Pressure ulcers are well known to be painful, costly and can negatively affect a patient’s quality of life. It has long been recognised that they increase the risk of infection, prolong hospital stays and can result in death (Young, 2021).
Discrepancies and systemic biases have been identified across healthcare systems, meaning that patients with dark skin may receive suboptimal care. It has been found that patients with dark skin tones are more likely to be diagnosed with higher-stage pressure ulcers due to inaccurate assessment and delayed identification (Oozageer Gunowa et al, 2017).
Many of the signs and symptoms that clinicians have been educated to look for as part of pressure ulcer prevention and identification may present differently depending on the patient’s skin tone. For example, it has been found that dark skin rarely shows the blanching response that clinicians are trained to look out for, and erythema may also be hard to detect (Grimes, 2009). A focus on ‘redness’ can be misleading, as the colour change can span the spectrum of pink, red, and purple – in some cases it may be limited to a subtle darkening of the existing skin tone (British Association of Dermatologists, 2021; Dhoonmoon et al, 2021).
Furthermore, a study on undergraduate nurse education at five higher education institutions in the UK confirmed that learning was predominately framed through a white lens, with white normativity being strongly reinforced through teaching and that learning activities were predominantly focused on white skin tones (Oozageer Gunowa et al, 2020), highlighting that teaching skin tone diversity is needed for many healthcare professionals.
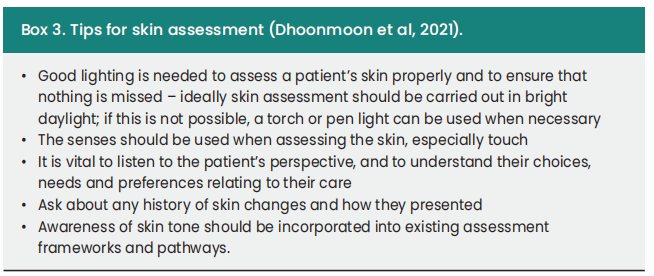
Best Practice guidelines have stated that skin inspection with an awareness of skin tone should be carried out as part of a full holistic assessment that includes the patient’s skin, their overall health and medical history, and their wound, ensuring that care is tailored to the individual and their needs. It is important to note that patients with all skin tones should receive an equitable level of assessment (Dhoonmoon et al, 2021).
The Christie project
The Christie NHS Foundation Trust, located in Manchester, stands as one of Europe’s largest cancer treatment centres. Given its diverse patient demographic, it is important for the staff to have the training and awareness to be able to provide optimal care for all and prevent potential patient harm. Within the Christie Hospital, there’s an increased likelihood of patients facing pressure ulcer risks. As the incidence rate of cancer rises, so does the potential for pressure ulcers, particularly when cancer affects a patient’s mobility and nutritional intake. Research strongly advocates for implementing comprehensive prevention strategies, citing their effectiveness in reducing incidence rates (Lyder, 2006).
A training and development project was developed, using the evidence in the Wounds UK Best Practice Statement (Dhoonmoon et al, 2021) to support staff awareness of skin tones. The aim of this project was to evaluate clinicians’ knowledge of skin tone assessment through a survey completed pre- and post-education, and to implement skin tone assessment into the existing aSSKINg bundle and the PURPOSE T pressure ulcer risk assessments.
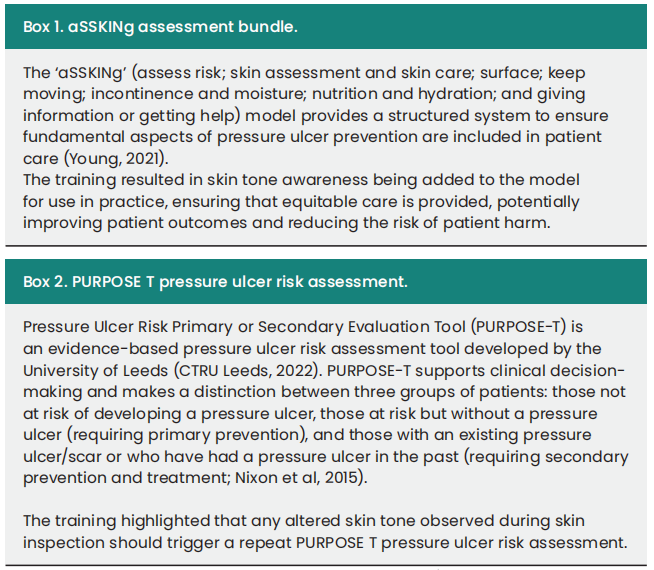
The nurse training package was based around the Best Practice Statement addressing skin tone bias in practice and use of the skin tone tool (Dhoonmoon et al, 2021). The training highlighted the need to measure and document baseline skin tone as part of the aSSKINg bundle, with skin tone assessment included in ongoing patient aSSKINg bundle assessments [Box 1] and any changes in skin tone detected through skin inspection triggering repeat PURPOSE T pressure ulcer risk assessment [Box 2].
