Understanding HbA1c
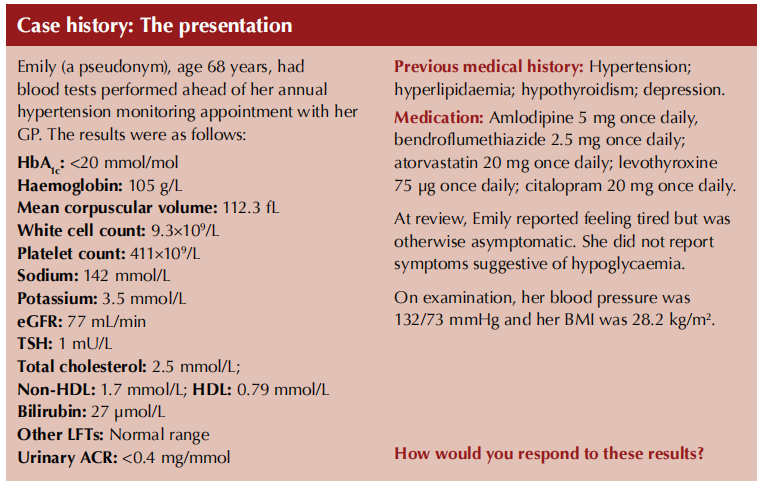
Under normal circumstances, approximately 97% of adult haemoglobin is haemoglobin A (HbA), which itself is composed of four globin chains: two alpha and two beta chains (Wang and Hng, 2021). When glucose binds covalently to the beta chain of HbA, the resulting form of the molecule then persists until the red cell is destroyed. In people without diabetes, around 6% of HbA is glycated, with the principal contribution, typically around 5%, coming from HbA1c (HbA can be glycated at other sites on the molecule). In people with diabetes, who have higher blood glucose concentrations, the level of HbA1c rises.
HbA1c, then, is a measure of the proportion of HbA within red cells that is glycated. It reflects the prevailing blood glucose levels over the lifetime of the red blood cell: approximately 120 days. It is important to note that glucose levels nearer to the time of HbA1c measurement contribute significantly more to the HbA1c value than those more distant from the time of testing, because red blood cells that are more recently glycated will better survive until the time of the test than older red blood cells (Little and Sacks, 2009).
HbA1c thus acts as a surrogate marker for plasma glucose levels over the previous 3 months – an average that is skewed to more recent glucose readings.
Utility of HbA1c in diagnosing and monitoring diabetes
HbA1c is routinely used as a means of diagnosing type 2 diabetes, with a threshold of 48 mmol/mol (6.5%), and is also used as a means of monitoring glycaemic control in all types of diabetes. An important advantage of using HbA1c is that a venous blood sample can be taken at any time, in contrast to fasting plasma glucose and the oral glucose tolerance test (OGTT), both of which require the individual to be fasted and, in the case of the OGTT, detained for a prolonged period. A further benefit of using HbA1c is that it is inherently less subject to the day-to-day variation of other diagnostic tests. HbA1c levels correlate well with diabetes complications.
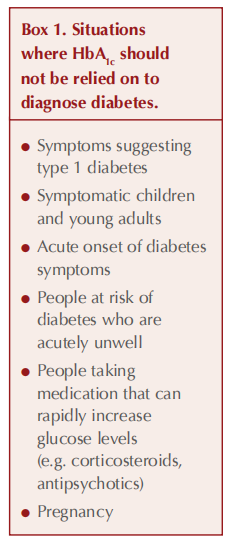
There are situations, however, when HbA1c should not be used as a diagnostic test for diabetes, notably when glucose levels have risen rapidly (see Box 1). In such situations, HbA1c will not accurately reflect current levels of glycaemia (Farmer, 2012; John, 2012). Remember that HbA1c does not indicate glucose variability, such that two individuals with very different glucose profiles could return the same HbA1c.
Unrepresentative HbA1c results
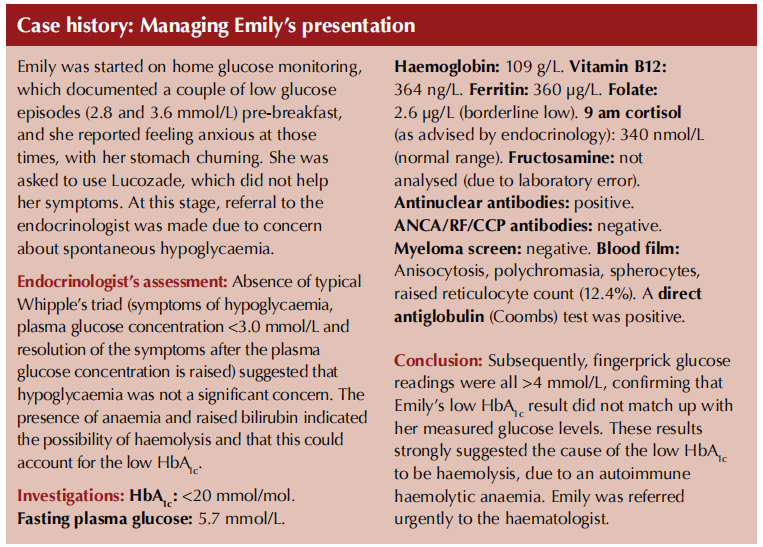
Conditions that reduce the lifespan of red blood cells and trigger increased erythrocyte turnover mean there is less time for glycation of red cells to occur and that HbA1c may, therefore, be falsely lowered (Radin, 2014; Wang and Hng, 2021). In contrast, and unlike in Emily’s case, extended erythrocyte survival or reduced erythrocyte turnover can lead to falsely elevated HbA1c values (see Table 1).
