ABSTRACT
This is the 2023 International Working Group on the Diabetic Foot (IWGDF) guideline on the prevention of foot ulcers in persons with diabetes, which updates the 2019 guideline. This guideline is targeted at clinicians and other healthcare professionals.
We followed the GRADE methodology to devise clinical questions and critically important outcomes in the PICO format, to conduct a systematic review of the medical-scientific literature including, where appropriate, meta-analyses, and to write recommendations and their rationale. The recommendations are based on the quality of evidence found in the systematic review, expert opinion where (sufficient) evidence was not available, and a weighing of the desirable and undesirable effects of an intervention, as well as patient preferences, costs, equity, feasibility and applicability.
We recommend screening a person with diabetes at very low risk for foot ulceration annually for loss of protective sensation and peripheral artery disease, and screening persons at higher risk at higher frequencies for additional risk factors. For preventing a foot ulcer, educate persons at-risk about appropriate foot self-care, educate not to walk without suitable foot protection, and treat any preulcerative lesion on the foot. Educate moderate-to-high risk people with diabetes to wear properly fitting, accommodative, therapeutic footwear, and consider coaching them to monitor foot skin temperature. Prescribe therapeutic footwear that has a demonstrated plantar pressure relieving effect during walking, to help prevent plantar foot ulcer recurrence. Consider advising people at low-to-moderate risk to undertake a, preferably supervised, foot-ankle exercise program to reduce ulcer risk factors, and consider communicating that a total increase in weight-bearing activity of 1000 steps/day is likely safe with regards to risk of ulceration. In people with non-rigid hammertoe with pre-ulcerative lesion, consider flexor tendon tenotomy. We suggest not to use a nerve decompression procedure to help prevent foot ulcers. Provide integrated foot care for moderate-to-high-risk people with diabetes to help prevent (recurrence of) ulceration.
These recommendations should help healthcare professionals to provide better care for persons with diabetes at risk of foot ulceration, to increase the number of ulcer-free days and reduce the patient and healthcare burden of diabetes-related foot disease.
LIST OF RECOMMENDATIONS
1. Screen a person with diabetes at very low risk of foot ulceration (IWGDF risk 0) annually for signs or symptoms of peripheral neuropathy and peripheral artery disease, to determine if the person is at increased risk for foot ulceration, using the IWGDF risk stratification system. (GRADE recommendation: Strong; Certainty of evidence: High)
2. If a person with diabetes has loss of protective sensation or peripheral artery disease, extend the
screening using clinical history and further foot examinations to assess for
- a history of foot ulceration or lower-extremity amputation;
- diagnosis of end-stage renal disease;
- presence or progression of foot deformity;
- limited foot and ankle joint mobility;
- excess callus;
- and any pre-ulcerative lesion or ulcer on the foot, to determine their risk for foot ulceration using the IWGDF risk stratification system and to inform treatment. Repeat this screening once every 6-12 months for those classified as IWGDF risk 1, once every 3-6 months for IWGDF risk 2, and once every 1-3 months for IWGDF risk 3. (Strong; High)
3. Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to protect their feet by not walking barefoot, not walking in socks without shoes, and not walking in thin-soled slippers, whether indoors or outdoors. (Strong; Low)
4. Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to wash their feet daily (with careful drying, particularly between the toes), use emollients to moisturize dry skin, and cut toenails straight across. (Strong; Low)
5. Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to examine their feet daily and with the presence or suspicion of having a (pre-)ulcerative lesion, to rapidly contact an appropriately-trained healthcare professional for further advice. (Strong; Low)
6. Provide structured education to a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) about appropriate foot self-care for preventing a foot ulcer. (Strong; Low)
7. Consider coaching a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2-3) to self-monitor foot skin temperatures once per day to identify any early signs of foot inflammation and help prevent a first or recurrent plantar foot ulcer. If the temperature difference between corresponding regions of the left and right foot is above a temperature threshold of 2.2 °C (or 4.0 °F) on two consecutive days, coach the patient to reduce ambulatory activity and consult an adequately trained healthcare professional for further diagnosis and treatment. (Conditional; Moderate)
8. In a person with diabetes who is at risk of foot ulceration
a. and with no or limited foot deformity, no pre-ulcerative lesions and no plantar ulcer history (IWGDF risk 1-3), educate to wear footwear that accommodates the shape of the feet and that fits properly. (Strong; Low)
b. and with a foot deformity that significantly increases pressure or a pre-ulcerative lesion (IWGDF risk 2 or 3), consider prescribing extra-depth shoes, custom-made footwear, custom-made insoles, and/or toe orthoses. (Strong; Low)
c. and with a healed plantar foot ulcer (IWGDF risk 3), prescribe therapeutic footwear that has a demonstrated plantar pressure relieving effect during walking, to help prevent a recurrent plantar foot ulcer; furthermore, encourage the person to consistently wear this prescribed footwear, both indoors and outdoors. (Strong; Moderate)
9. Provide appropriate treatment for any pre-ulcerative lesion or excess callus on the foot, for ingrown toe nails, and for fungal infections on the foot, to help prevent a foot ulcer in a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3). (Strong; Very low)
10. In a person with diabetes at risk of foot ulceration (IWGDF risk 1-3) and a non-rigid hammertoe with nail changes, excess callus or a pre-ulcerative lesion on the apex or distal part of this toe:
a. consider digital flexor tendon tenotomy for treating these outcomes and to help prevent a first or recurrent foot ulcer (Conditional; Moderate), or
b. consider prescribing orthotic interventions, such as toe silicone or (semi-)rigid orthotic devices, to help reduce excess callus on the toe. (Conditional; Low)
11. In a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3), we suggest not to use a nerve decompression procedure to help prevent a foot ulcer. (Conditional; Very low)
12. Consider advising and referring a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) to participate in an 8-12-weeks foot-ankle exercise program, preferably under the supervision of an appropriately trained healthcare professional, and to continue performing foot-ankle exercises afterwards, with the aim of reducing risk factors for ulceration. (Conditional; Low)
13. Consider communicating to a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) that an increase in the level of walking-related weight-bearing daily activity by an extra 1000 steps/day is likely to be safe regarding risk of foot ulceration. Advise this person to wear appropriate footwear when undertaking weight-bearing activities, and to frequently monitor the skin for (pre-)ulcerative lesions. (Conditional; Low)
14. Provide integrated foot care for a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2 and 3) to help prevent a first or recurrent foot ulcer. This integrated foot care should include at least professional foot care, adequate footwear and structured education about self-care. Repeat this foot care or re-evaluate the need for it once every one to three months for a person at high risk, and once every three to six months for a person at moderate risk, as necessary. (Strong; Low)
INTRODUCTION
Foot ulceration is a major complication of diabetes mellitus and is associated with high levels of morbidity and mortality, as well as significant financial costs (1-4). The lifetime incidence rate of diabetesrelated foot ulceration is 19-34%, with a yearly incidence rate of 2% (5). After successful healing the recurrence rate of diabetes-related foot ulceration is 40% within a year and 65% within 3 years (5). Therefore, the prevention of diabetes-related foot ulceration is paramount to reduce the risk to the patient and the resultant economic and social burden to society.
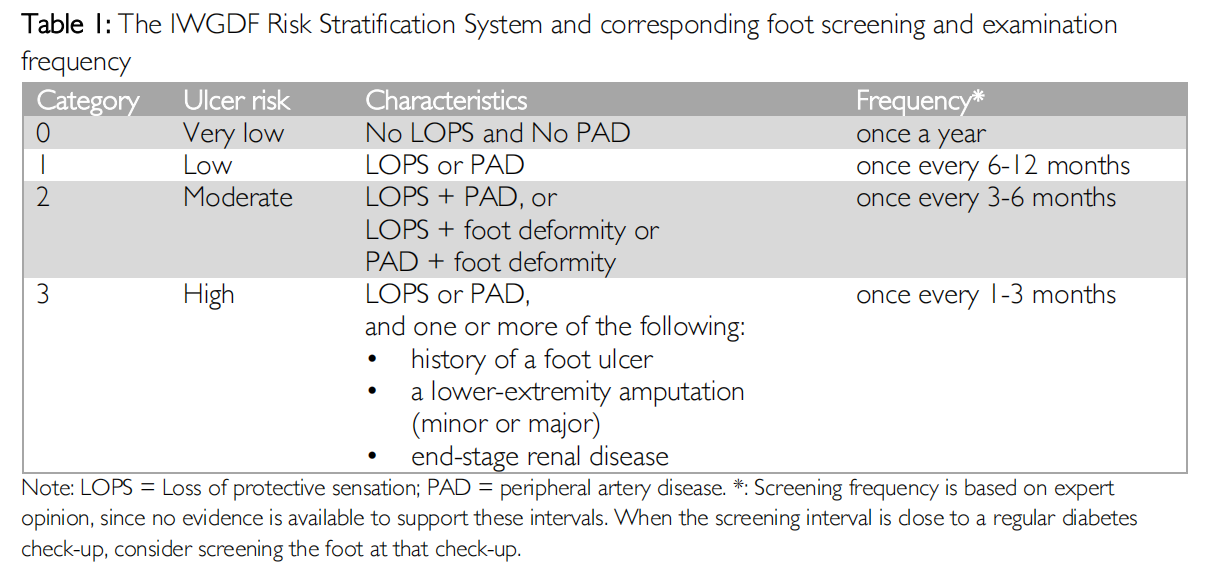
Not all people with diabetes are at-risk for ulceration. Key risk factors include: a loss of protective sensation (LOPS), peripheral artery disease (PAD) and foot deformity (5-7). Additionally, a history of foot ulceration and any level of lower extremity amputation, further increases the risk for ulceration up to 40% in one year after healing (5-7). In general, people with diabetes without any of these risk factors do not appear to be at an increased risk of foot ulceration in comparison to people without diabetes (5- 7). For the current guideline, we define a person at risk of foot ulceration as one currently or previously diagnosed with diabetes who does not have a foot ulcer, but who has at least LOPS or PAD. Table 1 shows the International Working Group on the Diabetic Foot (IWGDF) system for stratifying risk for foot ulceration.
Considering the above, only interventions aimed specifically at the prevention of foot ulcers in at-risk persons are included in this guideline. Within this group, those persons with a history of diabetes-related foot ulceration or amputation are considered at higher risk for ulceration when compared to those without such a history (7). Thus, we consider the first incidence of diabetes-related foot ulceration and recurrent incidences as separate outcomes of interest. Apart from ulceration as a key clinical outcome, other outcomes are also important for the prevention of foot ulcers and are considered in this guideline, following Grading of Recommendations, Assessment, Development and Evaluations (GRADE) methodology. These include pre-ulcerative lesions, quality of life, costs, foot-related mechanical stress, and adherence, among others.
Various interventions for the prevention of foot ulcers are either used in clinical practice or have been studied in scientific research (8, 9). We identify five key elements of prevention: 1) Identifying the at-risk foot; 2) Regularly inspecting and examining the at-risk foot; 3) Educating the person with diabetes, family and healthcare providers (this update newly including psychological interventions); 4) Ensuring routine use of appropriate footwear; 5) Treating risk factors for ulceration. Integrated foot care is a combination of these elements, and concerns the 6th element covered in this guideline.
The aim of this guideline is to provide evidence-based state-of-the-art recommendations for the prevention of foot ulcers in people with diabetes and includes a rationale of how we came to each recommendation. This guideline is targeted at clinicians and other healthcare professionals in the field. This guideline is part of the IWGDF Guidelines on the prevention and management of diabetes-related foot disease (10-15), and updates and replaces our previous guideline (16). The rationale provided is based on two systematic reviews of the literature (8, 9), together with a consideration of the desirable and undesirable effects of each intervention, as well as patients’ values and preferences, costs related to the intervention, equity, feasibility and acceptability, again using GRADE methodology. We also provide general considerations and propose an agenda for future research.
