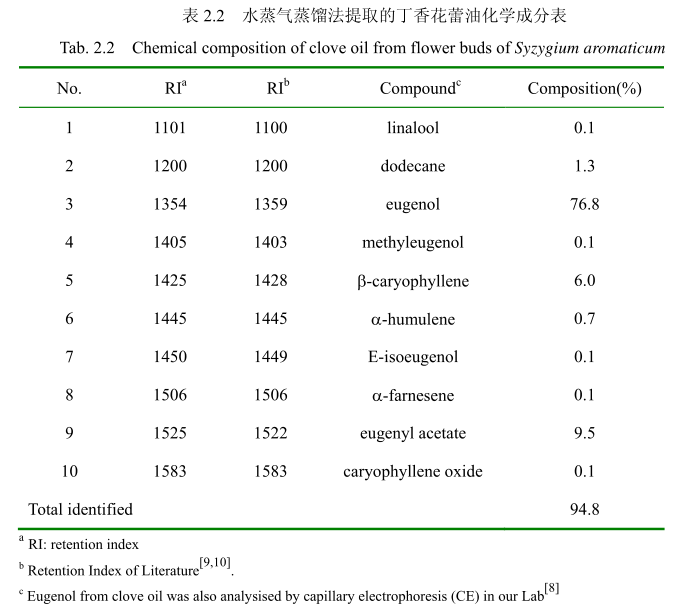
将最优提取条件下提取的丁香花蕾油通过GC-MS分析。图2.14是丁香花蕾油的GC-MS 图谱。从图2.14可以看出,丁香花蕾油的化学成分大多集中在保留时间 3.5-25分钟之间。通过和标准品或质谱数据库数据比对,鉴定出10种化学成分,占总油含量的94.8%。表2.2为鉴定出的丁香花蕾油成分和含量。从表2.2可看出,广东产的丁香花蕾油中相对含量较高的成分有丁香酚(76.8%)、乙酸丁香酯 (9.5%)、B-石竹烯(6.0%)、E-3-十二烯(1.9%)、2-1-十二烯(1.3%)等。
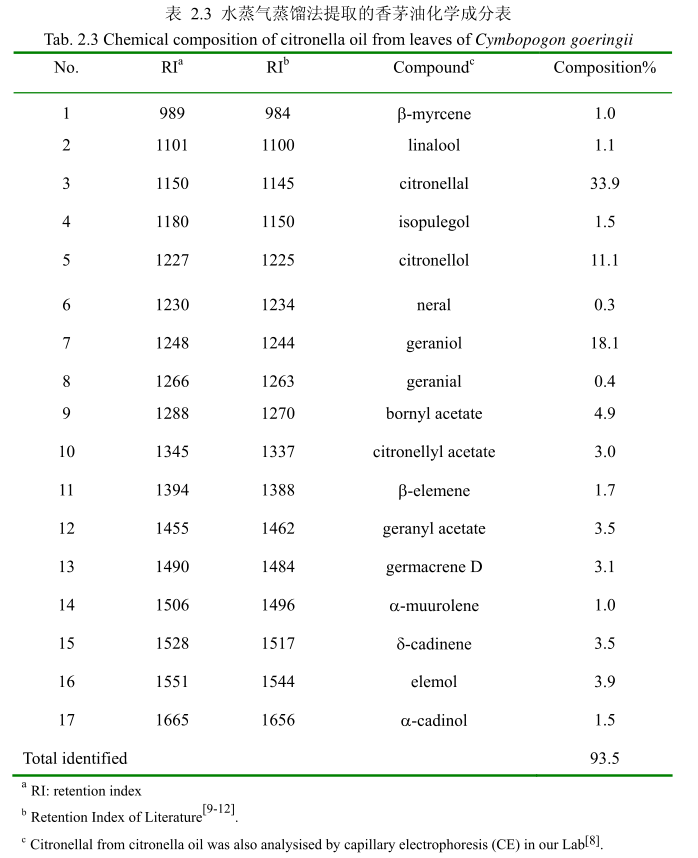
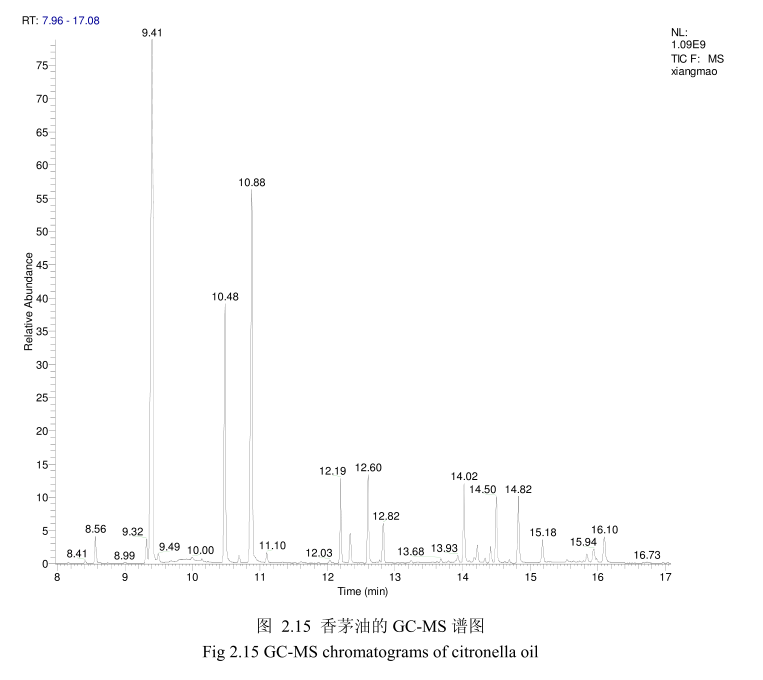
2.3.3.3.香茅油化学成分
将最优提取条件下提取的香茅油通过GC-MS分析。图2.15是香茅油GC-MS图谱。从图2.15可以看出,香茅油的化学成分大多集中在保留时间6.0-17分钟之间。通过和标准品或质谱数据库数据比对,鉴定出17种化学成分,占总油含量的93.5%。表2.3为鉴定出的香茅油成分及含量。从表2.3可看出,其相对含量较高的成分为香茅醛(33.9%)、香叶醇(18.1%)和香茅醇(11.1%)等。
2.4 讨论
挥发油是一种成分非常复杂的天然混合物,通常含有20-60种成分,并且其含量差异很大。挥发油通常含有两种或三种主要特征成分,每种的含量可达20%-70%,而有些成分的含量非常少。通常情况下,挥发油的主要成分决定了挥发油的生物活性。挥发油的成分包含两类[13-16]。其中主要的一类由萜烯类和萜类化合物组成,另外一类由芳香族和脂肪族化合物组成,都属于小分子化合物。
萜类化合物是植物次生代谢产物,在自然界分布广泛,由异戊二烯单元组成的化合物及其衍生物,按照碳原子的数目可以分为单萜、倍半萜、二萜、三萜和多萜等。由于萜类化合物分子中具有不同的碳环数,因此又可分为链萜、单环萜、双环萜和三环萜等[17]。单萜由两个异戊二烯单元组成,是挥发油中最有代表性的分子,占挥发油组分的 90%,包含:桂叶烯、罗勒、萜品烯、水芹烯、香叶醇、芳樟醇香茅醇,、熏衣草醇、香橙醇、薄荷醇、松油醇、龙脑、小茴香醇、香叶醛、橙花醛香茅醛、薄荷酮、香芹酮、薄荷酮、胡椒酮、乙酸芳樟酯、乙酸异冰片酯、桉油素麝香草酚、香芹酚等。当分子具有旋光性,两种对映异构体常常存在于不同的植物中。
芳香化合物衍生于苯基丙烷,其种类少于萜类。萜类和芳香化合物在植物中合成路径是分开的,但在某些植物中是共用一条合成路径。芳香类化合物包括:桂皮醛、肉桂醇、丁香酚、茴香脑、肉豆蔻醚等
挥发油是一种混合物,其化学成分会因为植物物种、生长的地理环境、提取方法、采收时间等因素的差异而不同[18,19]。本章运用水蒸气蒸馏法提取的自然晾干的山苍子果实的挥发油呈淡黄色。GC-MS分析水蒸气蒸馏法提取的山苍子油鉴定出19种化学成分,占总油的92.4%。其主要成分柠檬醛的相对含量占57.4%,柠檬烯的含量占 8.1%,芳樟醇的含量为5.2%,B-月桂烯的相对含量为4.7%,a-松油醇的相对含量为3.9%,β-烯的相对含量为2.7%,α-蒎烯的相对含量为1.9%。