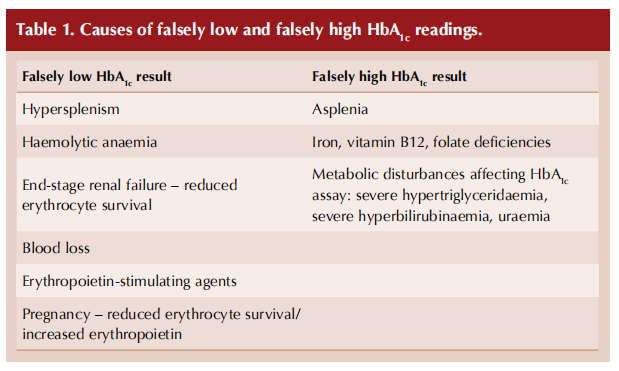
Haemoglobinopathies have a variable effect on HbA1c, and specialist advice should be sought (Radin, 2014). Blood transfusions can falsely lower or raise HbA1c, depending on the diabetes status of donor and recipient. It is also worth being aware that, for given levels of glycaemia, non-Caucasian populations have slightly higher HbA1c values than Caucasians (Herman and Cohen, 2012). HbA1c values should not be relied on in cases of severe anaemia (Hb <100 g/L).
Alternatives to HbA1c for assessing glycaemic control
Clearly, other means of assessing glycaemia need to be utilised in situations where it is suspected HbA1c could be unreliable. As in Emily’s case, self-monitoring of blood glucose (SMBG) can be undertaken, or if necessary some form of continuous glucose monitoring (CGM).
In pregnancy, the 75 g OGTT remains the gold standard for diagnosing diabetes (NICE, 2020). Thereafter, SMBG or CGM can be used to monitor glucose levels and direct treatment.
Serum fructosamine is an alternative measure of glycaemic control in situations where red cell turnover invalidates HbA1c, although it has not been validated as a measure of longer-term glycaemic control or as a predictor of diabetes complications (Rodin, 2014). The test measures glycation of proteins, principally albumin, and reflects glycaemic control over the previous 2–3 weeks, given that the half-life of albumin is around 20 days. However, fructosamine testing would be unreliable in the presence of hypoalbuminaemia.
Conclusion
HbA1c is a pragmatically useful surrogate marker for average glucose control over the preceding 3 months, albeit weighted towards more recent glucose levels. There are clinical situations, however, when HbA1c should not be relied on either to diagnose diabetes or to accurately reflect glucose levels. Unrepresentative HbA1c values can arise through altered erythrocyte lifespan. Under these circumstances, alternative means of assessing glycaemic control should be undertaken.
References
1. Farmer A (2012) Use of HbA 1c in the diagnosis of diabetes. BMJ 345: e7293
2. Herman WH, Cohen RM (2012) Racial and ethnic differences in the relationship between HbA1c and blood glucose: Implications for the diagnosis of diabetes. J Clin Endocrinol Metab 97: 1067–72
3. John WG; UK Department of Health Advisory Committee on Diabetes (2012) Use of HbA1c in the diagnosis of diabetes mellitus in the UK. The implementation of World Health Organization guidance 2011. Diabet Med 29: 1350–7
4. Little RR, Sacks DB (2009) HbA1c: How do we measure it and what does it mean? Curr Opin Endocrinol Diabetes Obes 16: 113–8
5. NICE (2020) to the postnatal period Diabetes in pregnancy: management from preconception [NG3]. https://www.nice.org.uk/guidance/ ng3
6. Radin MS (2014) Pitfalls in hemoglobin A 1c measurement: When results may be misleading. J Gen Intern Med 29: 388–94
7. Wang M, Hng TM (2021) HbA1c: More than just a number. Aust J Gen Pract 50: 628–32
This article is excerpted from the Diabetes & Primary Care Vol 25 No 5 2023 by Wound World.