WHAT’S NEW IN THIS 2023 UPDATE
We have made several changes to the recommendations included in this updated 2023 guideline on foot ulcer prevention when compared to the previous 2019 guideline. The main changes are the following:
- Used a more thorough GRADE methodological approach to the guideline and the systematic review supporting it, by performing meta-analyses, grading effect sizes, grading certainty(quality) of evidence with ‘very low’ as an option, and developing summary of judgement tables;
- Added new clinical question on psychological intervention for ulcer prevention;
- Added new important outcomes, including health-related quality of life, costs, mortality, self-efficacy, well-being and adverse events;
- Split the recommendation on the use of footwear according to the severity of foot deformity present;
- Reorganized the recommendations for a person with diabetes at risk of foot ulceration and a nonrigid hammertoe to contain both a surgical and orthotic intervention recommendation; and
- Updated the strength of recommendation and the certainty of evidence underlying the recommendation where appropriate based on new available evidence and on using the more thorough GRADE approach.
METHODS
In this guideline we have followed the key steps of the GRADE evidence-to-decision framework, including: i) establishing a diverse expert panel to develop the guideline, ii) defining key clinical questions and important outcomes in the PICO-format (Patient-Intervention-Comparison-Outcome), iii) performing systematic reviews and rigorous appraisals of all available evidence that addresses the questions, iv) assessing summary of judgements items for each question, v) developing recommendations and their rationale based on these summary of judgements, and vi) consulting external stakeholders on each step (17, 18). The methodology for this guideline is summarised below; we refer those seeking a more detailed description on the methods for developing and writing these guidelines to the ‘IWGDF Guidelines development and methodology’ document (19).
First, a multidisciplinary working group of independent international experts in preventing diabetesrelated foot ulcers (the authors of this guideline) was invited by the IWGDF Editorial Board to develop and write this guideline. International experts were defined as those having significant experience in clinical practice and/or studying the prevention of diabetes-related foot ulcers and published on the topic in the previous four years. The working group comprised members from exercise and human movement science, podiatry, podiatric surgery, and physical therapy disciplines from Europe, North America, South America and Australia.
Second, the working group devised important clinical questions and associated outcomes, building on the last version of the guideline, to be answered using the GRADE approach. The questions and outcomes were reviewed and prioritised with the help of 18 external clinical experts and two persons with lived diabetes-related foot ulcer experience from various geographical regions, and the IWGDF Editorial Board. The aim was to ensure the questions and outcomes were of relevance to a wide range of healthcare professionals and people with the disease so as to provide the most useful clinical information on the prevention of foot ulcers in people with diabetes. The working group classified the outcomes as critically important or important, aligning with international diabetes-related foot ulcer standards (20, 21) or the expert opinion of the working group if standards did not exist.
Third, we systematically reviewed the literature and appraised all studies addressing the above agreed upon clinical questions. Each assessable outcome for each question was meta-analysed if appropriate, and had effect sizes and certainty of evidence assessed using the Cochrane and GRADE Handbooks. Finally, we developed evidence statements for each assessable outcome for each question which we presented in full in the systematic review. The systematic reviews supporting this guideline are published separately (8, 9).
Fourth, based on the systematic review, summary of findings tables and expert opinion, teams of two members of the working group developed summary of judgements tables for each question following GRADE (see supplemental information). The summary of judgement items assessed included desirable and undesirable effects, balance of effects, certainty of evidence, values, costs, cost-effectiveness, equity, acceptability and feasibility. Definitions for these items can be found in the Summary of Judgements tables in the supplemental information. After careful weighing of the summary of judgements, the team proposed to the working group a direction, strength, certainty of evidence and wording of recommendation(s) and rationale to address the question concerned. Certainty of evidence was rated as ‘high’, ‘moderate’, ‘low’ or ‘very low’ based on the critical outcome(s) reviewed for the question in accordance with GRADE. Recommendations aimed to be clear, specific, and unambiguous on what was recommended, for which persons, and under what circumstances. Rationale for each recommendation was also provided and based on the summary of judgements tables (17, 18).
Fifth, summary of judgements tables and recommendations for each question were extensively discussed in online meetings with the working group. After discussion, a voting procedure was used for each recommendation to grade the direction of the recommendation as ‘for’ or ‘against’ the particular intervention, and the strength of each recommendation as ‘strong’ or ‘conditional’. A quorum of 60% of members were needed to be present for a discussion and vote to go ahead and a majority vote of those present was needed for final decisions on each recommendation. The outcomes of the voting are provided in the supplemental information.
Finally, all recommendations, with their rationales, were collated into a consultation (draft) guideline manuscript that was reviewed by the same clinical experts and persons with lived experience who reviewed the clinical questions, as well as by members of the IWGDF Editorial Board. The working group then collated, reviewed and discussed all feedback on the consultation manuscript and revised accordingly to produce the final guideline.
CONFLICT OF INTEREST STATEMENT
The prevention guideline working group is committed to developing trustworthy clinical practice guidelines through transparency and full disclosure by those participating in the process of guideline development. In order to prevent a major Conflict of Interest (COI) members of the guideline group were not allowed to serve as an officer, board member, trustee, owner, or employee of a company directly or indirectly involved in the topic of this guideline. Before the first and last meeting of the guideline working group, members were asked to report any COI in writing. In addition, at the beginning of each meeting this question was also asked and if answered yes, the members were asked to submit a COI form. These COIs included income received from biomedical companies, device manufacturers, pharmaceutical companies, or other companies producing products related to the field. In addition, industry relationships had to be disclosed each time and these included: ownerships of stocks/options or bonds of a company; any consultancy, scientific advisory committee membership, or lecturer for a company, research grants, income from patents. These incomes could either be personal or obtained by an institution with which the member had a relationship. All disclosures were reviewed by the chair and secretary of the working groups and these can be found at www.iwgdfguidelines.org/about-iwgdfguidelines/biographies. No company was involved in the development or review of the guideline. Nobody involved in the guideline development received any payment or remuneration of any costs, except for travel and accommodation expenses when meeting on-site.
RESULTS
Overall, 14 clinical questions, each with up to 13 (critically) important outcomes, were finalised and addressed by this guideline. The accompanying systematic reviews identified 172 eligible studies, performed 10 meta-analyses and developed 33 evidence statements to collectively address these questions (8,9). Based on the systematic reviews and expert opinion of the group, 9 summary of judgements tables were completed (see supplemental material) with 14 recommendations developed that addressed the clinical questions.
The different interventions for ulcer prevention are organized and discussed according to five key categories of prevention: 1) Identifying the at-risk foot; 2) Regularly inspecting and examining the at-risk foot; 3) Educating the person with diabetes, family and healthcare providers (this update newly including psychological interventions); 4) Ensuring routine use of appropriate footwear; 5) Treating risk factors for ulceration. Integrated foot care is a combination of these elements, and concerns the 6th element covered in this guideline.
We refer readers to the glossary at the end of this guideline for the definitions of the interventions discussed. Furthermore, many of the interventions recommended require specific training, skills, materials and equipment to apply properly. These aspects are discussed to only a limited extent in this guideline as they are often not described in the studies performed and may differ between centres and countries, and are beyond the scope of the guideline. We suggest that the person applying the intervention should be a properly trained healthcare professional who according to their national or regional standards has the knowledge, expertise, and skills necessary to treat people with diabetes who are at risk of foot ulceration.
RECOMMENDATIONS
1. IDENTIFYING THE AT-RISK FOOT
Clinical questions:
- In people with diabetes what structure and frequency of screening for risk factors of foot ulceration is indicated?
- In people with diabetes what risk factors for foot ulceration should be screened for?
- In people with diabetes how should one screen for peripheral sensory neuropathy and foot deformities?
- In people with diabetes how should ulcer risk be defined?
Recommendation 1: Screen a person with diabetes at very low risk of foot ulceration (IWGDF risk 0) annually for signs or symptoms of peripheral neuropathy and peripheral artery disease, to determine if the person is at increased risk for foot ulceration, using the IWGDF risk stratification system. (GRADE recommendation: Strong; Certainty of evidence: High).
Rationale: Targeting people with diabetes for foot ulcer prevention treatment, first requires identification of those at-risk. We found no evidence in the literature on the direct effect of screening for preventing a diabetes-related foot ulceration. However, we recommend an annual foot screening for all adult persons with diabetes with no additional risk factors (IWGDF risk 0). Foot screening identifies those at risk and should specifically include screening for LOPS caused by peripheral neuropathy, and for signs or symptoms of PAD. Foot screening should also include assessment for presence of a foot ulcer, excess callus, or pre-ulcerative lesion, such as blisters, fissures and haemorrhage. Foot screening should be performed by an adequately trained healthcare professional (see glossary for definition). We do not aim to provide an exhaustive description of the assessment techniques or methods, as they have been detailed elsewhere, including in the IWGDF practical guidelines (22). LOPS can be assessed with a 10- gram Semmes Weinstein monofilament (22): a meta-analysis of individual patient data found consistent results using this assessment to predict risk of foot ulcer (7). If a 10-gram monofilament is unavailable, use the Ipswich Touch Test (23). While outcomes of this test were not included in the aforementioned meta-analysis, the Ipswich Touch Test has shown results similar to testing with the 10-gram monofilament (24). Because limited vibratory sensation may also predict risk of foot ulceration (5), we suggest to screen for this with a tuning fork or biothesiometer/neurothesiometer, if outcomes from monofilament testing do not show LOPS. Screening for PAD is discussed in the IWGDF Guidelines on PAD (13). In short, this includes taking a cardiovascular history, palpating for foot pulses, and obtaining pedal Doppler arterial waveforms and ankle-brachial pressure index and toe-brachial pressure index measurements. Although evidence for a screening interval is non-existent, we recommend an annual screening for a person with diabetes in whom LOPS or PAD have not yet been identified.
Based on a meta-analysis (7), the quality of the evidence that LOPS and PAD are predictive of foot ulceration is high. We suggest there are no undesirable effects associated with yearly foot screenings, the desirable effects of foot screening outweigh the undesirable effects. We also suggest persons with diabetes will value such yearly screenings as part of their regular diabetes check-ups. While foot screening is generally feasible, acceptable and inexpensive on the individual level, it can be more complex and costlier to organize on the societal level, given the growing number of people with diabetes and the limited time allotted for primary care visits. However, early identifying persons at risk of foot ulceration is important and is needed to target those who require preventative treatment. Therefore, the recommendation for annual foot screening is strong.
Because we found no evidence in the literature on the effect of screening for preventing a diabetesrelated foot ulceration, we did not complete summary of judgement tables for this question.
2. REGULARLY INSPECTING AND EXAMINING THE AT-RISK FOOT
Clinical questions: see under 1. IDENTIFYING THE AT-RISK FOOT
Recommendation 2: If a person with diabetes has loss of protective sensation or peripheral artery
disease, extend the screening using clinical history and further foot examinations, to include:
- a history of foot ulceration or lower-extremity amputation;
- diagnosis of end-stage renal disease;
- presence or progression of foot deformity;
- limited foot and ankle joint mobility;
- excess callus;
- and any pre-ulcerative lesion or ulcer on the foot, to determine their risk for foot ulceration using the IWGDF risk stratification system and to inform treatment. Repeat this screening once every 6-12 months for those classified as IWGDF risk 1, once every 3-6 months for IWGDF risk 2, and once every 1-3 months for IWGDF risk 3. (Strong; High)
Rationale: When either LOPS or PAD is identified in a person with diabetes, more extensive and more frequent foot examination is needed, as the ulcer risk is higher (5, 7). This examination should consist of taking a detailed history of foot ulceration, lower-extremity amputation, and determining a diagnosis of end-stage renal disease. Physically examine the foot for presence of deformities or progression thereof; excess callus and pre-ulcerative lesions, such as blisters, fissures and haemorrhage; and limited joint mobility of the foot and ankle (6, 7). A history of a previous foot ulcer or amputation are important predictive factors for a new ulceration, as identified in a meta-analysis of individual patient data (7). Foot deformities, excess callus, pre-ulcerative lesions, and limited joint mobility may increase the risk of foot ulceration (5, 25), and are important determinants of treatment in people with LOPS or PAD. Again, we do not aim to provide an exhaustive description of the assessment techniques or methods, as they have been detailed elsewhere, including in the IWGDF practical guidelines (22).
