The advent of electronic healthcare records across the global health community has enabled the analysis of health outcomes by using retrospective health data. In former times, collating such data from paper records would have required massive investment in money and time.
While the analysis of electronic, retrospective, real-world data may be perceived as operating at a lower level of evidence, the speed, size of sample, analysis framework and implications of the results offer potentially useful and unique insights that can inform and develop current clinical practice.
In their recent article, Stedman et al (2023) report that for those with type 2 diabetes, of all of the factors assessed, renal complications were the most significant when considering risk in relation both to occurrence of incident foot complications and death once a foot complication has been identified, over a 10-year follow-up period. This was so, even compared to glucose and blood lipid control. Specifically, lowering of estimated glomerular filtration rate (eGFR) and elevation of the early morning urine albumin–creatinine ratio were associated with a higher risk of foot ulceration and a higher risk of death, when a foot complication has been identified. Conversely, in the absence of any foot complications, the risk of death for type 2 diabetes, as measured by mortality rate standardised for age and sex, was only slightly above that for the general population, at 13% over the follow-up period. This means that the long-term absence of foot complications is a positive prognostic factor for people with type 2 diabetes.
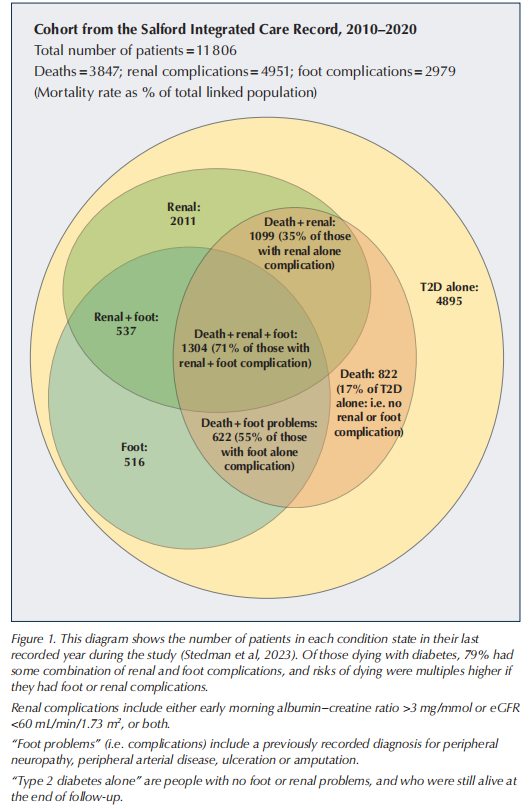
The findings are visualised in Figure 1. This shows that 79% of those dying with a diagnosis of diabetes have some combination of renal and foot complications, and that risks of dying are multiples higher if they have foot or renal complications. Notably, 71% of those with identified renal and foot complication died in the follow-up period, compared with 35% with a renal complication alone.
The clear take home message is “Think Foot, Think Kidney”. These findings suggest that there is an opportunity to identify those at risk of diabetes foot complications earlier and to reduce that risk, while also improving outcomes in those that do develop foot complications, with a targeted and stratified pharmacotherapeutic approach towards cardiorenal factors. There are now multiple strategies that can be employed to mitigate the progression of renal complications of type 2 diabetes (Davies et al, 2022). However, the rate of screening for microalbuminuria, which is often the first manifestation of diabetes-related renal pathology, is well below target in the UK, running currently at around 60% (NHS Digital, 2023; Stedman et al, 2023).
The authors found that the presence of any foot complication (or “foot problem”; defined as pulse deficit as a manifestation of peripheral vascular disease, diabetes-related peripheral neuropathy, foot ulcer or amputation) was associated with 6.9 life-expectancy years lost compared with that of an individual without diabetes. This comes as no surprise to those involved in diabetes foot care (Schofield et al, 2021), but highlights acutely the importance of aggressive targeting of cardiorenal risk factors, not just in those people with an active or historic foot ulcer, but in anyone with a documented diabetes foot complication now or in the past. Furthermore, the article provides evidence for the importance of prioritisation of screening for renal complications (ElSayed et al, 2023) in managing anyone with or without a diabetes foot complication.
The health economic consequences of diabetes foot ulceration have been highlighted previously from a UK perspective (Kerr et al, 2019). We suggest that intensive intervention to reduce the risk of foot ulceration should start before any diabetes foot complication is diagnosed, through the regular monitoring of renal function as well as the usual foot-care measures. Once foot complications aremanifest, this monitoring and remedial action should intensify.
One limitation of the study by Stedman and colleagues is that the population studied did not include many people of non-Caucasian ethnicity. There may be some disparities of risk and care in people from ethnic minority backgrounds, which would influence the development of diabetes complications (Haw et al, 2021). This does not, however, detract from the core message: “Think Foot, Think Kidney”.
To conclude, effective management of the atrisk diabetes foot requires active engagement between podiatrists, nurses in general practice and, where appropriate, diabetes specialists and diabetes specialist nurses to ensure that renal checks (including early morning urine albumin– creatinine ratio) go hand in hand with foot checks. With effective co-working, the rates of type 2 diabetes foot ulcers and diabetes-related mortality can be reduced.
References
1. Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65: 1925–66
2. ElSayed NA, Aleppo G, Aroda VR et al (2023) 11. Chronic kidney disease and risk management: Standards of Care in Diabetes–2023. Diabetes Care 46(Suppl 1): S191–202
3. Haw JS, Shah M, Turbow S et al (2021) Diabetes complications in racial and ethnic minority populations in the USA. Curr Diab Rep 21: 2
4. Kerr M, Barron E, Chadwick P et al (2019) The cost of diabetic foot ulcers and amputations to the National Health Service in English. Diabet Med 36: 995–1002
5. NHS Digital (2023) National Diabetes Audit. Available at: https:// digital.nhs.uk/data-and-information/publications/statistical/ national-diabetes-audit (accessed 21.12.23)
6. Schofield H, Haycocks S, Robinson A et al (2021) Mortality in 98 type 1 diabetes mellitus and type 2 diabetes mellitus: Foot ulcer location is an independent risk determinant. Diabet Med 38: e14568
7. Stedman M, Robinson A, Dunn G et al (2023) Diabetes foot complications and standardized mortality rate in type 2 diabetes. Diabetes Obes Metab 25: 3662–670
This article is excerpted from the Journal of Diabetes Nursing by Wound World.