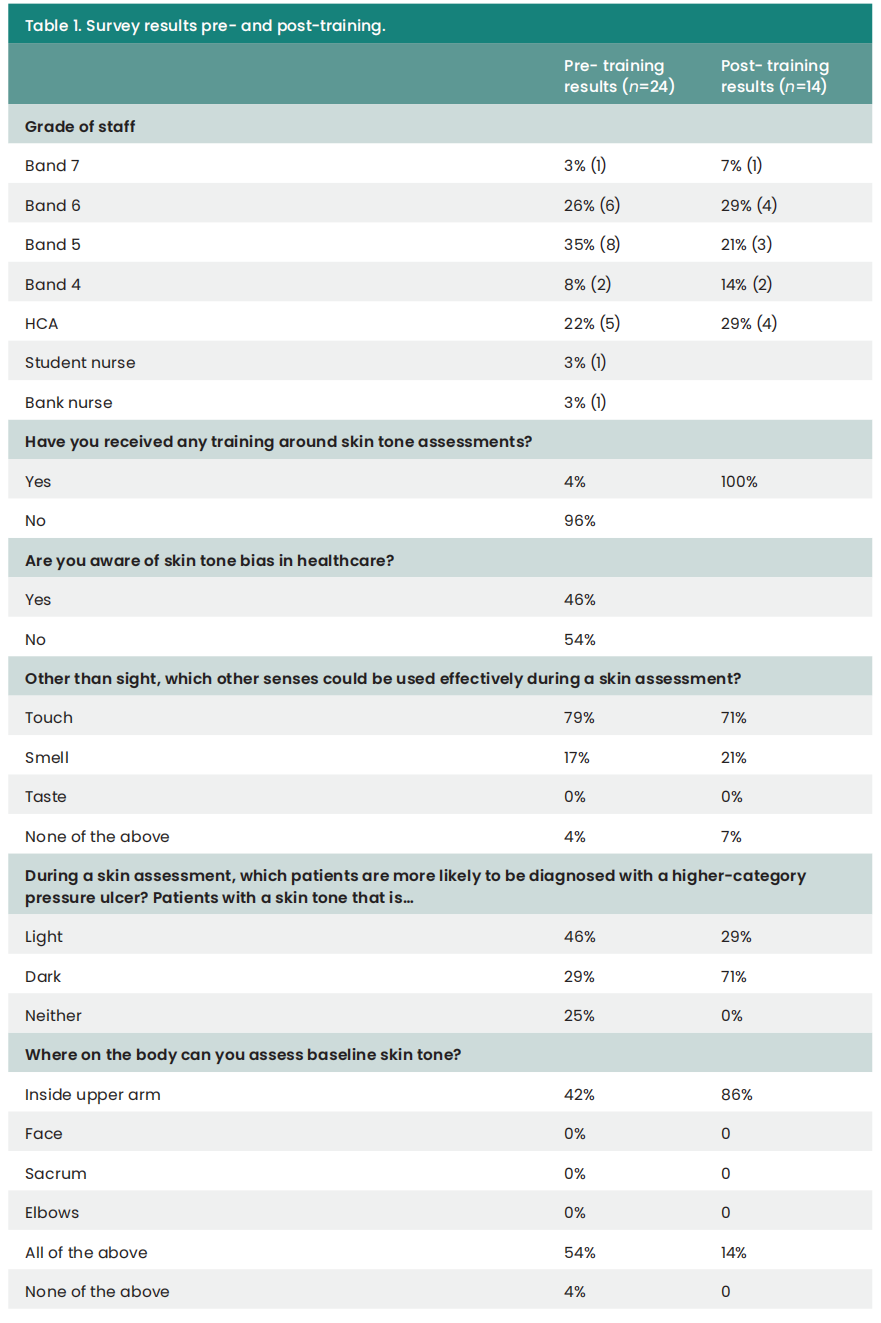
A survey was completed by staff both before and after training to establish existing knowledge and evaluate the impact of the education package.