Notwithstanding the lack of evidence, other factors that we suggest taking a history of are: presence of social isolation, poor access to healthcare and financial constraints, depression or similar psychological comorbidities, frailty, foot pain (with walking or at rest) and numbness or claudication. We also suggest examining the presence of ill-fitting, inadequate, or lack of footwear; abnormal skin colour, temperature or oedema; poor foot hygiene, e.g., improperly cut toenails, unwashed feet, superficial fungal infection, or unclean socks; physical limitations that may hinder foot self-care (e.g. visual acuity, obesity); and poor foot care knowledge (25-28). Lacking footwear, or having Ill-fitting or inadequate footwear can be a cause of ulceration (26), and poor hygiene may be reflective of an inability to self-care. Appropriate interventions can potentially improve these modifiable risk factors when they are identified.
Any foot ulcer identified during screening should be treated according to the principles outlined in the other IWGDF guidelines (10-15).
IWGDF Risk Stratification
Based on the findings of the screening, a person with diabetes can be stratified according to their risk for foot ulceration (Table 1). The risk categories defined are based on a meta-analysis and a systematic review of prospective risk factor studies on foot ulceration (7).
Someone without LOPS and without PAD is classified as IWGDF risk 0 and is at very low risk for ulceration. This person requires only annual screening. All other categories are considered “at-risk,” and require more frequent foot screening, regular inspection and foot examination than in people who are not at-risk.
A person with either LOPS or PAD, but no additional risk factors, is stratified as IWGDF risk 1, and is considered at low risk. This person should be screened once every 6-12 months. When a combination of risk factors is present, a person is stratified as IWGDF risk 2 and is considered to be at moderate risk. As their risk is higher, this person should be screened every 3-6 months. All persons with either LOPS or PAD and a history of foot ulcer or lower-extremity amputation are stratified as IWGDF risk 3 and considered to be at high risk of ulceration. These persons should be screened once every 1-3 months. We also regard persons with LOPS or PAD in combination with end-stage renal disease (29-31) as being at high risk, irrespective of their ulcer history, and have therefore added these to IWGDF risk 3. We have not extended the high-risk level in the risk stratification system with new layers of sub-risk, nor have we included Charcot’s neuro-osteoarthropathy as high risk or modifiable risk factors in our risk stratification system. These options were discussed in the working group and we concluded that there was not yet sufficient evidence to add these aspects to the risk stratification system.
A person’s risk status should be made aware to the person and may change over time, thus requiring continuous monitoring. The screening frequencies we have provided help guide such monitoring. If findings lead to a change in risk status, screening frequency should be adjusted accordingly. As someone’s diabetes course progresses, upgrading is the most likely change. Downgrading risk status might occur after (surgical) interventions that normalize foot structure or improve lower extremity blood flow. Further, in a person with LOPS, it is not required to repeat the assessment of LOPS at subsequent screenings. It should also be noted that only biological measures determine the risk level, not behavioural measures. However, behaviour plays a role in foot ulcer risk. When a person with diabetes and neuropathy does not follow recommendations for a person at low-risk, for example by not wearing shoes at all, the risk of developing an ulcer is likely much higher, despite the low-risk stratification. This should be considered when determining the right preventative treatments for the individual person.
In view of the lack of evidence for the effectiveness of a screening interval in at-risk people with diabetes we recommend these intervals based on expert opinion. The aim of more frequent screening is early identification of risk factors that can increase the chances of developing a foot ulcer. This should then be followed by providing appropriate preventative foot care. For example, early diagnosis and treatment of pre-ulcerative lesions on the foot may prevent foot ulcers, as well as more severe complications such as infection and hospitalization. Screening for all these factors should help increase awareness, while it might also raise concern or feelings of anxiety in some people. However, we think that in general the potential for harm is limited. All screening can be done without the need for intrusive interventions and may also provide an opportunity to provide patient education, counselling and support. We suggest that the benefits associated with targeted preventative treatment following screening likely outweigh potential harms, provided appropriate treatment is given by an adequately trained healthcare professional. Screening takes relatively little time, and while this is feasible, acceptable and inexpensive at the individual level, it may be harder to organize and costlier on a societal level. Taking all evidence together, we strongly recommend such screening.
Because we found no evidence in the literature on the effect of examining the foot and on screening interval for preventing a diabetes-related foot ulceration, we did not complete summary of judgement tables for this question.
3. EDUCATING THE PERSON WITH DIABETES, FAMILY AND HEALTHCARE PROVIDERS
3A.Education on foot self-care
Clinical question: In a person with diabetes at risk of foot ulceration, should foot self-care be recommended?
Recommendation 3: Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to protect their feet by not walking barefoot, not walking in socks without shoes, or not walking in thin-soled slippers, whether indoors or outdoors. (Strong; Low)
Rationale: The feet of an at-risk person with diabetes need to be protected against high mechanical stresses, as well as external physical trauma, as both may cause foot ulcers (22). To protect their feet, a person with diabetes should therefore not walk barefoot, not walk in socks without shoes, and not walk in thin-soled slippers, either at home or outside. This also includes any other open type of footwear that increases risk for direct skin damage by a foreign object. While no studies have been directly performed to assess the effect of walking barefoot, in socks without shoes, or in thin-soled standard slippers, on risk of foot ulceration, there are at least large prospective studies that show that at-risk people with diabetes have elevated levels of mechanical plantar pressure during walking barefoot, in socks without shoes and in thin-soled slippers (32, 33). These high pressures are a significant independent risk factor for foot ulceration and should therefore be avoided (5). In addition, walking barefoot, in socks without shoes, or in thin-soled standard slippers has other harmful effects in at-risk people with diabetes, such as lack of protection against thermal or external mechanical trauma. Thus, despite the lack of direct evidence for this recommendation, we strongly advocate that people should be educated to avoid these walking conditions to reduce risk of damaging the foot. Only when supervised by a qualified healthcare professional, limited barefoot walking may be part of foot and ankle exercise programs for low-to-moderate risk people with diabetes (see recommendation 12).
People with diabetes might prefer not to follow this recommendation, especially inside their house (34- 36). However, given the potential harm of walking without shoes for foot protection outweighs any benefit to be gained from choosing this preference, we strongly recommend to educate at-risk people with diabetes not to walk barefoot, not to walk in socks without shoes, and not to walk in thin-soled standard slippers, whether at home or when outside. The education should be provided by a healthcare professional with disease-specific knowledge and skills in education.
Recommendation 4: Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to wash their feet daily (with careful drying, particularly between the toes), use emollients to moisturize dry skin, and cut toenails straight across. (Strong; Low)
Recommendation 5: Educate, and after that encourage and remind a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) to examine their feet daily and with the presence or suspicion of having a (pre-)ulcerative lesion, to rapidly contact an appropriately-trained healthcare professional for further advice. (Strong; Low)
Rationale: Although no direct evidence is available for the effect of these self-care interventions in preventing foot ulcers, they enable a person to detect and respond early to signs of diabetes-related foot ulceration and contribute to basic foot hygiene and escalation of care if indicated (i.e., if a preulcerative lesion is suspected). This education is likely to help prevent a foot ulcer, although it may pose some burden to people with diabetes.
The education should be provided by a healthcare professional with disease-specific knowledge and skills in education. Specifically, for washing their feet daily, people should avoid soaking their feet in a bath. With rapidly contacting an appropriately trained healthcare professional we mean immediately calling when identifying the lesion during normal working hours, or at earliest possibility outside of working hours. Appropriately trained means qualified to diagnose, either treat or refer people with diabetes and (pre-)ulcerative lesions.
It can be expected that people will generally consider basic foot hygiene as accessible and feasible, and that the desirable effects will outweigh undesirable effects associated with either inappropriate or inadequate or no foot self-care at all. These foot self-care behaviours can be done at a low cost per person who is at risk for diabetes-related foot ulceration. Despite the limited evidence for the effect of these self-care activities on ulcer prevention, this is a strong recommendation.
The summary of judgements for this clinical question is shown in the supplemental information.
3BProviding structured education about foot self-care Clinical questions:
- In a person with diabetes at risk of foot ulceration, should structured education be offered or provided?
- In a person with diabetes at risk of foot ulceration, should psychological interventions be offered or provided?
Recommendation 6: Provide structured education to a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3) about appropriate foot self-care for preventing a foot ulcer. (Strong; Low)
Rationale: Structured education is considered an essential and integral part of foot ulcer prevention, as it is widely thought fundamental that people with diabetes at-risk of foot ulceration need to understand their disease, and what recommended foot self-care is, in order to engage in that care (37). Structured education is defined as any educational modality that is provided to people in a structured way, that is through a protocol or other defined set of sequential routines and content. This can take many forms, such as one-to-one verbal education, education which is integrated into motivational interviewing, educational group sessions, video education, booklets, software applications, quizzes, and pictorial education via animated drawing or descriptive images. Despite this myriad of forms available and education being ingrained in clinical practice all over the world, research on its specific effectiveness (i.e., its desirable effects) for prevention of diabetes-related foot ulceration is limited although education seems to improve knowledge and foot self-care behaviour (9). Our meta-analysis of 5 RCTs shows a relative risk (RR) for ulcer occurrence (either first-ever or recurrent) of 0.66 (95%CI: 0.37-1.19), a statistically non-significant difference in favour of the intervention (9). Education seemed more effective in the subgroups with participants at lower risk of ulceration. Given its relative low cost, ease of provision and likely trivial undesirable effects, the use of this intervention is probably favoured on balance. Therefore, education should aim to improve the person’s foot care knowledge and self-care behaviour, and encourage the person to adhere to the foot self-care education provided.
Structured foot care education should consist of information on:
- Foot ulcers and their consequences
- Prevention-focused foot self-care behaviours, such as: not walking barefoot or in socks without shoes or in thin-soled slippers
- Wearing adequate protective footwear
- Undergoing regular foot checks
- Practicing proper foot hygiene; and
- Seeking professional help in a timely manner after identifying a foot problem (see recommendations 4 and 5).
As there is evidence of the benefits of treatment adherence on ulcer outcomes (38, 39), encourage people at risk of diabetes-related foot ulceration to adhere to the foot self-care education provided. It is best if such education is integrated with regular foot screenings (see recommendations 1 and 2), is reenforced and is part of integrated foot care (see recommendation 16). Structured education should be culturally appropriate, account for risk profile and gender differences, and align with a person’s health literacy and personal circumstances. The education should be provided by a healthcare professional with disease-specific knowledge and skills in education. These steps are likely to further enhance the acceptability and feasibility of the intervention. It is not possible to provide globally applicable recommendations on the best form of education given the diversity of contexts in which education will be provided. We suggest that structured foot self-care education should be provided individually or in small groups of people with diabetes. It should be provided over several sessions and with periodical reinforcement, to maximise effect.
In summary, although the certainty of the evidence for the desirable effects of structured education is low, we strongly recommend providing structured education on foot self-care given undesirable effects are likely to be trivial, face value is high, education is considered by most to be an acceptable and feasible intervention, and we assess that on the balance of effects the benefits of education likely outweigh the potential harms. While education could potentially lead to harm such as an increased fear of complications (40), it may also provide an opportunity for people with diabetes to clarify misunderstandings and seek answers to questions they have (28). People with diabetes will probably prefer structured education when it is appropriate to their circumstances, feasible, and accessible. While structured education is inexpensive at the individual level, it may be harder to organize and costlier on a societal level. Taken together, we strongly recommend providing structured education.
The summary of judgements for this clinical question is shown in the supplemental information.