本章运用 GC-MS 分析的山苍子油的主要化学成分与其它相关文献报道的山苍子油的主要化学成分基本一致[20,21],但是比例不同,从而证明天然挥发油含量的差异性[22]。例如,同一种类的山苍子油,其产地为美国,主要成分柠醛的相对含量为 85.7%,柠檬烯的相对含量为2.9%,芳樟醇的相对含量为1.7%。Wang等[23]研究的山苍子油中柠檬醛的含量为63.75%,柠檬烯的相对含量为7.38%,甲庚酮的相对含量为 3.54%,烯的相对含量为2.87%,4-伞花烃的含量为2.14%。
同样用GC-MS 分析产于中国广东的丁香花蕾油,鉴定出10种物质,占总油的 94.8%。主要成分丁香酚的相对含量为76.8%,乙酸丁香酯的相对含量为 9.5%,B-石竹烯的相对含量为6.0%。尽管其主要成分与其它文献报道的一致,但是其含量不一致。如产地为意大利的丁香花蕾油中丁香酚的相对含量为70.8%,B-石竹烯的相对含量为 24.9%,乙酸丁香酯的含量为4.2%。Moon 等[24]报道的丁香花蕾油中丁香酚的相对含量为76.8%,B-石竹烯的相对含量为17.4%,乙酸丁香酯的相对含量为 1.2%。
用GC-MS分析的香茅叶的挥发油鉴定出17种成分,占总油的93.5%。其中主要成分香茅醛的相对含量为33.9%、香叶醇的相对含量为18.1%、香茅醇的相对含量为11.1%。其主要成分与相关文献报道的香茅油的主要化学成分一致,但是其比例有一点差异。如中国云南产的香茅挥发油中主要成分香茅醛的含量为36.055%,香叶醇的含量为21.33%。
从本章分析的三种天然挥发油与其相关文献报道的结果相比较可以看出,尽管其主要化学成分一致,但是其含量有一定差异。而挥发油的化学成分及其含量决定了其生物活性,因此其挥发油的生物活性也可能存在较大差异。
2.5 本章小结
本章运用水蒸气蒸馏法萃取了产地中国广东的山苍子果实、丁香花蕾、香茅叶,获得挥发油的理化指标如下:
(1)山苍子油得率2.7%,澄清淡黄色液体;感官特征:具有清鲜、甜的果香,类似柠檬油的香气;相对密度0.889(20/20℃);折光指数1.482(20℃)。通过单因素实验,山苍子挥发油最佳提取工艺参数为山苍子粉碎至40目,浸泡时间8小时,料液比1:10,提取时间6小时。GC-MS分析山苍子油鉴定出19种化学成分,占总油的92.4%。其主要成分柠檬醛的相对含量占57.4%,柠烯的含量占8.1%,芳樟醇的含量为5.2%,B-月桂烯的相对含量为4.7%,a-松油醇的相对含量为3.9%,B-烯的相对含量为2.7%,a-的相对含量为1.9%。
(2)丁香花蕾油,得率3.5%,澄清淡黄色液体,辛香及丁香酚的特征香气;相对密度 1.045(20/20℃);折光指数15290(20℃)。通过单因素实验,丁香花蕾挥发油最佳提取工艺参数为丁香花蕾粉碎至40目,浸泡时间6小时,料液比1:12,提取时间6小时。用GC-MS 分析丁香花蕾油,鉴定出10种物质,占总油的94.8%。主要成分丁香酚的相对含量为76.8%,乙酸丁香酯的相对含量为9.5%,B-石竹烯的相对含量为6.0%。