Pre-training survey findings
Nurses completed the survey before undergoing the training package to establish baseline knowledge and measure the impact of the training.
The survey results showed that 96% of clinicians had not received previous training on skin tone assessment, with over half (54%) unaware of the issue of skin tone bias in healthcare. Before training, 46% of clinicians incorrectly thought that patients with light skin tone were at higher risk of developing highercategory pressure ulcers than those with dark skin tones.
Only 13% of clinicians reported feeling confident discussing skin tone with patients (33% were ‘not confident’, 13% ‘slightly confident’ and 41% ‘unsure’). None of the clinicians reported feeling ‘very confident’ discussing skin tone.
Less than half (42%) correctly identified that, according to best practice, patients’ skin tone should be assessed using the inside upper arm.
Despite this, the initial survey revealed a positive finding that, even before training, 79% of clinicians were aware of the value of touch in skin assessment, which is an important aspect of assessing all patients’ skin.
Skin tones training package
The skin tones training package consisted of face-to-face sessions lasting 15–20 minutes, conducted on the wards to align with the Best Practice Statement (Dhoonmoon et al, 2021). The primary focus was on integrating knowledge and awareness of skin tones into the existing aSSKINg assessment bundles and ensuring that any changes in baseline skin tone triggered a repeat PURPOSE T pressure ulcer risk assessment.
The sessions began with an introduction citing research (Oozageer Gunowa et al, 2017) showing higher occurrences of higher-category pressure ulcers in individuals with dark skin tones due to a lack of early identification and accurate assessment.
Discussions during the sessions highlighted differences in symptom presentation based on patients’ skin tones. For instance, dark skin typically rarely exhibits the blanching response that clinicians are trained to look out for, which also may pose challenges in detecting erythema (Grimes, 2009). This emphasised the need to engage all senses, particularly touch, in comprehensive skin assessments.
The training also covered specific questions integral to comprehensive skin assessments (page 5 of the Best Practice Statement; Dhoonmoon et al, 2021). Alongside introducing the skin tone tool for establishing baseline assessment, this tool was distributed to all clinicians.
A crucial aspect of the training involved integrating skin tone considerations into the aSSKINg bundle, detailing both baseline and altered skin tones, and how the identification of altered skin tone triggered the PURPOSE T pressure ulcer risk assessment [Figure 1].
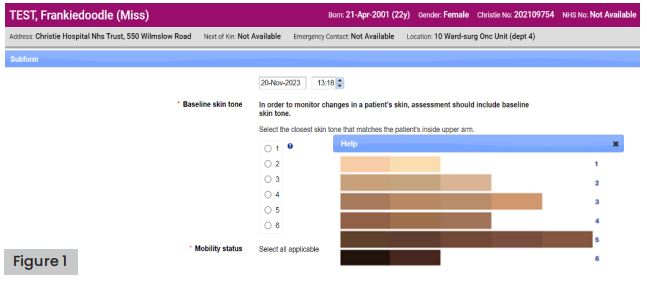
Figure 1. PURPOSE T pressure ulcer risk assessment with the inclusion of baseline skin tone assessment
To continuously reinforce learning, all training sessions were recorded and subsequently uploaded to the Christie HIVE intranet system, ensuring accessibility and facilitating ongoing education and knowledge consolidation for all staff members.
Post-training survey findings
After completing the training, clinicians were required to complete the survey again to assess the impact of the training on their knowledge. Following the training, only 7% of clinicians expressed that they did not feel confident in discussing skin tone with patients.