Psychological interventions: We are unable to make a specific recommendation about the use of psychological interventions for the prevention of diabetes-related foot ulceration in at risk people, due to a very low evidence base at this time. We believe this is an important avenue for future research and clinical guidance due to the success of psychological interventions in other health-related areas, using evidence-based approaches such as motivational interviewing, cognitive behavioural therapy (CBT) and health behaviour change strategies.
3C.Instructions about foot self-management
Clinical question: In a person with diabetes at risk of foot ulceration should instructions about foot selfmanagement, including home foot temperature monitoring, be given?
Recommendation 7: Consider coaching a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2-3) to self-monitor foot skin temperatures once per day to identify any early signs of foot inflammation and help prevent a first or recurrent plantar foot ulcer. If the temperature difference between corresponding regions of the left and right foot is above a temperature threshold of 2.2 °C (or 4.0 °F) on two consecutive days, coach the person to reduce ambulatory activity and consult an adequately trained healthcare professional for further diagnosis and treatment. (Conditional; Moderate)
Rationale: Foot self-management differs from foot self-care as it involves more advanced interventions that are specifically designed for ulcer prevention, such as home-monitoring tools and telemedicine approaches. Self-management can include many interventions, but we found no evidence to support the use of any specific intervention, with the exception of home monitoring of foot skin temperature (9). We found evidence in our meta-analysis that home monitoring of plantar foot skin temperature at minimum once per day with an easy to use infrared thermometer, combined with subsequent preventative action when elevated temperatures were noted for two consecutive days, is statistically more effective than standard treatment for preventing foot ulcers in high-risk people with diabetes (IWGDF risk 2-3), with a relative risk of 0.51 (95%CI: 0.31-0.84) in favour of the intervention (9). These preventative actions include: reduction of ambulatory activity, consultation with an adequately trained healthcare professional to discuss the findings, and further preventative treatment as per the healthcare professional’s assessment. For this recommendation to be effective a person needs to have ready access to and the ability to use an appropriate thermometer and be in communication with an adequately trained healthcare professional.
Professionals may value at-home foot temperature monitoring as an easy to use relatively affordable method (in comparison to therapeutic footwear or surgery) that may have high clinical value and helps empower people in their care of their own feet. However, people with diabetes may have difficulty using temperature monitoring because of necessity to measure daily, requirement to target locations on the foot, the risk of false alarms, the requirement for surrounding infrastructure, and costs (41). For both professionals and people with diabetes, the value of skin temperature measurement may be compromised because of the risk of missing an ulcer that develops without the skin heating up before ulceration (42). In addition, practicalities of scaling up the usage of foot temperature monitoring on a global scale raises questions about the implementation of this intervention in different settings worldwide, and therefore there is an uncertainty about the widespread global feasibility of such devices.
The available evidence shows that adherence to measuring foot temperatures was an important factor in its effectiveness, and people, in particular those who have not had a foot ulcer, may find the requirement for daily assessment a burden (43, 44). False-positive and false-negative outcomes of temperature measurements may unnecessarily concern people and affect their confidence in using this approach (42, 45-48).
To our knowledge, home monitoring of foot temperature is currently not routinely implemented in foot care of people with diabetes at moderate to high risk of diabetes-related foot ulceration. This may be due to how people value the need for and ease of use of daily temperature measurements, lack of easy access to calibrated equipment, lack of full-report information on cost-effectiveness and implementation feasibility. Although the desirable effects outweigh undesirable effects, given the potential limitations of this intervention regarding i) equity among different settings, as the tool needed may not be frequently available to be used; ii) patient acceptability, as it adds a burden to measure foot temperature daily; and iii) feasibility, we decided that this is a conditional recommendation.
The summary of judgements for this clinical question is shown in the supplemental information.
4. ENSURING ROUTINE WEARING OF APPROPRIATE FOOTWEAR
Clinical question: In a person with diabetes at risk of foot ulceration, what orthotic interventions, including therapeutic footwear, should be used?
Recommendation 8: In a person with diabetes who is at risk of foot ulceration
a. and with no or limited foot deformity, no pre-ulcerative lesion and no plantar ulcer history (IWGDF risk 1-3), educate to wear footwear that accommodates the shape of the feet and that fits properly. (Strong; Low)
b. and with a foot deformity that significantly increases pressure or a pre-ulcerative lesion (IWGDF risk 2 or 3), consider prescribing extra-depth shoes, custom-made footwear, custom-made insoles, and/or toe orthoses. (Strong; Low)
c. and with a healed plantar foot ulcer (IWGDF risk 3), prescribe therapeutic footwear that has a demonstrated plantar pressure relieving effect during walking, to help prevent a recurrent plantar foot ulcer; furthermore, encourage the person to consistently wear this prescribed footwear, both indoors and outdoors. (Strong; Moderate)
Rationale: Appropriate footwear is considered an essential and integral part of foot ulcer prevention, as it is widely thought fundamental that people with diabetes at-risk of foot ulceration need to protect their feet from external stress, either through direct trauma or repetitive from weight-bearing activity, and from heat stress.
When educating about or prescribing footwear, also educate the person to check the inside of the shoe for any foreign objects each time before they don the footwear. Furthermore, the healthcare professional should be aware of cultural considerations around footwear and the impact this may have on uptake of wearing appropriate footwear and the level of education and support that will be required for uptake.
Advise the person wearing footwear to wear socks of natural materials/threads, that are seamless and preferably of light colour so that stains from (pre-)ulcerative lesions may become visible.
Rationale for 8a and 8b: People at moderate or high risk for foot ulceration (IWGDF risk 2-3) have often lost their ability to feel pain or pressure, and may not adequately judge the fit of their footwear or the level of pressure on their foot. Being at increased risk for ulceration, it is important that their footwear fits, protects and accommodates the shape of their feet; this includes having adequate length, width and depth (49). When a foot deformity or pre-ulcerative lesion is present, it becomes even more important to change foot biomechanics and reduce plantar pressure on at-risk locations. This may require custom-made footwear, custom-made insoles or toe orthoses. For people who have healed from a plantar foot ulcer, therapeutic footwear needs to reduce plantar pressure at high-risk areas, including the previous ulcer location. Based on a meta-analysis of 3 RCTs and 3 cohort studies, therapeutic footwear, including shoes, insoles or orthoses may reduce the risk of a first-ever or recurrent foot ulcer over a person’s own footwear in someone at moderate-to-high risk for diabetesrelated foot ulceration (IWGDF risk 2 to 3), with a relative risk of 0.53 (95%CI: 0.24-1.17) (8). Additionally, such footwear can reduce the plantar pressure during walking (50). High plantar pressures are a significant independent risk factor for foot ulceration and should therefore be avoided (5, 51). Because people with diabetes with LOPS cannot adequately judge footwear fit, footwear should be evaluated by appropriately trained professionals. Evaluate the fit with the person in the standing position, preferably at the end of the day (49). People at moderate or high risk with a foot deformity that significantly increases pressure or a pre-ulcerative lesion may require extra-depth shoes, custom-made footwear, custom-made insoles, and/or toe orthoses. The evidence shows variable effects on ulcer recurrence for specific insoles compared to standard insoles worn in therapeutic footwear (9). These insoles have a positive effect on in-shoe plantar pressure.
People with diabetes may value the role of properly fitting footwear, extra-depth and more custom footwear when they have a deformity to prevent ulcers, but some still consider their footwear to be the cause of their problems, especially when the footwear does not fit properly. Properly fitting footwear, extra-depth or custom-made footwear may also not align with personal comfort and style preferences, while in some countries wearing footwear is not customary at all or may lead to inconvenience (e.g. in warmer or wet climates). However, we know little about the adherence of people with diabetes at moderate risk for ulceration to wearing properly fitting footwear. Therapeutic footwear or adequately trained professionals may also not be present in all countries, which limits access to orthotic interventions. With the additional benefit of protection against thermal and mechanical trauma, and the evidence of reducing ulcer risk, we judge the benefits to outweigh the harm and therefore assign a strong recommendation.
Rationale for 8c: For people with a healed plantar foot ulcer (IWGDF risk 3), therapeutic footwear needs to reduce plantar pressure at high-risk areas, including the previous ulcer location. A meta-analysis of two RCTs on footwear or custom-made insoles that were demonstrably optimised for pressure reduction showed a relative risk of 0.62 (95%CI: 0.26-1.47) (9). For other outcomes, no differences were found between such pressure-optimized footwear and non-optimized footwear for pre-ulcer lesions, adverse events, health-related quality of life, adherence and mortality, while plantar pressure was lower in optimized footwear/insoles (3 RCTs and 3 non-controlled studies; (9)).
Demonstrated plantar pressure relieving effect means that at high pressure locations there should be a ≥30% reduction in the in-shoe peak pressure during walking (compared to the current therapeutic footwear), or an in-shoe peak pressure <200kPa (if measured with a validated, reliable, and calibrated in-shoe pressure measuring system with sensors sized 2cm2) (52, 53). The way to achieve such a pressure relief or level is by applying available state-of-the-art scientific knowledge on footwear designs that effectively offload the foot (54).
The desirable effects of continuously wearing optimised footwear or insoles with a proven offloading effect outweigh the undesirable effects, which are few based on the available trials (9). On the other hand, inappropriate footwear (inadequate length or width) increases the risk of ulceration (55), and we again stress the importance of ensuring adequate fit. Clinicians should also encourage people with diabetes to wear their prescribed footwear at all times. The costs of prescribing therapeutic footwear with demonstrated offloading effect may be quite high, as it requires the measurement of barefoot or in-shoe plantar pressure, which to date is relatively expensive for validated systems. However, these costs should always be considered in association with the benefit of ulcer prevention. Cost-effectiveness has not been reported to date. However, based on one unpublished cost-effectiveness analysis of pressure-optimized custom-made footwear as well as on the costs of foot ulceration, in our opinion, footwear designed or evaluated using plantar pressure measurement is likely to be cost-effective when it can reduce ulcer risk by 37% (the outcome from the meta-analysis), and even more when adherence is warranted (9). This is therefore a strong recommendation.
Note that this recommendation is predicated on the availability of both therapeutic footwear and accurate technology for pressure measurement. We acknowledge that the technology and expertise for such measurements are not yet widely available. For regions and settings where this can be made available, we encourage services to invest in regular plantar pressure measurements. For regions and clinical settings where this cannot yet be accommodated, we suggest to prescribe therapeutic footwear using available state-of-the-art scientific knowledge on footwear designs that effectively offload the foot (54).
The summary of judgements for this clinical question is shown in the supplemental information.
5. TREATING RISK FACTORS FOR ULCERATION
5A.Treatment of risk factors or pre-ulcerative lesions on the foot
Clinical question: In a person with diabetes at risk of foot ulceration, how should pre-ulcerative lesions and symptoms be treated?
Recommendation 9: Provide appropriate treatment for any pre-ulcerative lesion or excess callus on the foot, for ingrown toe nails, and for fungal infections on the foot, to help prevent a foot ulcer in a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3). (Strong; Very low)
Rationale: Pre-ulcerative lesions on the foot, such as blisters, fissures or haemorrhage appear to be strong predictors of future ulceration (5, 25, 27). Other risk factors that require treatment include excess callus, ingrown or thickened toe nails and fungal infections. These signs require immediate treatment by an appropriately trained healthcare professional. Appropriate treatment means: removing excess callus; protecting blisters and draining them when necessary; treating fissures; treating ingrown or thickened toe nails; treating cutaneous haemorrhage; and, prescribing antifungal treatment for fungal infections. The effectiveness of treating these signs on the prevention of a diabetes-related foot ulcer has not been directly investigated. Indirect evidence of benefit is that removal of callus reduces plantar pressure, an important risk factor for ulceration (9).
The benefit-harm ratio of treatment of pre-ulcerative lesions by an appropriately trained foot care professional will likely be positive, and come at relatively low costs. However, these treatments do have the potential to harm when improperly performed, and should therefore only be done by an appropriately trained healthcare professional and for the full length of time that the signs or lesions are present. It can be expected that people educated to the dangers of pre-ulcerative lesions prefer that they be treated. Despite a lack of evidence, we consider this standard practice and therefore the recommendation is strong.