(3)香茅油得率0.5%,澄清淡黄色液体;感官特征:具有轻快、新鲜的清甜果香,有成熟柠檬果皮的香气;相对密度0.889(20/20℃);折光指数 1.486(20℃)通过单因素实验,香茅叶挥发油最佳提取工艺参数为香茅粉碎至20目,浸泡时间4小时,料液比1:8,提取时间4小时。GC-MS 分析的香茅叶的挥发油鉴定出 17种成分,占总油的93.5%。其中主要成分香茅醛的相对含量为33.9%、香叶醇的相对含量为 18.1%、香茅醇的相对含量为11.1%。
2.6参考文献
[1] Masotti V, Juteau F, Bessie 're JM. Seasonal and phenological variations of the essential oil from the narrow endemic species Artemisia molinieri and its biological activities. Journal of Agricultural and Food Chemistry, 2003, 51:7115- -7121
[2] Jirovetz L, Buchbauer G, Stoilova I, et al. Chemical composition and antioxidant properties of clove leaf essential oil. Journal of Agricultural and Food Chemistry, 2006, 54(17):6303-6307
[3] Smith R, Cohen S, Doull J, et al. A procedure for the safety evaluation of natural flavor complexes used as ingredients in food: essential oils. Food and Chemical Toxicology, 2005, 43(3):345-363
[4]Huang B, Ban X, He J, et al. Comparative analysis of essential oil components and antioxidant activity of extracts of Nelumbo nucifera from various areas of China. Journal of Agricultural and Food Chemistry, 2009, 58(1):441-448
[5]Wang Q, Yang Y, Zhao X, et al. Chemical variation in the essential oil of Ephedra sinica from Northeastern China. Food Chemistry, 2006, 98( 1):52-58
[6] Wang HW, Liu YQ. Chemical composition and antibacterial activity of essential oils from different parts of Litsea cubeba. Chemistry & Biodiversity, 2010,7:229-235.