The percentage of clinicians who became aware that patients with dark skin tones are more at risk of developing highercategory pressure ulcers increased from 46% before training to 71% after training. For full information on the pre- and post-training survey data, see Table 1.
Use of the skin tone tool
The skin tone tool (adapted from Ho and Robinson, 2015) is a validated classification tool that shows a range of skin tones [see Figure 2], so that the tone can be selected that most closely matches the patient’s inside upper arm. The skin tone tool has been found to be a simple and economical way of assessing skin tone and can be used across various care settings, including with patients who may have limited literacy (Ho and Robinson, 2015). Unlike binary ‘light’ and ‘dark’ categorisations, this tool encompasses multiple gradients, making it more practical for clinical use (Dhoonmoon et al, 2021).
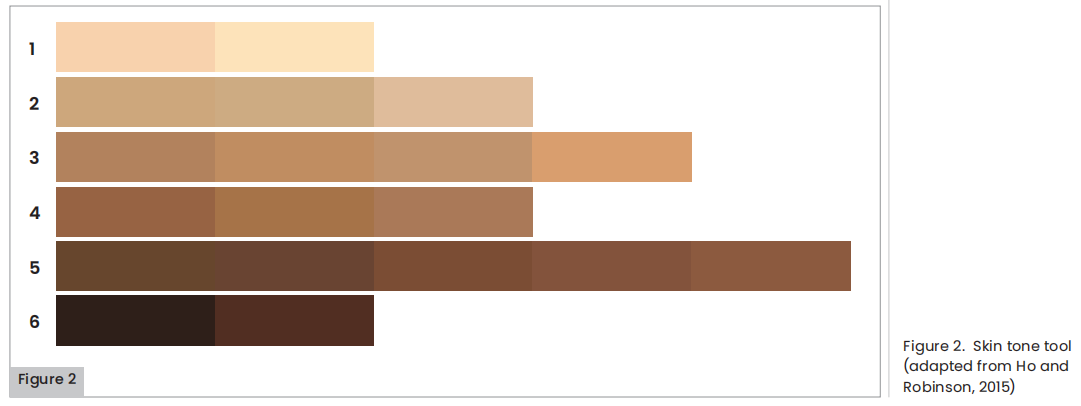
Following the training, clinicians were asked to identify patients’ skin tones using the skin tone tool in practice. A baseline skin tone of one was identified in 101 patients, two in 13 patients, three in 4 patients and five and six in 1 patient each. This demonstrates the staff’s ability to appropriately identify skin tone.
Implementation into practice
The training resulted in developments to practice, with the aim of providing equitable care to all patients, and ultimately improving patient outcomes and reducing the risk of patient harm.
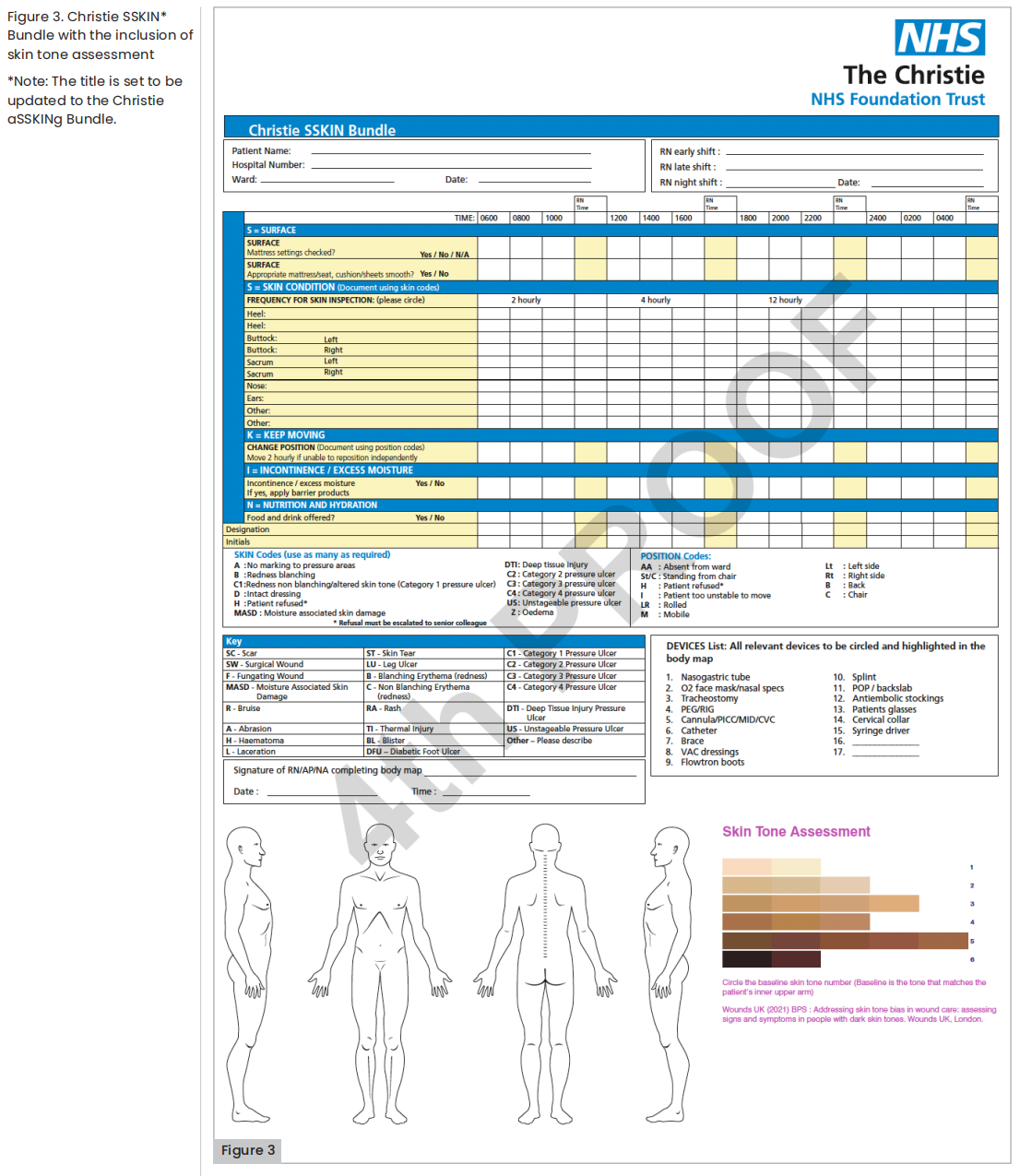
The skin tone tool was added to the aSSKINg bundle [Figure 3] so that baseline skin tone could be established at the initial skin assessment (every new aSSKINg bundle /24 hours). This is important to ensure that any changes to the skin are spotted, and potential pressure damage is identified as early as possible.