The summary of judgements for this clinical question is shown in the supplemental information.
5B.Surgical interventions
Clinical question: In a person with diabetes at risk of foot ulceration, should surgical interventions be used?
Recommendation 10: In a person with diabetes at risk of foot ulceration (IWGDF risk 1-3) and a nonrigid hammertoe with nail changes, excess callus or a pre-ulcerative lesion on the apex or distal part of this toe:
a. consider digital flexor tendon tenotomy for treating these outcomes and to help prevent a first or recurrent foot ulcer. (Conditional; Moderate), or
b. consider prescribing orthotic interventions, such as toe silicone or (semi-)rigid orthotic devices, to help reduce excess callus on the toe. (Conditional; Low)
Rationale: Flexor tenotomy may reduce the risk of ulcer development in people with diabetes with excess callus on the tip of their toes or thickened nails (9). We consider flexor tenotomy a valuable procedure in a patient who has a pre-ulcerative lesion on the toe, that fails to respond to non-surgical treatment, and requires normalization of foot structure to prevent ulceration. Preventative surgery should only be considered after full evaluation of non-surgical treatment options by an appropriately trained healthcare professional.
The desirable effects of flexor tenotomy are moderate and likely outweigh the undesirable effects, as few complications have been reported (9), probably favouring the intervention. People with diabetes who have pre-ulcerative lesions for which they have frequent non-surgical treatment that does not improve outcomes may value and prefer treatment by flexor tenotomy. The procedure is easily performed in an outpatient setting, with no need for subsequent immobilization, and is not likely to negatively affect foot function. A flexor tenotomy is performed in a limited time and as an outpatient procedure and may prevent the use of non-surgical treatment options; thus, the added costs may be negligible, and the procedure may be cost-effective given the effect it has on ulcer prevention. Possible adverse effects of the surgery may include a transfer lesion or transfer pressure and should be discussed with the patient. In people with diabetes with poor arterial supply to the foot, this includes potential non-healing of the surgical incision or wound. Provided a surgeon is available, which seems the case in most settings, tendon tenotomy has little impact on equity, is acceptable and feasible. Due to the low number of controlled trials and low certainty of evidence, we consider the recommendation as conditional.
The summary of judgements for this clinical question is shown in the supplemental information.
To reduce excess callus and the associated increased foot pressure, people with diabetes at risk of ulceration (IWGDF risk 1-3) can be provided with toe silicone and (semi-)rigid orthoses or felted foam in addition to therapeutic footwear (9). The clinician should provide information on proper use of the orthosis, to avoid wrong placement that may even aggravate the situation.
Recommendation 11: In a person with diabetes who is at risk of foot ulceration (IWGDF risk 1-3), we suggest not to use a nerve decompression procedure to help prevent a foot ulcer. (Conditional; Very low)
Rationale: While observational studies on nerve decompression procedures have demonstrated low ulcer incidence rates over extended follow-up periods in people with diabetes with or without a prior foot ulcer experiencing neuropathic pain, there is no evidence to support an ulcer prevention effect of nerve decompression (9). Furthermore, if compared to standard of care in these studies, the standard of care was either poor according to current evidence-based guidelines or poorly described. Two RCTs are currently underway to assess the effect of nerve decompression, but primarily focus on quality of life and neuropathic symptoms, and secondarily on ulceration ((56) and NCT01762085). With various nonsurgical or other surgical interventions available that are accepted standards of good quality care to prevent a foot ulcer in an at-risk patient (recommendations 1-10, 14), and given the inherent risk of the surgical procedure, we suggest not to use nerve decompression to help prevent a foot ulcer.
The summary of judgements for this clinical question is shown in the supplemental information.
5C. Foot-related exercises and weight-bearing activity Clinical questions:
- In a person with diabetes at risk of foot ulceration, should foot-related exercises be done?
- In a person with diabetes at risk of foot ulceration, can the level of weight-bearing physical activity be increased?
Recommendation 12: Consider advising and referring a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) to participate in an 8-12-weeks foot-ankle exercise program, preferably under the supervision of an appropriately trained healthcare professional, and to continue performing foot-ankle exercises afterwards, with the aim of reducing risk factors of ulceration. (Conditional; Low)
Rationale: The risk of ulceration increases in the presence of risk factors. Interventions described in this guideline as part of education (section 3) and footwear (section 4) may help prevent foot ulcers, but do not mitigate the risk factors underlying them. While not all risk factors can be modified, some can. This includes plantar pressure distribution, neuropathy signs and symptoms, deficits in foot sensation, footankle joint mobility and strength (8). Various forms of foot-related exercises are possible when aiming to improve these modifiable risk factors for foot ulceration. These exercises can include stretching and strengthening of the foot and ankle joints and musculature and functional exercises, such as balance and gait exercises (8). These exercises are generally provided in 8-12 weeks training programs, supervised by physical therapists or other qualified and trained professionals, face-to-face or home-based, individually or in groups. In our meta-analyses, we found that these exercise programs do not increase the risk of ulceration, while improving foot and ankle joint range of motion, neuropathy signs and symptoms and plantar pressure distribution (8). As such, the desirable effects outweigh the undesirable effects.
As people with diabetes who are at risk of foot ulceration will likely not be aware of appropriate exercises, we recommend them to undergo a foot assessment and exercise prescription by an adequately trained healthcare professional prior to commencing exercise. Weekly evaluation of progress with training and modification of the program in collaboration with the professional is recommended. While this involves moderate costs, we assessed the importance of involving a healthcare professional for supervision and support as being of value because of the nature of the intervention, and also found better results on some outcomes if supervision was incorporated. People with a pre-ulcerative lesion or with a foot ulcer should not partake in foot-related exercises in which the foot is mechanically loaded, as there is still no evidence if these exercises are safe.
Advising people with diabetes at low to moderate risk of foot ulceration (IWGDF risk 1 or 2) to perform foot-related exercises is based on low certainty of evidence (8). Any potential for harm is outweighed by both general health benefits of exercise and specific improvements to the complex musculoskeletal deficits that develop with diabetes. Foot-related exercises are relatively easy to perform autonomously, are acceptable to people with diabetes, and feasible to execute. Minimal exercise equipment is required, for example elastic bands or exercise balls. As adherence may be a challenge, we advise health practitioners to continue to motivate people with diabetes to complete the exercise program as prescribed. We recommend regularly evaluating the training and outcome progress and updating the program when required. However, lifelong continued support from a health trained professional is not feasible. We therefore recommend that people with diabetes continue after the program, without professional support, preferably with the support of booklets, videos or rehabilitation technology tools. Feasibility of this part of our recommendation has not been studied, and it is unknown how people with diabetes assess such continuation. Because we expect the positive outcomes of the programs to continue if the exercises are continued, we do recommend people with diabetes to keep performing the exercise after the 8-12 weeks program.
We provide a conditional recommendation to this intervention. Although the benefits of performing foot-ankle exercises on health and foot-related outcomes outweigh the undesirable effects, it may require quite an effort to obtain the improvements in joint range of motion and neuropathy signs and symptoms, and the direct link between these improvements and ulcer prevention has not yet been proven. When implementation of foot-ankle exercises is considered as part of ulcer prevention programs, we stress the importance of first focusing on the strong recommendations in this guideline, such as the availability of adequate footwear. If these are met or at all unavailable in a given setting, implementation of foot-ankle exercises can be a relevant next step.
The summary of judgements for this clinical question is shown in the supplemental information.
Recommendation 13: Consider communicating to a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) that an increase in the level of walking-related weightbearing daily activity by an extra 1000 steps/day is likely to be safe regarding risk of foot ulceration. Advise this person to wear appropriate footwear when undertaking weight-bearing activities, and to frequently monitor the skin for (pre-)ulcerative lesions. (Conditional; Low)
Rationale: Exercise has general health benefits for people with diabetes, including specific improvements to the complex musculoskeletal deficits that develop with diabetes (57). However, when this exercise is weight-bearing, it increases the cumulative plantar tissue stress on the foot and should therefore be considered in the context of foot disease (58). Based on 4 studies where people with diabetes at risk of foot ulceration participated in a training program that increased their weight-bearing activity but where this did not result in increased incidence of ulceration (8), we suggest to consider advising people at low or moderate risk for ulceration (IWGDF 1 or 2) that a gradual increase in the level of walking-related weight-bearing activity is likely to be safe. We define an increase as a gradual increase in activity with an end goal of an additional 1000 steps/day, based on the increases seen in these 4 studies (8), and an RCT that showed such an increase to be beneficial for glycaemic control in people with diabetes (59). It is advisable to avoid sudden spikes in activity and to increase daily steps by a maximum of 10% per week, until a person reaches an overall increase of 1000 steps/day in comparison to baseline. This increase in daily steps may also be considered for those people with IWGDF risk 3 (60), as evidence showed that these people take on average the same number of daily steps compared to those at low or moderate risk (61). Thus it is probably safe, especially if they wear appropriate footwear when performing weightbearing activities (see recommendations 8-11).
The certainty of the evidence to support this recommendation is low, as it is based on 4 RCTs, but with none of them powered to detect a difference in ulcer development (8). This uncertainty is a concern (and an important area for future research). However, we think the lack of differences in rates of ulceration between the groups in these trials and the known benefits of increasing weight-bearing exercises on general health and foot-related outcomes, outweighs the harms. Also, increasing weightbearing activity is feasible for almost anyone, and as such this may increase equity to care. However, people with diabetes should remain cautious to avoid adverse outcomes such as falls and pre-ulcerative lesions. To prevent adverse outcomes, advise people with diabetes to wear appropriate footwear when undertaking weight-bearing activities (see recommendations 8-11), and to monitor their skin for preulcerative lesions or breakdown (see recommendations 4-6). Increasing the level of weight-bearing daily activity as recommended can be considered feasible and acceptable to people with diabetes. However, high drop-out rates in some trials show that this may not hold for all people with diabetes. Exercise programs are a relatively cheap intervention. Primarily because of the low quality of evidence in relation to ulcer prevention, this is a conditional recommendation.
The summary of judgements for this clinical question is shown in the supplemental information.
6. INTEGRATED FOOT CARE
Clinical question: In a person with diabetes at risk of foot ulceration, should integrated care be provided?
Recommendation 14: Provide integrated foot care for a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2 and 3) to help prevent a first or recurrent foot ulcer. This integrated foot care should include at least professional foot care, adequate footwear and structured education about self-care. Repeat this foot care or re-evaluate the need for it once every one to three months for high risk, and once every three to six months for moderate risk, as necessary. (Strong; Low)
Rationale: We define integrated foot care as an intervention that at a minimum integrates regular foot care and examination by an adequately trained professional, structured education, and adequate footwear. In our meta-analysis of 3 RCTs, we found an RR of 0.78 (95%CI: 0.58-1.06), a statistically nonsignificant difference favouring integrated over non-integrated care (9). One cohort study and five noncontrolled studies all reported a significantly lower percentage of recurrent ulcers in people with diabetes who received integrated foot care compared to those who did not, or in those people with diabetes who were adherent to an integrated foot care program compared to those who were not (9). None of the studies reported any complications from, or other harm related to, integrated care.
Professional foot care, by an adequately trained healthcare professional, consists of: treating risk factors and pre-ulcerative lesions as described in recommendation 9; structured education about foot self-care according to recommendations 3-6; and, providing adequate footwear following recommendation 8. The person’s feet should be regularly examined (see recommendations 1 and 2). Integrated foot care may further include foot self-management (recommendation 7), access to surgery (recommendation 10), and foot-related exercises and weight-bearing activity (recommendations 12 and 13). Given the efficacy of several interventions in people with diabetes without a history of foot ulceration, we also recommend integrated foot care for those with moderate risk of foot ulceration, based on the same expected cumulative effects of the combined interventions as with high-risk people.