[7]Mockute D, Bernotiene G. The main citral-geraniol and carvacrol chemotypes of the essential oil of Thymus Pulegioides L. growing wild in Vilnius District (Lithuania). Journal of Agricultural and Food Chemistry,1999, 47: 3787-3790
[8]Huang XW, Yi L,Gao ZH, et al. Determination of seven active ingredients in three plant essential oils by using micellar electrokinetic chromatography. Analytical Letters, 2012,45, 2014-2015
[9]Jirovetz L, Buchbauer G, Stoilova I, et al. Chemical composition and antioxidant properties of clove leaf essential oil. Journal of Agricultural and Food Chemistry, 2006, 54, 6303-6307
[10] Kiran SR, Reddy AS, Devi PS,et al. Reddy, Insecticidal, antifeedant and oviposition deterrent effects of the essential oil and individual compounds from leaves of Chloroxylon swietenia DC. Pest Management Science, 2006, 62:1116-1121
[11] Lota ML, Serra DD, Tomi F,et al. Volatile components of peel and leaf oils of Lemon and Lime Species. Journal of Agricultural and Food Chemistry, 2002, 50:796-805
[12] Rajeswara R, Bhattacharya AK, Mallavarapu GR,et al. Yellowing and crinkling disease and its impact on the yield and composition of the essential oil of citronella (Cymbopogon winterianus Jowitt). Flavour Fragrance Jourmal, 2004, 19:344-350
[13]Da Silva EB, Matsuo AL, Figueiredo CR, et al. Chemical constituents and cytotoxic evaluation of essential oils from leaves of Porcelia macrocarpa(Annonaceae). Natural Product Communications, 2013, 8(2):277-279
[14]Betts TJ. Chemical characterisation of the different types of volatile oil constituents by various solute retention ratios with the use of conventional and novel commercial gas chromatographic stationary phases. Journal ofChromatography A, 2001, 936(1):33-46
[15]Setzer WN. Essential oils and anxiolytic aromatherapy. Natural Product Communications,2009,4(9): 1305-1316.
[16] Pichersky E, Noel JP, Dudareva N. Biosynthesis of plant voltiles: nature's diversity and ingenuity. Science Signaling, 2006, 311(5762):808-811
[17] 张长波,孙红霞,巩中军.植物萜类化合物的天然合成途径及其相关合酶.植物生理学通讯,2007,43(4) :779-785
[18] Lota ML, De Rocca Serra D, Tomi F, et al. Volatile components of peel and leaf oils of lemon and lime species. Journal of Agricultural and Food Chemitry, 2002, 50(4):796-805
[19] Lalko J, Api A. Investigation of the dermal sensitization potential of various essential oils in the local lymph node assay. Food and Chemical Toxicology, 2006, 44(5):739-746
[20] Gao Z, Xu H, Chen X, et al. Antioxidant status and mineral contents in tissues of rutin and baicalin fed rats. Life Sciences, 2003, 73(12):1599-1607
[21] Ho CL, Jie-Pinge O, Liu YC, et al. Compositions and in vitro anticancer activities of the leaf and fruit oils of Litsea cubeba from Taiwan. Natural Product
Communications, 2010, 5(4):617-620
[22] Liu ZL, Liu QR, Chu SS, et al. Insecticidal activity and chemical composition of the essential oils of Artemisia lavandulae folia and Artemisia sieversiana from China. Chemistry & Biodiversity, 2010, 7(8):2040-2045
[23] Wang H, Liu Y. Chemical composition and antibacterial activity of essential oils from different parts of Litsea cubeba. Chemistry & Biodiversity, 2010,
7(1):229-235
[24] Moon SE, Kim HY, Cha JD. Synergistic effect between clove oil and its major compounds and antibiotics against oral bacteria. Archives of Oral Biology, 2011 ,56(9):907-916
未完待续……
摘 要
随着大气层中臭氧的逐渐减少,地球表面的紫外线强度不断增加。高强度的紫外照射会引起皮肤色素的过度沉着和皮肤功能的紊乱。因此研发有效的祛斑、美白护肤品一直是化妆品领域的热门之一。近年来,出于安全性方面的考虑,人们更愿意接受源自天然中草药的美白护肤产品。中国是一个植物物种多样的国家,有许多药食同源的植物挥发油在民间被广泛地应用于护肤品,但其是否具有祛斑、美白的功能,却鲜有研究。本论文选取了三种各具独特功能的本土植物挥发油(丁香花蕾油、香茅油和山苍子油),通过系列实验,为判断其是否具有成为美白护肤品成分的潜能提供科学依据。
主要内容包含以下几个方面:
1、优化了提取山苍子油、丁香花蕾油和香茅油的提取工艺,并用气质联用技术鉴定了三种挥发油的主要成分。鉴定出山苍子油中的19种化学成分,占整个挥发油组分的 92.4%。主要成分有柠檬醛(57.4%),柠檬烯(8.1%),芳樟醇(5.2%),B-月桂烯(4.7%),α-松油醇(3.9%),β-蒎烯(2.7%)和a-蒎烯(1.9%);鉴定出丁香花蕾油中的 10种成分,占整个挥发油的94.8%。主要成分有丁香酚(76.8%),乙酸丁香酯(9.5%)和B-石竹烯(6.0%);鉴定出香茅油中的 17 种成分,占整个挥发油的 93.5%。主要成分有香茅醛(33.9%),香叶醇(18.1%),和香茅醇(11.1%)。