Challenges to implementation
During the early stages of implementation, discussions focused on establishing a baseline area for skin tone assessment. The Best Practice Statement (Dhoonmoon et al, 2021) recommends using the patient’s inside upper arm and choosing a skin tone. However, there was some debate about whether baseline assessments should include different anatomical locations on the body. Eventually, it was agreed that assessing baseline in multiple locations was impractical and that the inside upper arm should be used instead. Nonetheless, the importance of inspecting a comparable area of skin for reference was emphasised. For example, when examining the heel for a potential pressure ulcer, it is important to also examine the other heel whenever possible, as differences in skin tone between areas such as the soles are common.
As print quality could affect the validity and accuracy of the skin tone tool, ensuring high-quality print files for skin tone documents became crucial. The material of the cards was also considered important because it had to comply with Trust infection prevention guidelines. Changes were implemented in high-quality printing to ensure skin tone colours were accurate, and adjustments were made to the material of the cards to ensure they could withstand decontamination.
Despite these challenges, the project received support and endorsement from both documentation and clinical governance/ quality groups. This support was instrumental in overcoming any initial implementation challenges.
Clinician feedback
Clinicians initially expressed concerns about potential discomfort or awkwardness in raising the topic of skin tone assessment with patients. However, these worries dissipated as they engaged with the training, ultimately embracing it and feeling empowered by the knowledge gained.