While integrated foot care programs have been directly investigated in the controlled and noncontrolled studies found in our systematic review (9), none included all potential components of integrated foot care. The effect of a state-of-the-art integrated foot care program that combines all recommendations from this guideline is expected to be much stronger than that achieved by the programs researched to date (5, 62). Our recommendation that integrated foot care as minimum, consists of professional foot care, structured patient education, and adequate footwear, with a regular examination of a person’s feet, is based on this potential effect, shown by our systematic review and other analyses (5, 9, 62). However, the largest effect sizes in ulcer prevention can be found for selfmanagement and surgical interventions (9). Therefore, a complete integrated foot care approach should include these as well. For all aspects of an integrated foot care program, adherence to what is recommended increases the benefits, and should be given adequate attention in communication with the person with diabetes. Taken together, state-of-the-art integrated foot care has been estimated to be able to prevent up to 75% of all diabetes-related foot ulcers (62).
We found no information on costs and cost-effectiveness of integrated foot care. However, a publication from the United States suggested that there was an increase in hospital admissions for a diabetes-related foot ulcer after Medicare cancelled financial coverage in one state for preventative treatment given by podiatrists (63). Two further studies suggested that there was a reduction in amputations following the introduction of integrated foot care that included both ulcer prevention and ulcer treatment (64, 65).
Integrated foot care should be provided by one or more adequately trained healthcare professionals. People with diabetes at risk for foot ulceration who are cared for by professionals without specific expertise on diabetes-related foot disease should refer them to integrated foot care services. Educational interventions targeting healthcare professionals to improve completion rates of yearly foot examinations and to improve diabetes-related foot disease specific knowledge of healthcare professionals not involved daily in diabetes-related foot care may be important, but the effectiveness of such education is unclear (66). Teams that provide integrated foot care may perform educational outreach activities for healthcare professionals in primary or secondary care. The teams should be aware, however, that the effect of such education is limited with respect to knowledge improvement and performance of yearly foot examination, and may have to be repeated frequently.
The benefits of integrated foot care by one or more adequately trained healthcare professionals outweigh the potential harm of such treatment. We think it is likely that people with diabetes prefer integrated foot care delivered by healthcare professionals working in partnership rather than undergoing uncoordinated care delivered by different healthcare professionals working in isolation. We consider the combined effect size of the various interventions that make up integrated foot care to be high. Despite the low quality of the evidence, given the other advantages described, we rate our recommendation as strong.
The summary of judgements for this clinical question is shown in the supplemental information.
CONSIDERATIONS
1. The recommendations in this guideline are aimed at healthcare professionals providing treatment to people with diabetes-related foot disease. However, these professionals treat people with diabetes within a healthcare system or organisation, which itself may have an effect on outcomes. Although direct evidence for this is not available, indirect evidence comes from the effect of increasing podiatry and multidisciplinary teams in the Netherlands (67), which resulted in a reduction of lowerextremity amputations. A study in the US showed that treatment by a podiatric physician reduced 2-year medical care costs compared to no podiatric treatment (68) and yet another study that the discontinuation of podiatry care from Medicare in the US (63) resulted in an increase in hospitalizations for diabetes-related foot disease. The incidence of ulceration and ulcer recurrence is also associated with the availability, implementation and organisation of prevention services. Each of the above studies point to the potential importance of healthcare organisation in diabetes-related foot care, including ulcer prevention. We suggest that a healthcare system includes the multiple levels of foot care as described in the IWGDF practical guidelines (22), that people with diabetes can be referred from primary care to secondary care without delay, and that evidence-based preventative interventions are reimbursed within the system. Also, all healthcare professionals should be adequately trained to triage people with diabetes to ensure they are treated by the right professional. Investment in these aspects of the healthcare system is important to provide adequate preventative foot care for at-risk people with diabetes. This guideline is not written for governments or other agencies investing in healthcare organisations, but we do urge politicians and managers responsible to invest in healthcare systems that facilitate these characteristics.
2. All recommendations in this guideline are targeted at just three strata within the IWGDF risk stratification system (Table 1). Some specifications are given in relation to the location of a previous ulcer (e.g. plantar vs. non-plantar; toes vs. forefoot) or the presence of foot deformities, when recommending orthotic or surgical interventions. However, many differences between people with diabetes in the same stratum exist, and may limit providing the right treatment for the right person at the right time. No research has been done on such personalised medicine and its effects on the prevention of diabetes-related foot ulcers, which means that specific personalised recommendations cannot be made. This may change in the near future, as the medical community is moving more and more towards personalised solutions for medical problems (69).
3. An important factor for most recommendations made is a person’s adherence to the recommendations. As we noted in our previous guideline (16), adherence to an intervention has been shown to be crucial in preventing foot ulcers, and it is consistently reported that people with diabetes who do not adhere present with higher rates of ulceration (9). Several studies have investigated methods to improve adherence (36, 70, 71), but a stronger focus on the development, evaluation and implementation of methods that improve adherence to preventative foot treatment remains urgently needed. In turn, evaluating and optimizing feasibility and acceptability of treatments for people with diabetes, should be a key priority in the ongoing development and clinical research on the prevention of diabetes-related foot ulceration.
4. Probably the three most common preventative actions in daily clinical foot practice globally are foot screening (recommendations 1 and 2), foot self-care (recommendations 3 and 4), and (structured) education (recommendation 5). Despite the widespread application of these recommendations in clinical foot practice, the evidence underlying these recommendations is still poor (9). Frequency of foot screening is based on expert opinion only, and foot self-care and structured education have not been studied adequately. Lack of effect shown does not imply that these interventions do not work, but more research is needed to provide a stronger evidence base.
5. Costs and cost-effectiveness have only to a very limited extent been investigated for any of the interventions described in this guidance, and more attention to cost aspects is warranted. While some interventions are relatively inexpensive at the individual level (such as foot screening), they can be costly at a societal level, considering the millions of people with diabetes. Other interventions are costly at the individual level (such as custom-made footwear and surgical intervention), but reduce ulcer recurrence risk to a level that they are expected to be cost-saving at a societal level. Furthermore, cost-effectiveness can be very dependent on the setting (e.g. high resource versus low resource). More research in this area is needed.
6. We acknowledge that several or maybe many of the recommendations in this guideline and the implementation thereof are subject to aspects such as cultural diversity, religion, socio-economic status, equity, climate, geography, ways of living, values, priorities etc. Identifying these factors is important for a given setting to assess how applicable these guidelines are in that setting. Translation of the guidelines to different languages and the use of them for the development of national guidelines may be helpful tools here.
FUTURE RESEARCH AGENDA
Based on the gaps in the evidence as identified in our systematic reviews (8, 9), and the recommendations and considerations made in this guideline, we consider the following topics as the most important for future research:
- A general increase in research on the prevention of diabetes-related foot ulceration, both in quantity and quality, as research on prevention is still not sufficiently prioritized by funding bodies, policy makers, healthcare settings and clinicians and other healthcare professionals themselves (9).
- A state-of-the-art integrated foot care approach that combines up-to-date interventions as recommended in this guideline has not been investigated to date on efficacy to prevent foot ulcers, while the effect sizes of various interventions found suggest that up to 75% of foot ulcers can be prevented (62). This needs to be investigated in well-designed randomized controlled trials, of which one is currently underway (NCT05236660).
- Current treatment recommendations are based on stratified healthcare. Research is needed to explore the potential of a more personalised medicine approach in diabetes-related foot ulcer prevention, in order to to deliver the right treatment, to the right person, at the right time (69). See also consideration 2.
- Organisation of healthcare and healthcare setting likely plays a significant role in ulcer prevention, but this has not yet been investigated. This includes podiatry services, but also nursing homes, from which little data is available. See also consideration 1.
- Structured education is by many considered a key aspect of a foot ulcer prevention program, but it remains unknown what the exact effect is and which educational approach works best. Future
research should assess the effectiveness of various educational interventions, as well as the frequency of education provided. This includes, but is not limited to, motivational, psychological, or other behavioural interventions, e-health applications and (online) social support systems by peers or healthcare professionals.
-
Adherence to treatment is crucial to achieve the best possible outcome in ulcer prevention, but it is still largely unknown how adherence can be improved. Research to develop interventions that have the potential to improve adherence is needed. These interventions may include, among others, assistive technology, educational and behaviour change interventions or footwear solutions. Some proof-of-principle studies on some of these interventions have been conducted and are reported in these guidelines or the systematic review underlying the guideline (9). However, definitive randomized control studies are needed, to test the efficacy of interventions aimed at improving adherence to treatment to prevent ulcers. See also consideration 3.
-
The costs and the cost-effectiveness of interventions that aim to prevent foot ulcers needs to be investigated more extensively. See also consideration 5.
-
Peripheral neuropathy is the most important risk factor for the development of foot ulcers in people with diabetes, but there is little research on the prevention or treatment of neuropathy. A stronger research focus in this area is needed.
-
Robust data are lacking on whom, how, and when to screen for the risk of foot ulceration. High quality data on the benefit of interventions to prevent a first foot ulcer are scarce. As the event rate (foot ulceration) is relatively low in a population without a previous ulcer, to have clinical impact on first foot ulcer occurrence, large numbers of people with diabetes would need to be targeted. It is unclear if the potential benefit for the relatively small number of first ulcers prevented, would outweigh the resource and cost burden of large-scale preventative treatment implementation. Studies should, however, better define the categories of people with diabetes that will benefit from preventative interventions and what specific types of interventions should be included.
-
Foot-ankle exercise programs show some promising benefits on risk factors of ulceration, also in meta-analyses (8). However, these are primarily measured directly at the end of the program, mostly at 8 or 12 weeks. Future studies should investigate longer-term outcomes, including the acceptability and feasibility of continuing with the exercises beyond the supervised part of the program, and should also focus on ulceration as outcome.
-
The development and evaluation of adjunctive psychological interventions, to support the psychosocial wellbeing of people with diabetes, their families, friends and supports, and help prevent diabetes-related foot ulceration and, are urgently needed. This is an undeveloped area in the prevention of diabetes-related foot ulceration, however, it presents strong promise and is an important focus for future research.
CONCLUDING REMARKS
The global patient and economic burden of diabetes-related foot disease can be considerably reduced when evidence-based preventative treatment is implemented in the foot care of people with diabetes who are at risk of developing a foot ulcer. Reducing the risk of ulceration also reduces the risk of infection, hospitalization, and lower-extremity amputation in these people with diabetes. Despite foot ulcer management still being regarded as the top priority by most clinicians and researchers, foot ulcer prevention should be considered the best way to prevent severe morbidity and mortality in people with diabetes. Following the recommendations for preventative treatment in this guideline will support healthcare professionals and teams to continuously improve the quality of care provided for people with diabetes who are at risk of ulceration.
As part of quality improvement, we encourage our colleagues, both those working in primary care and in diabetes-related foot clinics, to consider developing forms of surveillance (e.g., registries, pathways) to monitor and track the foot health outcomes of people with diabetes at risk of foot ulceration. We also encourage our research colleagues to consider our future research agenda to conduct properlydesigned studies in collaboration with clinicians (20) to address the gaps identified in the evidence base to better guide policy and practice decisions on the most effective treatment to help prevent foot ulceration in people with diabetes who are at risk of ulceration.
GLOSSARY
Excess callus: Callus assessed by an appropriately trained healthcare professional as requiring debridement to reduce risk for ulceration.
Adherence: The extent to which a person’s behaviour corresponds with agreed recommendations for treatment from a healthcare provider (72), expressed as quantitatively as possible; e.g. the proportion of time, steps or instances that the prescribed intervention (or comparator) is used.
Adequately trained healthcare professional: a person who according to national or regional standards has the knowledge, expertise, and skills to perform a specified task in screening, examining, or managing a person with diabetes who is at risk of foot ulceration.