2、通过酪氨酸酶抑制试验来评价三种挥发油及其主要成分对酪氨酸酶的抑制效果。结果表明山苍子油和其主要成分柠檬醛对酪氨酸酶单酚酶和二酚酶活性有抑制能力,对酪氨酸酶二酚酶的抑制能力强于酪氨酸酶单酚酶,且动力学结果表明柠檬醛对酪氨酸酶是非竞争性抑制作用。丁香花蕾油和丁香酚对酪氨酸酶单酚酶具有一定的抑制作用,但是对酪氨酸酶二酚酶没有表现出任何抑制作用。而香茅油及其主要成分对酪氨酸酶没有抑制作用。
3、分别研究了山苍子油、香茅油、丁香花蕾油和其主要成分的抗氧化活性。
结果表明丁香花蕾油具有最强的自由基清除能力(超阴离子的ICo值为58g/mL;ABTS的ICso值为8.5μg/mL)和强的抑制脂质过氧化的能力;香茅油的自由基清除能力和抑制脂质过氧化的能力低于丁香花蕾油(超氧阴离子的ICso值为150 μg/mL;ABTS*的ICso值为 500μg/mL)。山苍子油的自由基清除能力最低(超氧阴离子的ICso值为10.2mg/mL;ABTS 的ICso值为 17.75 mg/mL)。
4、为了探讨山苍子油、丁香花蕾油和香茅油分别对 UV-TiO2-NO,体系导致的蛋白质氧化和酪氨酸硝化损伤的抑制作用,将牛血清蛋白作为模型蛋白进行体外试验,采用免疫印迹法测定牛血清白蛋白的氧化和酪氨酸硝化。结果表明丁香花蕾油、香茅油和山苍子油对UV-TiO,-NO,-催化的蛋白质氧化和酪氨酸硝化都有较强的抑制效果且呈剂量依耐性。
关键词:挥发油,酪氨酸酶,抗氧化,纳米二氧化钛,蛋白质氧化,蛋白质酪氨酸硝化
Abstract
Ultraviolet (UV) radiation on the surface of the earth is certainly increasing as a result of the depletion of stratospheric ozone. High-intensity or accumulated UV radiation provokes many hyperpigmentation disorders, which are of particular concern to women as well as men, In recent years, the study of traditional herbal medicines for skin-protecting and skin-lighting has become a hot spot in the cosmetics field, due to various safety concerns and interesting largely unexplored sources. In this dissertation. the main objective was to investigate the potential usage of clove oil , citronella oil and Litsea cubeba oil as natural sources of tyrosinase inhibitor, antioxidant, and protectionprotein against UVTiO,-NO2- induced protein oxidation and tyrosine nitration in jury The main results are as follows:
1. The clove oil, citronella oil and Litsea cubeba oil extracted by hydrodistillation, showed light yellow in color. The total of 10 compounds was identified by GC-MS in the clove oil, accounting for 94.8% of the total oil. The main components were eugenol(76.8%), followed by eugenyl acetate (9.5%) and β-caryophyllene (6.0%). Essential oil from Cymbopogon goeringii leaves was also analyzed by GC-MS, resulted in the identification of 17 compounds representing 93.5% of the oil. Citronellal (33.9%),geraniol (18.1%), and citronellol (11.1%) were the main compounds. GC-MS analyses of Litsea cubeba oil led to identification of 19 different compounds, accounting for 92.4%of the total oil. The main components were citral representing 57.4% of the total amount of oil extracted, follow by limonene(8.1%),linalool (5.2%),β-myrcene (4.7%),a-terpineol (3.9%),β-pinene(2.7%) and a-pinene(1.9%%).
2. Tyrosinase inhibitory assay was used to evaluate whether the three essential oilsand their main components possessed potential inhibitory effect on tyrosinase. The results show that Litsea cubeba oil and citral exhibited inhibitory effect on monophenolase and diphenolase activity of tyrosinase. The inhibitory effect of Litseacubeba oil and citral on diphenolase activity was stronger than monophenolase activity oftyrosinase. The inhibition pattern of mushroom tyrosinase by citral was determined byLineweaver-Burk polt analysis. The results demonstrated that citral was anoncompetition tyrosinase inhibitor, Clove oil and eugenol exhibited some inhibitoryeffect on monophenolase activity of` tyrosinase, but not show any inhibitory effect on diphenolase activity of tyrisinase. Citronella oil and their main components didn'texhibited any inhibitory effect.
3. In order to determine whether the three essential oils and their main components had antioxidant activity, ABTS cation radical scavenging assay, superoxide anion radicalscavenging assay and lipid peroxidation assay were carried out. Clove oil exhibited prominent radical scavenging activities (ICso: 58 μg/ mL for O2 and 8.5 ug/ mL for ABTS*) and strong inhibitory effect on lipid peroxidation, whilst citronella oil showedweaker antioxidative activities (ICso: 150 μg/ mL for O, and 500 μg/ mL for ABTS )and lipid peroxidation inhibitory efficiency. Litsea cubeba oil exhibited the lowest anti-oxidative activities (ICso: 17.75 mg/mL for ABTS , 10.2 mg/mL, for O, ).