Feedback from clinicians highlighted a notable shift in perspective. Many expressed newfound awareness regarding the crucial role of considering skin tone during skin assessments for all patients—an aspect they hadn’t previously taken into account. One clinician specifically acknowledged the potential negative impact on care delivery due to overlooking this factor in the past, stating “After the training, I now know how important it is to consider skin tone when carrying out skin assessments on all my patients. This is something I haven’t considered before and the negative impact it could have had on my care delivery.”
The introduction of the skin tone tool significantly influenced clinician behaviour, prompting them to routinely include skin tone assessment in their evaluations. This integration swiftly became a habitual part of their assessment process, demonstrating how quickly it was adopted and internalised within their practice. One clinician noted, “As soon as I see the skin tone tool, it prompts me to include a skin tone assessment.” Another mentioned, “It very quickly has become my habit to complete.”
Patient feedback
Moreover, the feedback echoed a sentiment of reassurance from patients. One patient expressed appreciation for the nurses’ awareness of different skin tones, highlighting the significance of receiving standardised care irrespective of individual differences, stating, “It is nice to know nurses are aware of different skin tones, so we all get the same care.”
Future developments
The Christie Hospital’s future developments involve expanding the scope of skin tone assessment by including it in their incident reporting tools, specifically DATEX. This strategic initiative aims to facilitate the auditing process for both the incidence and prevalence related to skin-related incidents within their setting.
Additional implementations sites
Several other Trusts have collaborated with Essity to formally integrate skin tone assessment into their pressure ulcer prevention protocols.
University Hospitals Sussex, NHS Foundation Trust
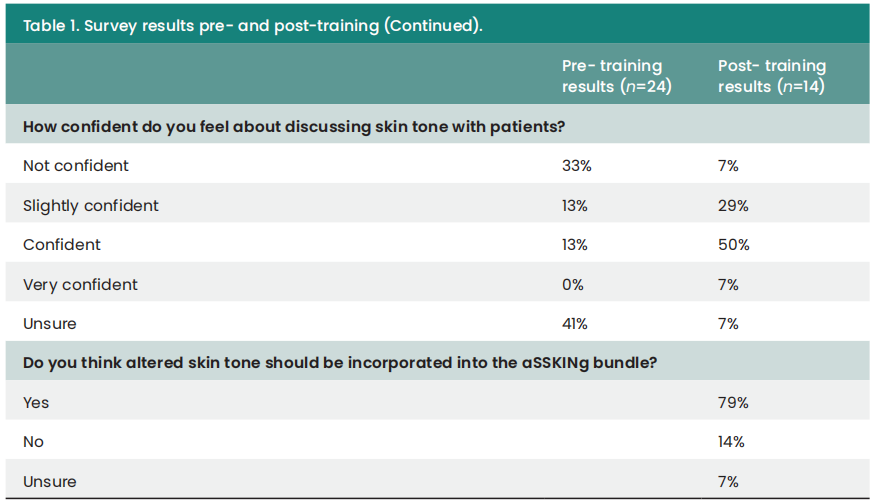
Claire Gillespie, Tissue Viability Clinical Nurse Specialist at University Hospitals Sussex, NHS Foundation Trust, has implemented skin tone assessment as a mandatory element of patient skin inspection throughout the Trust using a training and education programme. This initiative includes the ‘TAKE the Steps’ to Prevent Inequality in Pressure Damage Prevention Methodology: A Nurse’s Guide on Assessing Patients’ Skin Tones, which is shown in Figure 4. The acronym ‘TAKE’ stands for Touch, Ask, Knowledge and Examine.
In Claire Gillespie’s Trust, additional work needs to be done to ensure that the language used is appropriate for each patient.
Whipps Cross Hospital, Barts Health Trust
Maria Rebouco and Lourdes Rivera, Tissue Viability Specialists at Whipps Cross Hospital, Barts Health Trust, have implemented skin tone assessment into patient assessments following an audit aimed at investigating the identification and treatment of pressure ulcers. Findings revealed that staff were still looking for signs of redness on patients with dark skin, potentially overlooking category 1 or 2 pressure ulcers.