Custom-made insole: An insole that is custom-made to the individual’s foot using a 2D or 3D impression of the foot, and that is often built-up in a multi-layer construction. This may also incorporate other features, such as a metatarsal pad or metatarsal bar. The insole is designed to conform to the shape of the foot, providing cushioning and redistribution of plantar pressure. The term “insole” is also known as “insert” or “liner”
Custom-made (medical grade) footwear: Footwear uniquely manufactured for one person, when this person cannot be safely accommodated in pre-fabricated (medical grade) footwear. It is made to accommodate deformity and relieve pressure over at-risk sites on the plantar and dorsal surfaces of the foot. In-depth assessment, multiple measurements, impressions or a mould, and a positive model of a person’s foot and ankle are generally required for manufacture. This footwear includes a custom-made insole. Also known as “bespoke footwear” or “orthopaedic footwear”.
Diabetes-related foot ulcer (DFU): see IWGDF definitions and criteria document (21).
Extra-depth footwear: Footwear constructed with additional depth and volume in order to accommodate deformity such as claw/hammer toes and/or to allow for space for a thick insole. Usually a minimum of 5 millimetres (~3/16”) depth is added compared to off-the-shelf footwear. Even greater depth is sometimes provided in footwear that is referred to as double depth or super extra-depth.
Foot deformity: Alterations or deviations from normal shape or size of the foot, such as hammer toes, mallet toes, claw toes, hallux valgus, prominent metatarsal heads, pes cavus, pes planus, pes equines, or results of Charcot neuro-osteoarthropathy, trauma, amputations, other foot surgery or other causes. Also includes limited joint mobility in the foot and/or ankle (21).
Foot-related exercises: Any physical exercise specifically targeting the foot or lower-extremity with the aim of changing foot function. These exercises can include stretching and strengthening of the foot and ankle musculature and functional exercises such as balance and gait training. These exercises are provided and/or supervised by a physical therapist or a similarly adequately trained healthcare professional.
Foot self-care: Foot care interventions the person with diabetes can do at home, consisting of but not limited to: foot inspection, washing of feet, careful drying between the toes, nail cutting, using emollients to lubricate skin, not using chemical agents or plasters to remove callus, footwear inspection, avoidance of walking barefoot or on socks only or in thin-soled slippers, avoidance of wearing tight socks, avoiding exposure to excessive cold and heat.
Foot self-management: Advanced assistive interventions the person with diabetes can use at home, consisting of but not limited to: home monitoring systems, lifestyle interventions, telemedicine, technological applications, peer support programs.
Footwear: defined broadly as any shoe-gear and including insoles.
Footwear modification: Modification to existing footwear with an intended therapeutic effect, e.g. pressure relief.
Hosiery: Stockings or socks of any kind. See further Stockings or Socks.
In-shoe (semi-)rigid orthosis: Term used for device put inside the shoe to achieve pressure reduction or alteration in the function of the foot. Can be pre-fabricated or custom-made.
Limited joint mobility: Reduced mobility of the joints of the foot, including the ankle, caused by changes in joints and associated soft tissues (21).
Medical grade footwear: Footwear that meets the specific needs of a person. Can be either prefabricated (see “Pre-fabricated medical grade footwear”) or custom-made (see “Custom-made medical grade footwear”). Also known as pedorthic footwear
Off-the-shelf footwear: Readily available footwear that has not been modified and has no intended therapeutic functions. Preferred term is pre-fabricated footwear.
Pre-fabricated medical grade footwear: Pre-fabricated footwear that meets the specific needs of a person, on the basis of footwear that provides extra depth, multiple width fittings and features designed to accommodate a broader range of foot types. Other features may include modified soles, fastenings and smooth internal linings. This type of footwear is usually available at specialty shoe shops.
Pre-fabricated insole: An “off-the-shelf” flat or contoured insole made without reference to the shape of the patient’s foot.
Shoe last: Last used to make footwear. The upper of the footwear is moulded or pulled over the last. The last shape defines the footwear shape including the outsole shape, heel pitch and toe spring. For off-the-shelf or pre-fabricated footwear generically generated lasts in different sizes are used.
Slipper: Low-cut, open type footwear that is easily slipped onto the foot. Includes thin-soled slippers and flip-flops (thongs).
Socks: Garment for the foot and lower part of the leg, typically knitted from wool, cotton, or nylon.
Stockings: Garment that fits closely over the foot and lower leg, typically elastic. Includes compression stockings for medical purposes.
Structured education: Any educational modality that is provided in a structured way. This can take many forms, such as one-to-one verbal education, motivational interviewing, educational group sessions, video education, booklets, software, quizzes, and pictorial education via animated drawing or descriptive images.
Therapeutic footwear: Generic term for footwear designed to have some therapeutic effect that cannot be provided by or in a conventional shoe. Custom-made shoes or sandals, custom-made insoles, extradepth shoes, and custom-made or prefabricated medical grade footwear are examples of therapeutic
Toe orthosis: an in-shoe orthosis to achieve some alteration in the function of the toe.
Weight-bearing activity: Activity during which the foot is loaded by supporting the body weight of the person, and expressed as quantitatively as possible. Incudes walking and standing.
CONFLICT OF INTEREST STATEMENTS
Production of the 2023 IWGDF Guidelines was supported by unrestricted grants from: Advanced Oxygen Therapy Inc., Essity, Mölnlycke, Reapplix, and Urgo Medical. These sponsors did not have any communication related to the systematic reviews of the literature or related to the guidelines with working group members during the writing of the guidelines, and have not seen any guideline or guideline-related document before publication. Full conflict of interest statements of all authors can be found online at www.iwgdfguidelines.org.
ACKNOWLEDGEMENTS
We would like to thank the following external experts for their review of our PICOs for clinical relevance: Lee Brentnall and Tom Fitzpatrick (Australia), Ingrid Ruys (the Netherlands), Jill Cundell (United Kingdom), Mieke Fransen (Belgium), Alfred Gatt (Malta), Yamile Jubiz (Colombia), Rajesh Kesavan (India), Elisabetta Iacopi (Italy), Jarmila Jirkovska (Czech Republic), Gerald Oguzie (Nigeria), Virginie Blanchett (Canada), James Ngoyo (Kenya), Sharad Pendsey (India), Heidi Corcoran (Hongkong), Simone McConnie (Barbados), Maimouna Mbaye (Senegal), Hermelinda Pedrosa (Brazil), as well as the patients Jane Cheney (Australia) and Ole Frejlev (Denmark).
AUTHOR CONTRIBUTIONS
SAB performed qualitative assessments, completed summary of judgements, and wrote recommendations for interventions 5 and 6, and wrote the manuscript. AnitaR and MMS performed qualitative assessments, completed summary of judgements, and wrote recommendations for interventions 1-3, and critically reviewed and edited the manuscript. LL and JvN performed qualitative assessments, completed summary of judgements, and wrote recommendations for clinical questions 5 and 8, and critically reviewed and edited the manuscript. JP performed qualitative assessments, completed summary of judgements, and wrote recommendations for clinical questions 4, 6, and 8, and critically reviewed and edited the manuscript. IS performed qualitative assessments, completed summary of judgements, and wrote recommendations for intervention 4, and critically reviewed and edited the manuscript. AnneR performed qualitative assessments, completed summary of judgements, and wrote recommendations for interventions 5 and 6, and critically reviewed and edited the manuscript.
SAB acted as chair of the working group and JvN as secretary and they take full responsibility for the content of the manuscript.
REFERENCES
(1) Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global Disability Burdens of DiabetesRelated Lower-Extremity Complications in 1990 and 2016. Diabetes Care. 2020;43(5):964-74.
(2) Lazzarini PA, Pacella RE, Armstrong DG, van Netten JJ. Diabetes-related lower-extremity complications are a leading cause of the global burden of disability. Diabet Med. 2018.
(3) Jupiter DC, Thorud JC, Buckley CJ, Shibuya N. The impact of foot ulceration and amputation on mortality in diabetic patients. I: From ulceration to death, a systematic review. International wound journal. 2016;13(5):892-903.
(4) Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995-1002.
(5) Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017;376(24):2367-75.
(6) Monteiro-Soares M, Boyko EJ, Ribeiro J, Ribeiro I, Dinis-Ribeiro M. Predictive factors for diabetic foot ulceration: a systematic review. Diabetes Metab Res Rev. 2012;28(7):574-600.
(7) Crawford F, Cezard G, Chappell FM, Murray GD, Price JF, Sheikh A, et al. A systematic review and individual patient data meta-analysis of prognostic factors for foot ulceration in people with diabetes: the international research collaboration for the prediction of diabetic foot ulcerations (PODUS). Health Technol Assess. 2015;19(57):1-210.
(8) Van Netten JJ, Sacco ICN, Raspovic A, Lavery LA, Monteiro-Soares M, Paton J, et al. Clinical and biomechanical effectiveness of foot-ankle exercise programs and weight-bearing activity in people with diabetes and neuropathy: a systematic review and meta-analysis. Diab Metab Res Rev. 2023;in press.
(9) Van Netten JJ, Raspovic A, Lavery LA, Monteiro-Soares M, Paton J, Rasmussen A, et al. Prevention of foot ulcers people with diabetes at risk of ulceration: a systematic review and meta-analysis. Diab Metab Res Rev. 2023;in
(10) Chen P, Vilorio NC, Dhatariya K, Jeffcoate W, Lobmann R, McIntosh C, et al. Guidelines on interventions to enhance healing of foot ulcers in people with diabetes (IWGDF 2023 update). Diab Metab Res Rev. 2023;in press.
(11) Bus SA, Armstrong DG, Crews RT, Gooday C, Jarl G, Kirketerp-Moller K, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2023 update). Diab Metab Res Rev. 2023;in press.
(12) Monteiro-Soares M, Hamilton EJ, Russell DA, Sirisawasdi G, Boyko EJ, Mills JL, et al. Guidelines on the classification of foot ulcers in people with diabetes (IWGDF 2023 update). Diab Metab Res Rev. 2023;in press.
(13) Fitridge R, Chuter VH, Mills JL, Hinchliffe RJ, Azuma N, Behrendt C-A, et al. The intersocietal IWGDF, ESVS, SVS guidelines on the diagnosis, prognosis and management of peripheral artery disease in patients with diabetes mellitus. Diab Metab Res Rev. 2023;in press.
(14) Senneville É, Albalawi Z, Van Asten SA, Abbas ZG, Allison G, Aragón-Sánchez J, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF/IDSA 2023). Diab Metab Res Rev. 2023;in press.
(15) Wukich DK, Schaper NC, Gooday C, Bal A, Bem R, Chabra A, et al. Guidelines on the diagnosis and treatment of active charcot neuro-osteoarthropathy in persons with diabetes mellitus (IWGDF 2023). Diab Metab Res Rev. 2023;in press.
(16) Bus SA, Lavery LA, Monteiro-Soares M, Rasmussen A, Raspovic A, Sacco ICN, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3269.
(17) Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ (Clinical research ed). 2016;353:i2089.
(18) Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924-6.
(19) Bus SA, Game F, Monteiro-Soares M, Van Netten JJ, Apelqvist J, Fitridge R, et al. Standards for the development and methodology of the 2023 International Working Group on the Diabetic Foot guidelines. Diab Metab Res Rev. 2023;in press.
(20) Jeffcoate WJ, Bus SA, Game FL, Hinchliffe RJ, Price PE, Schaper NC. Reporting standards of studies and papers on
the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet
Diabetes Endocrinol. 2016;4(9):781-8.
(21) Van Netten JJ, Bus SA, Apelqvist J, Chen P, Chuter VH, Fitridge R, et al. Definitions and criteria for diabetes-related foot disease (2023 update). Diab Metab Res Rev. 2023;in press.
(22) Schaper NC, Van Netten JJ, Apelqvist J, Bus SA, Fitridge R, Game F, et al. Practical guidelines on the prevention and management of diabetes-related foot disease. Diab Metab Res Rev. 2023;in press.