4. In order to investigate inhibitory effects of essential oils to UV-TiO,-NOzinduced protein oxidation and protein tyrosine nitration injury, bovine serum albumin(BSA) were used as model protein, inhibition were followed by $DS-PAGE and Western blotting methods. The results showed that clove oil, citronella oil and Litsea cubeba oil exhibited satisfactory protective effects and revealed dose-dependence in protecting BSAagainst UV - TiO, - NO,` induced protein oxidation and tyrosine nitration injury.
Keywords: essential oil, tyrosinase, antioxidant, nano TiO2, protein oxidation, tyrosine nitration
徐春涛1,马飞2,纪红兵2
(1中山职业技术学院信息工程学院,2广东中山528404:中山大学化学与化学工程学院,广东广州510275)
摘要:红缨合耳菊属于西藏特有的菊科植物,其有潜在的美白及防晒效果。本文选择水、正已烷、乙醚和乙醉为溶剂,考察 4种草取溶剂提取液的紫外吸收效果,并结合最佳革取溶剂,考察不同提取工艺对红撄合耳莉防晒成分提取率的影响。结果表明,采用超声波提取工艺,以乙醇为萃取溶剂效果最佳,整体提取率为27%。采用气质联用仪(GC-MS)对红缨合耳菊提取液成分进行分析,研究发现提取物中含有较多的共双体系化合物,这些化合物分别是 3-亚甲基-6-(1-甲基乙基)环已烯、菜烯、环已烯等,带有共轭双键体系的化合物具有较强的紫外吸收效果,将红缨合耳菊提取液制成防晒霜,发现含有质量分数2.5%的红缨合耳菊提取物防晒霜在UVB(290~320nm)段禁外线区具有很好的禁外线防护功能,平均吸光度值为1.95。
关键调:红缨合耳药:防晒剂:防晒霜:提取物:紫外线中图分类号:TO658.2文献标志码:
A文章编号:1000-6613(2017)04-1429-05
DO1:10.16085/.issn.1000-6613.2017.04.037
Sunsereen ingredients of synotis erythopappa(Bur.et Franch)C. Jeffey et Y.L.Chen and its application in sun cream
XU Chuntao1, MA Fei2 . .JI Hongbing2
('College of Information Engineering, Zhongshan Polytechnic, Zhongshan 528404. China: 'School of Chemistry and
Chemical Engineering, Sun Yat-sen University, Guangzhou 510275,Guangdong. China)
Abstract: Synotis erythopappa ( Bur.et Franch) C. Jeffeyet Y. L Chen, as an endemic compositae in Tibete. has potential benifits in whitening and sun blocking. In this paper, four different solvents
(water, hexane, aether and alcohol) were used to extract the plant, respectively. The extraction was investigated by testing actual UV absorbtion value. Using the best extract solvent, different extract