Whipps Cross Hospital serves a diverse community, with 50% of residents and 48% of the workforce in the area identifying as ‘non-white’. Formal skin tone assessment was implemented to ensure equitable care for all patients. An education programme was delivered to all staff, and skin tone is now included in all mandatory training at the Trust.
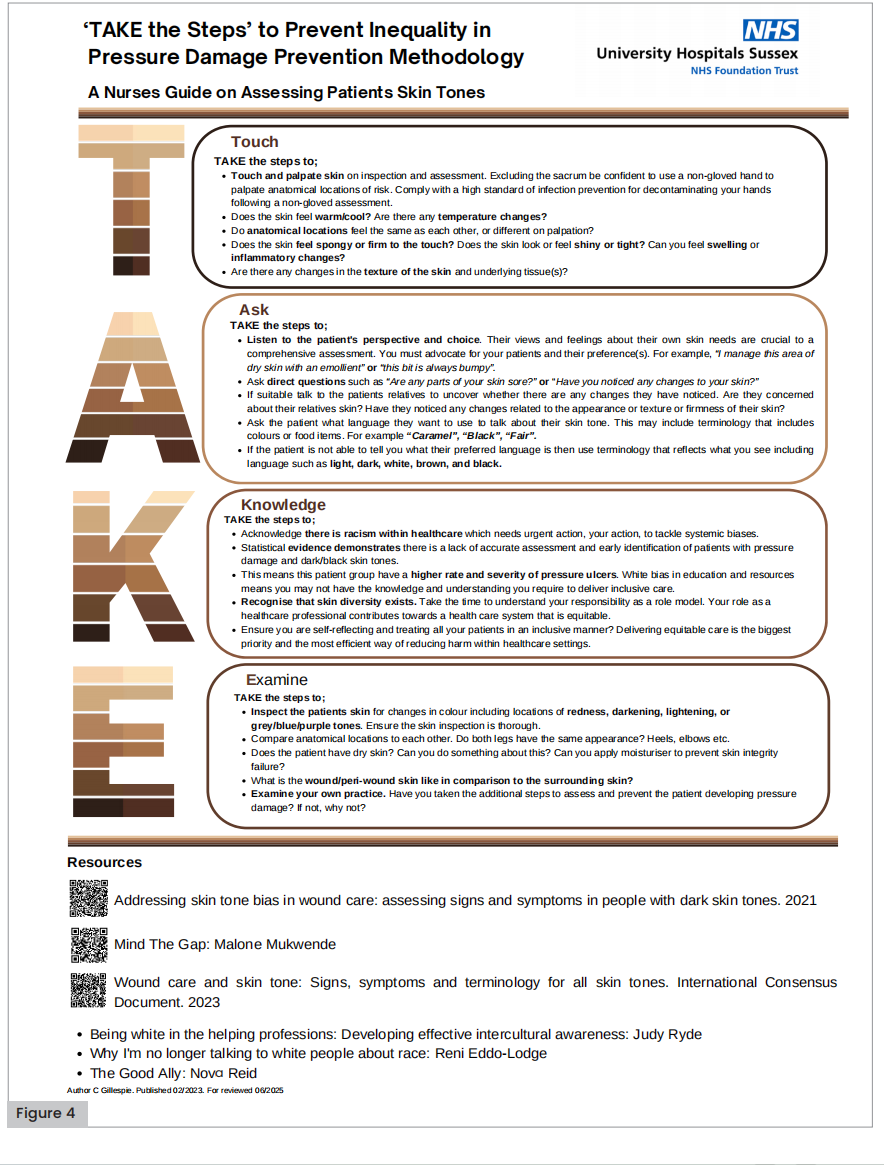
Figure 4. ‘TAKE the Steps’ to Prevent Inequality in Pressure Damage Prevention Methodology: A Nurse’s Guide on Assessing Patients’ Skin Tones
Manchester Foundation Trust
Maryam Bi, Senior Infection Control and Tissue Viability Specialist Nurse at Manchester University NHS Foundation Trust, with the support of her team, has implemented skin tone assessment into patient assessments. A comprehensive questionnaire with 30 staff members was undertaken to gauge competence in assessing dark skin tones and confidence levels. The forthcoming analysis of pre- and post-questionnaire results will be used to guide the implementation of skin tone training across acute and community settings.