(23) Rayman G, Vas PR, Baker N, Taylor CG, Jr., Gooday C, Alder AI, et al. The Ipswich Touch Test: a simple and novel method to identify inpatients with diabetes at risk of foot ulceration. Diabetes care. 2011;34(7):1517-8.
(24) Sharma S, Kerry C, Atkins H, Rayman G. The Ipswich Touch Test: a simple and novel method to screen patients with diabetes at home for increased risk of foot ulceration. Diabetic medicine : a journal of the British Diabetic Association. 2014;31(9):1100-3.
(25) Waaijman R, de Haart M, Arts ML, Wever D, Verlouw AJ, Nollet F, et al. Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Diabetes Care. 2014;37(6):1697-705.
(26) Apelqvist J, Larsson J, Agardh CD. The influence of external precipitating factors and peripheral neuropathy on the development and outcome of diabetic foot ulcers. J Diabet Complications. 1990;4(1):21-5.
(27) Reiber GE, Vileikyte L, Boyko EJ, del Aguila M, Smith DG, Lavery LA, et al. Causal pathways for incident lowerextremity ulcers in patients with diabetes from two settings. Diabetes care. 1999;22(1):157-62.
(28) Coffey L, Mahon C, Gallagher P. Perceptions and experiences of diabetic foot ulceration and foot care in people with diabetes: A qualitative meta-synthesis. Int Wound J. 2019;16(1):183-210.
(29) Lavery LA, Hunt NA, Ndip A, Lavery DC, Van Houtum W, Boulton AJ. Impact of chronic kidney disease on survival after amputation in individuals with diabetes. Diabetes care. 2010;33(11):2365-9.
(30) Otte J, van Netten JJ, Woittiez AJ. The association of chronic kidney disease and dialysis treatment with foot ulceration and major amputation. J Vasc Surg. 2015;62(2):406-11.
(31) Game FL, Chipchase SY, Hubbard R, Burden RP, Jeffcoate WJ. Temporal association between the incidence of foot ulceration and the start of dialysis in diabetes mellitus. Nephrol Dial Transplant. 2006;21(11):3207-10.
(32) Fernando ME, Crowther RG, Pappas E, Lazzarini PA, Cunningham M, Sangla KS, et al. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: a metaanalysis of observational studies. PLoS One. 2014;9(6):e99050.
(33) Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, Buttner P, et al. Biomechanical characteristics of peripheral diabetic neuropathy: A systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Clinical biomechanics (Bristol, Avon). 2013;28(8):831-45.
(34) Barwick AL, van Netten JJ, Hurn SE, Reed LF, Lazzarini PA. Factors associated with type of footwear worn inside the house: a cross-sectional study. J Foot Ankle Res. 2019;12:45.
(35) Waaijman R, Keukenkamp R, de Haart M, Polomski WP, Nollet F, Bus SA. Adherence to wearing prescription custom-made footwear in patients with diabetes at high risk for plantar foot ulceration. Diabetes Care. 2013;36(6):1613-8.
(36) Keukenkamp R, Van Netten JJ, Busch-Westbroek TE, Bus SA. Custom-made footwear designed for indoor use increases short-term and long-term adherence in people with diabetes at high ulcer risk. BMJ Open Diabetes Research and Care. 2022;10(1).
(37) Price P. How can we improve adherence? Diabetes Metab Res Rev. 2016;32 Suppl 1:201-5.
(38) Calle-Pascual AL, Duran A, Benedi A, Calvo MI, Charro A, Diaz JA, et al. Reduction in foot ulcer incidence: relation to compliance with a prophylactic foot care program. Diabetes care. 2001;24(2):405-7.
(39) Viswanathan V, Madhavan S, Rajasekar S, Chamukuttan S, Ambady R. Amputation prevention initiative in South India: positive impact of foot care education. Diabetes care. 2005;28(5):1019-21.
(40) Wukich DK, Raspovic KM, Suder NC. Patients With Diabetic Foot Disease Fear Major Lower-Extremity Amputation More Than Death. Foot & ankle specialist. 2018;11(1):17-21.
(41) Rovers FJ, Van Netten JJ, Busch-Westbroek TE, Aan de Stegge WB, Bus SA. Adherence to at-Home Monitoring of Foot Temperatures in People with Diabetes at High Risk of Ulceration. Int J Low Extrem Wounds. 2022:15347346221114565.
(42) Stegge WBA, Van Netten JJ, Bus SA. Does the skin heat up before it breaks down in diabetic foot ulceration? Diabetes Metab Res Rev. 2023:e3621.
(43) Lavery LA, Higgins KR, Lanctot DR, Constantinides GP, Zamorano RG, Athanasiou KA, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care. 2007;30(1):14-20.
(44) Bus SA, Aan de Stegge WB, van Baal JG, Busch-Westbroek TE, Nollet F, van Netten JJ. Effectiveness of at-home skin temperature monitoring in reducing the incidence of foot ulcer recurrence in people with diabetes: a multicenter randomized controlled trial (DIATEMP). BMJ Open Diabetes Res Care. 2021;9(1).
(45) Wijlens AM, Holloway S, Bus SA, van Netten JJ. An explorative study on the validity of various definitions of a 2·2°C temperature threshold as warning signal for impending diabetic foot ulceration. Int Wound J. 2017;14(6):1346-51.
(46) van Netten JJ, Prijs M, van Baal JG, Liu C, van der Heijden F, Bus SA. Diagnostic values for skin temperature assessment to detect diabetes-related foot complications. Diabetes technology & therapeutics. 2014;16(11):714-21.
(47) Featherston J, Wijlens AM, van Netten JJ. Is a Left-to-Right >2.2°C Difference a Valid Measurement to Predict Diabetic Foot Ulceration in People with Diabetes and a History of Diabetic Foot Ulceration? Int J Low Extrem Wounds. 2021:15347346211062719.
(48) Frykberg RG, Gordon IL, Reyzelman AM, Cazzell SM, Fitzgerald RH, Rothenberg GM, et al. Feasibility and Efficacy of a Smart Mat Technology to Predict Development of Diabetic Plantar Ulcers. Diabetes Care. 2017;40(7):973-80.
(49) van Netten JJ, Lazzarini PA, Armstrong DG, Bus SA, Fitridge R, Harding K, et al. Diabetic Foot Australia guideline on footwear for people with diabetes. J Foot Ankle Res. 2018;11:2.
(50) Arts ML, Waaijman R, de Haart M, Keukenkamp R, Nollet F, Bus SA. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet Med. 2012;29(12):1534-41.
(51) Fernando ME, Crowther RG, Lazzarini PA, Sangla KS, Wearing S, Buttner P, et al. Plantar pressures are higher in cases with diabetic foot ulcers compared to controls despite a longer stance phase duration. BMC Endocr Disord. 2016;16(1):51.
(52) Bus SA, Waaijman R, Arts M, de Haart M, Busch-Westbroek T, van Baal J, et al. Effect of custom-made footwear on foot ulcer recurrence in diabetes: a multicenter randomized controlled trial. Diabetes Care. 2013;36(12):4109-16.
(53) Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR. Prevention of Recurrent Foot Ulcers With Plantar Pressure-Based In-Shoe Orthoses: The CareFUL Prevention Multicenter Randomized Controlled Trial. Diabetes Care. 2014;37(7):1982-9.
(54) Bus SA, Zwaferink JB, Dahmen R, Busch-Westbroek T. State of the art design protocol for custom made footwear for people with diabetes and peripheral neuropathy. Diabetes Metab Res Rev. 2020;36 Suppl 1(Suppl 1):e3237.
(55) Litzelman DK, Marriott DJ, Vinicor F. The role of footwear in the prevention of foot lesions in patients with NIDDM. Conventional wisdom or evidence-based practice? Diabetes Care. 1997;20(2):156-62.
(56) Rinkel WD, Fakkel TM, Castro Cabezas M, Birnie E, Coert JH. (Cost-)effectiveness of lower extremity nerve decompression surgery in subjects with diabetes: the DeCompression (DECO) trial-study protocol for a randomised controlled trial. BMJ Open. 2020;10(4):e035644.
(57) Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065-79.
(58) Lazzarini PA, Crews RT, van Netten JJ, Bus SA, Fernando ME, Chadwick PJ, et al. Measuring Plantar Tissue Stress in People With Diabetic Peripheral Neuropathy: A Critical Concept in Diabetic Foot Management. Journal of diabetes science and technology. 2019;13(5):869-80.
(59) Kooiman TJM, de Groot M, Hoogenberg K, Krijnen WP, van der Schans CP, Kooy A. Self-tracking of Physical Activity in People With Type 2 Diabetes: A Randomized Controlled Trial. Computers, informatics, nursing : CIN. 2018;36(7):340-9.
(60) Fernando ME, Woelfel SL, Perry D, Najafi B, Khan T, DuBourdieu C, et al. Dosing Activity and Returning to PreUlcer Function in Diabetic Foot Remission: Patient Recommendations and Guidance from the Limb Preservation Consortium at USC and The National Rehabilitation Center at Rancho Los Amigos. J Am Podiatr Med Assoc. 2021;111(5).
(61) van Netten JJ, Fijen VM, Bus SA. Weight-bearing physical activity in people with diabetes-related foot disease: A systematic review. Diabetes Metab Res Rev. 2022;38(6):e3552.
(62) Bus SA, van Netten JJ. A shift in priority in diabetic foot care and research: 75% of foot ulcers are preventable. Diabetes Metab Res Rev. 2016;32 Suppl 1:195-200.
(63) Skrepnek GH, Mills JL, Armstrong DG. Foot-in-wallet disease: tripped up by "cost-saving" reductions? Diabetes Care. 2014;37(9):e196-7.
(64) Marn Pernat A, Persic V, Usvyat L, Saunders L, Rogus J, Maddux FW, et al. Implementation of routine foot check in patients with diabetes on hemodialysis: associations with outcomes. BMJ open diabetes research & care. 2016;4(1):e000158.
(65) Schmidt BM, Wrobel JS, Munson M, Rothenberg G, Holmes CM. Podiatry impact on high-low amputation ratio characteristics: A 16-year retrospective study. Diabetes research and clinical practice. 2017;126:272-7.
(66) van Netten JJ, Sacco ICN, Lavery LA, Monteiro-Soares M, Rasmussen A, Raspovic A, et al. Treatment of modifiable risk factors for foot ulceration in persons with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36 Suppl 1:e3271.
(67) van Houtum WH, Rauwerda JA, Ruwaard D, Schaper NC, Bakker K. Reduction in diabetes-related lower-extremity amputations in The Netherlands: 1991-2000. Diabetes Care. 2004;27(5):1042-6.
(68) Carls GS, Gibson TB, Driver VR, Wrobel JS, Garoufalis MG, Defrancis RR, et al. The economic value of specialized lower-extremity medical care by podiatric physicians in the treatment of diabetic foot ulcers. J Am Podiatr Med Assoc. 2011;101(2):93-115.
(69) Van Netten JJ, Woodburn J, Bus SA. The future for diabetic foot ulcer prevention: A paradigm shift from stratified healthcare towards personalized medicine. Diabetes Metab Res Rev. 2020;36 Suppl 1:e3234.
(70) Keukenkamp R, Merkx MJ, Busch-Westbroek TE, Bus SA. An Explorative Study on the Efficacy and Feasibility of the Use of Motivational Interviewing to Improve Footwear Adherence in Persons with Diabetes at High Risk for Foot Ulceration. J Am Podiatr Med Assoc. 2018;108(2):90-9.
(71) McDonogh C, Nube VL, Frank G, Twigg SM, Penkala S, Holloway S, et al. Does in-shoe pressure analysis to assess and modify medical grade footwear improve patient adherence and understanding? A mixed methods study. J Foot Ankle Res. 2022;15(1):94.
(72) World Health Organization. Adherence to long-term therapies: evidence for action. Geneva, Switzerland 2003.
This article is excerpted from the 《The International Working Group on the Diabetic Foot》by Wound World.