technologies were used to evaluate the effectiveness of the extraction. The results showed thatethanol, as the extract solvent and combing with ultrasonic extraction technology, the exctraction rate was up to 27%. Gas chromatographymass spectrometer (GC-MS ) was used to analyze the sun block components from extract solvent. It was found that 3-methylenc-6-( l-methyl ethyl) cyclohexene, cyclohexene,
pinene, myrcene, with conjugated double bonds could absorb ultraviolet. With the synotis erythopappa(Bur.et Franch)C. Jeffey et Y.L. Chen extract as a sunscreen ingredient, it was found
sunscreen with 2.5% mass fraction of synotis erythopappa (Bur.et Franch) C. Jeffey et YL.Chen had very good UV protection in UVB (290- 320nm) ultraviolet region, and the average absorbance value
was 1.95.
Key words: synotis erythopappa( Bur.et Franch )C. Jeffey ct Y .L. Chen: sunscreen: sunscreen cosmetics; extracts; ultraviolet rays
3.1 前言
皮肤黑色素形成机理:存在于黑色素细胞组织中的酪氨酸在酪氨酸酶等酶的作用下经多巴、多巴醌、多巴色素、二羟基哚等中间体逐步转化为真黑色素,进而黑色素细胞组织将黑色素转移到表皮基底层细胞中,随着细胞的新陈代谢而被带到角质层中,最后随角质化细胞脱落。但是由于受紫外线、遗传、内分泌、炎症介质、饮食不当等因素的影响,黑色素代谢异常,皮肤黑素过快增长和分布不均,就会造成局部皮肤过黑及色素沉着,表现为黄褐斑、雀斑和炎症后色素沉着等。从国外文献来看,评价美白化妆品的功效主要以检测施加美白化妆品有效成分后,是否抑制酪氨酸酶活性为主要手段。目前,随着人们对祛斑美白药物需求的不断增加,越来越多的治疗色素沉着性疾病的药物投人到临床使用,其中不少药物确有良效,但使用中也出现了大量的不良反应导致严重的后果。
而将药物直接加入到细胞中观察药物对细胞的影响,则是一种最为直接的手段。由于黑素瘤细胞具有能够多次传代、生长快和培养条件相对较低等优点,成为筛选美白剂时的首选细胞。20世纪70年代初,Eisinger成功培养出正常黑色素瘤细胞,越来越多地采用人体正常黑色素细胞的体外培养技术。为此,我们基于实验室黑色素细胞培养,选用国内外常用B16黑素瘤细胞作为受试细胞,对红缨合耳菊的疗效和安全性的评价,为临床提供资料。
3.2材料与仪器
3.2.1 材料
红缨合耳菊提取物 自制
RPMI-1640培养基 美国 HyClone 公司
小牛血清 美国 HyClone 公司
胰蛋白酶 美国 HyClone 公司
L-多巴 美国 Sigma公司
Triton X-100 美国 Sigma公司
磷酸氢二钠 广州市化学试剂有限公司
磷酸二氢钾 广州市化学试剂有限公司
氯化钠 广州市化学试剂有限公司
氯化钾 广州市化学试剂有限公司
二甲基亚砜 广州市化学试剂有限公司