In addition, the topic of caring for patients with dark skin tones is addressed in face-to face monthly sessions at the Tissue Viability Academy.
To emphasise the importance of assessing dark skin tones further, the slogan “suspect it, touch it, feel it” has been introduced in mandatory pressure ulcer eLearning sessions for Trust staff.
Wound assessment now includes evaluation of the surrounding skin tone, and the plan is to implement baseline skin tone in patients’ demographics using the HIVE intranet system.
Declaration
This article is supported by an education grant from Essity. Essity’s strategic healthcare partners are available to support the implementation of skin tone projects into clinical practice . Please contact concierge.service@ essity.com for help.
Additional tools are available to raise awareness of skin tone bias in wound care; see Box 4 for further reading.
Conclusion
It has been shown that there are gaps in clinicians’ knowledge around skin tone, which can result in inequitable care and potential patient harm. In particular, there is strong evidence that patients with dark skin tones are more likely to be diagnosed with highercategory pressure ulcers, leading to poorer outcomes (Oozageer Gunowa et al, 2017).
Skin assessment is a vital part of pressure ulcer prevention, and should be carried out with an awareness of skin tone (see Box 3 for tips for a good skin assessment). The patient’s baseline skin tone should be measured and recorded using the skin tone tool, so that any changes to the patient’s skin can be monitored and appropriate action can be taken promptly. An awareness of the patient’s baseline skin tone should mean that the clinician does not rely on generalised markers such as ‘redness’, which are not applicable to all patients and may result in pressure damage being missed in patients with dark skin tones.
Clinicians at the Christie NHS Foundation Trust participated in a pre- and post-training survey survey to assess their existing knowledge and evaluate the training’s impact. As a result of the training, the skin tone tool has been added into the aSSKINg assessment, with any changes in patients’ baseline skin tone triggering a PURPOSE T pressure ulcer risk assessment. The aim of this development is to improve patient outcomes and reduce the risk of potential patient harm.
References
1. British Association of Dermatologists (2021) Describing erythema in skin of colour. Available at: https://www. bad.org.uk/healthcare- professionals/inclusivity-and representation/ erythema-in-skin-of-colour (accessed 6.11.2023)
2. CTRU Leeds (2022) PURPOSE-T Registration. https://ctru. leeds.ac.uk/PURPOSE/PURPOSE-t/ (accessed 6.11.2023)
3. Dhoonmoon L, Fletcher J, Atkin L et al (2021) Best Practice Statement. Addressing skin tone bias in wound care: assessing signs and symptoms in people with dark skin tones. Wounds UK
4. Grimes PE (2009) Management of hyperpigmentation in darker racial ethnic groups. Seminars in Cutaneous Medicine and Surgery 28: 77-85
5. Ho BK, Robinson JK (2015) Color bar tool for skin type self-identification: a cross-sectional study. J Am Acad Dermatol 73(2): 312-3
6. Lyder CH (2006) Assessing risk and preventing pressure ulcers in patients with cancer. Semin Oncol Nurs 22(3): 178-184 doi:10.1016/j.soncn.2006.04.002
7. Nixon J, Nelson EA, Rutherford C et al (2015) Pressure Ulcer Programme Of research (PURPOSE): using mixed methods (systematic reviews, prospective cohort, case study, consensus and psychometrics) to identify patient and organisational risk, develop a risk assessment tool and patient-reported outcome Quality of Life and Health Utility measures. Programme Grants Appl Res 3(6):15-167
8. Oozageer Gunowa N, Hutchinson M, Brooke J et al (2017) Pressure injuries in people with darker skin tones: A literature review. Journal of Clinical Nursing
9. Oozageer Gunowa N, Hutchinson M, Brooke J et al (2020) Pressure injuries and skin tone diversity in undergraduate nurse education: Qualitative perspectives from a mixed methods study. Journal of Advanced Nursing
10. Young C (2021) Using the ‘aSSKINg’ model in pressure ulcer prevention and care planning. Nurs Stand 36(2): 61-6
This article is excerpted from the Wounds International 2024 | Volume: 15 Issue: 1 by Wound World.