熊果苷 美国 Sigma公司
3.2.2 仪器
CJT-12超净工作台 北京昌平长城空气净化公司
DG-5031型酶联免疫检测仪 杭州博特仪器有限公司
CH2-TKC-3倒置显微镜 广东光学仪器有限公司
HZQ-F全温振荡培养 上海苏坤仪器有限公司
灭菌锅 上海苏坤仪器有限公司
3.3 实验方法
3.3.1细胞的培养及接种
无菌条件下,将B16细胞接种于含10%(体积分数)的小牛血清的RPMI1640培养基的培养瓶中,在5%(体积分数)COz培养箱中培养,每3d用0.25%胰酶消化传代一次。待细胞生长到对数期,用PBS洗涤,0.25%酶消化,细胞计数板计数。电镜观察细胞形态变化。调整细胞5X10个/mL。接种于96孔板中,每孔100L,置孵箱中孵育24h后,弃上清液,添加待测药物,每组药物最终质量浓度分别为320mg/L、160 mg/L、80 mg/L、40 mg/L、20 mg儿、10 mg/L、5 mg/L。每一浓度设5个孔,对照组不加药物,代之同量维持液,空白孔不接种细胞。37℃5%的CO,孵箱中孵育 72 h。
3.3.2 倒置显微镜观察
收集对数生长期细胞接种于6孔培养板中,每孔2ml。培养过夜后,加入不同浓度的药液100L,对照组加入同体积的RPMI-1640液。作用不同的时间后,置倒置显微镜下观察,照相并记录实验结果。
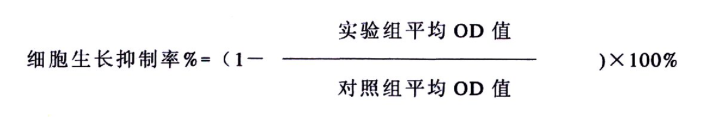
3.3.3黑色素细胞增殖抑制率测定
四甲基偶氮唑蓝比色法(MTT法):药物作用72h后,每孔加入5g/LMTT溶液10μL,4h后弃上清液,每孔加入 DMSO 100μL,振荡 10min 左右,在酶标仪上检测各孔吸光度值,以空白孔调零,波长为490nm。
3.4 实验结果与讨论
3.4.1 显微镜观察
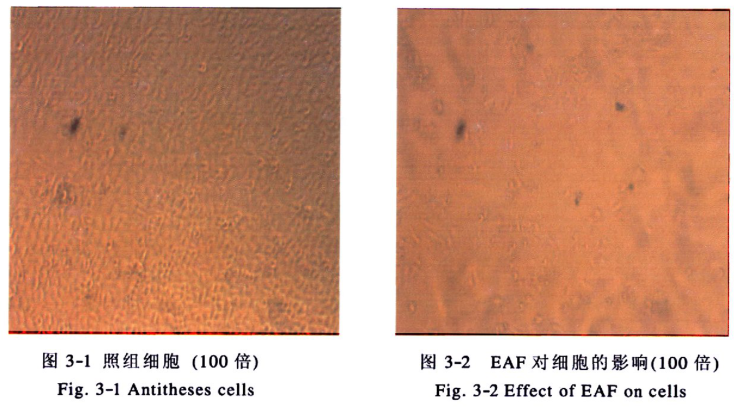
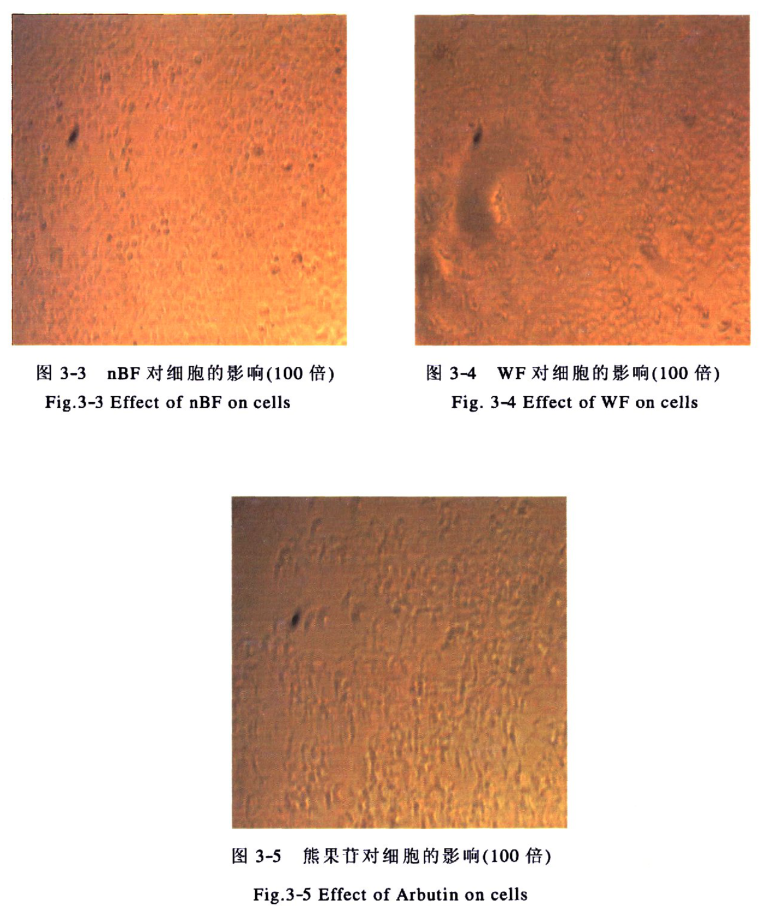
将红缨合耳菊各部分加入培养液(终浓度为320g/mL),作用于细胞后,我们发现细胞的形态明显发生变化。对照组细胞生长良好(见图3-1);加入EAF部分后,细胞树突减,细胞个数减少,变大(见图3-2);加入nBF部分后发现细胞未发生明显的变化,生长良好(见图3-3):加入WF部分后细胞生长状态稍差,不如对照组及nBF部分组(见图3-4):加入熊果苷组后能明显看到细胞树减少,细胞融合在一起(见图3-5)。
3.4.2 黑色素细胞增值率
红缨合耳菊可抑制黑色素细胞的生长,其效果与浓度相关,随着浓度的增加对细胞生长的抑制能力增加,320g/mL的熊果苷、EAF部分、nBF部分、WF部分对细胞生长的抑制率分别可达到42.57%、65.67%、10.24%、9.75%(表 3-1)。
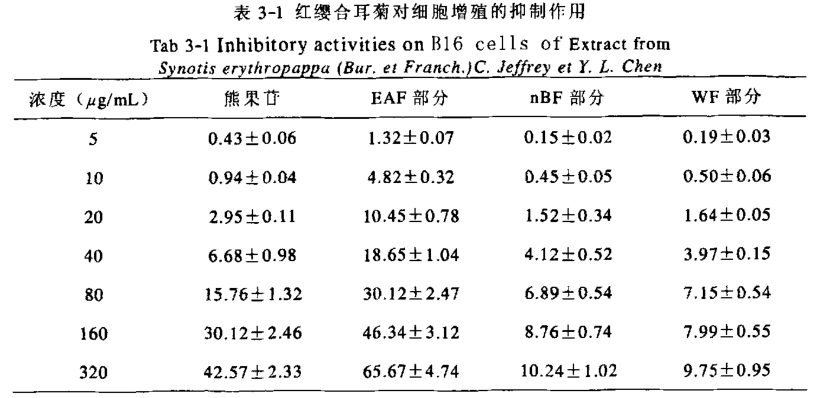
实验结果表明,受试物对黑色素细胞的毒性作用大小依次是:乙酸乙酯萃取部分>熊果苷>正丁醇萃取部分>水溶部分。熊果苷是常用的化妆品美白添加剂,其美白作用明显,人们对其美白作用的重视超过了对其细胞毒性的关注。然而许多研究均已表明熊果苷具有比较强的细胞毒性。我们的实验结果也对其进行了验证,当浓度为320μg/mL时,对细胞增殖的抑制作用可达到42.57%,可见其毒性较高。红缨合耳菊提取物的测试结果表明乙酸乙酯萃取部分对细胞的毒性比较大,而正丁醇萃取部分及水溶部分则对黑色素细胞的增殖抑制作用较小,浓度在320μg/mL时,其对细胞增殖的抑制率在10%左右,即这两部分有很小的细胞毒性。因此从健康方面考虑,在研究开发美白化妆品添加剂时,若使用熊果苷之类具有细胞毒性的物质,一定要在安全剂量范围内使用,而红缨合耳菊的正丁醇及水溶部分则可作为一种新型的天然植物提取物,基本没有剂量方面的限制。
3.5 本章小结
1.通过对细胞形态的观察,我们发现加入红缨合耳菊提取物及熊果苷后,细胞形态均发生变化,其中以EAF部分对细胞的影响最大。
2.测试了红缨合耳菊提取物对细胞生长的抑制率,研究发现,EAF部分对细胞的致死率最大,在320μg/mL时可达到65.67%,而nBF、WF部分分别为10.24、9.
未完待续……