Despite the implementation of several pressure ulcer (PU) prevention programmes, the number of PUs continues to rise. In the UK, in 2012/2013, it was estimated that 153,000 adults had a pressure ulcer (Guest et al, 2015). By 2017/2018 this had number had risen to 202,000 PUs, representing an increase of 32% in 5 years (Guest et al, 2020), and adding to the already overloaded demand for NHS resources. In one 12-month period, using NHS costings from 2015/2016, Guest et al (2018) calculated the mean cost of treating a community-acquired PU was £8720 (range £1382/patient with a Category I PU to >£8500/patient with a Category II, III, IV or unstageable PU). If a PU remained unhealed after 12 months the cost equated to 2.4 times that of one that had healed (£5140/healed PU versus £12,300/ unhealed PU; Guest et al, 2018).
A challenge arising from the compromised blood supply to pressure damaged skin is a reduction in the availability of oxygen to the underlying tissues. Oxygen is critically important for wound healing processes, e.g., angiogenesis, revascularisation, synthesis of connective tissue, and resistance to infection (Castilla et al, 2012). Typically, wounds are hypoxic at their centre, with an increasing oxygen gradient towards the intact tissue (Bishop, 2008). Hypoxia may be due to an increased demand, as a result of the high metabolic activity of a healing wound but may also be affected by the partial oxygen pressure of the surrounding tissue and circulating blood supply, e.g., diffusive constraints due to prolonged pressure. Although, initially, hypoxia acts as a signal to stimulate the wound healing process, prolonged hypoxia is detrimental to healing progression (Chadwick et al, 2019, Gottrup et al, 2017). Chronic wounds have been shown to have a sustained oxygen deficit at the wound bed, with a concomitant detrimental effect on wound healing (Dissemond, 2015). The delivery of oxygen, either intrinsically from the blood supply, or extrinsically via oxygen therapy, to a chronic wound is therefore a vital therapy to facilitate wound healing progression.
Granulox®, a topical-based haemoglobin spray improves the oxygen supply to chronic wounds through simplified diffusion, so helping to stimulate wound healing. When Granulox is applied to the wound bed, the haemoglobin binds oxygen from the surrounding air and transports it to the wound bed where it diffuses into the cells. Clinical studies demonstrated that the addition of Granulox to the standard wound care procedure as compared with standard wound care alone in the treatment of hard-to-heal wounds (Hunt and Elg, 2017) and sloughy wounds (Hunt et al, 2018), including PUs, resulted in significant wound size reduction. In the first of these studies, 90% (45/50) of wounds receiving Granulox therapy in addition to standard care had healed by week 26 compared to 38% (19/50) of wounds receiving standard care alone (Hunt and Elg, 2017). These findings are consistent with those observed in the second study, i.e. at week 26, 94% (94/100) of wounds receiving Granulox therapy in addition to standard care had healed compared to 63% (63/100) of wounds receiving only standard care (Hunt et al, 2018). In addition, wounds treated with Granulox had reduced levels of slough, wound exudate, and pain. Using data from one of the clinical studies (Hunt ad Elg, 2017), Elg and Bothma (2019) demonstrated Granulox to be a cost-effective adjunctive therapy to standard wound care. Their analysis revealed that the total number of weeks healed was 874 in the intervention group and 278 in the control group. Despite the additional cost of Granulox, the total cost of dressings used was lower in the intervention group (£6953) compared with the control group (£9547; Elg and Bothma, 2019).
Taking these data into consideration, it was decided to introduce Granulox into the treatment regimen of a patient with a category IV, static sacral PU that had been present for 4 years. Research Ethics Committee (REC) approval for this case study was not deemed necessary, as it refers to standard clinical practice involving the use of products in line with the instructions for use supplied with them. Written informed consent to use the images in this article was obtained from the patient.
CASE REPORT
The 63-year-old female patient with Type II diabetes mellitus, who resided with her adult son (also with health needs) and was living with multiple sclerosis. She was bedbound, and despite constant advice from healthcare professionals of the need to frequently change position to relieve the pressure on the PU, she spent each day sitting up in bed. Pain increased when sitting but this was managed with mild analgesics prescribed by her doctor; sleep was not impacted by pain. Although the patient had a low quality of life, with feelings of loneliness and isolation, especially as she felt unable to take holidays, she showed no embarrassment for the wound itself, as due to its longevity, it had become the ‘norm’.
Throughout the 4 years, the care provided to the patient included regular PU prevention advice, the provision of pressure relieving equipment (Hybrid air mattress, ToTo lateral turning platform), and treatment using a large range of conventional dressings, for example, Aquacel, Cutimed, Flaminal, and basic wound packing dressings. To the frustration of both the patient and the nursing staff, all the dressings that were tried failed to promote wound healing. In addition, although the dressings successfully managed the consistently high wound exudation, maintaining dressing attachment was a challenge due to persistent faecal incontinence and catheter bypassing, adding to the tendency towards maceration of the periwound region. Consequently, the nurses were resigned to the fact that the wound would never heal, and the patient expressed that she was ‘fed up’ with the on-going wound care, especially with the failure to see any change in the condition of the wound. She voiced to the nursing staff that she had ‘had enough’, raising serious concerns over her mood and mental health. At this point of low expectation, it was decided to introduce Granulox into the treatment regimen. However, there were mixed thoughts concerning the use of this product, especially as none of the previously used dressings or wound care products had led to an improvement in the wound’s condition. The patient was open to trying new treatments and was excited to start using Granulox.
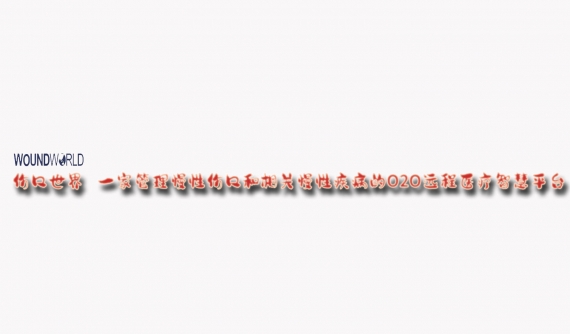
Immediately before commencing Granulox treatment, the pressure ulcer measured 32.2cm2 with a depth of 1.0cm (Figure 1). Although the wound bed was composed of 100% granulating tissue, areas appeared hypotrophic indicating a reduction in the blood supply to the tissue. Wound exudate levels were high, but non-viscous and clear/serous in appearance. The periwound skin was macerated, a possible consequence of the high exudation and incontinence problems. A wound infection was suspected as the patient had indicated an increased level of wound pain, especially during the dressing change procedure. Using a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (maximum pain ever), the patient rated pain before dressing removal and during dressing removal as 5 and 10, respectively. The patient was visited four times each day by a domiciliary carer who attended to patient repositioning and personal care, and she received daily visits from a community nurse who performed wound dressing changes, according to local clinical practice. The wound dressings used were AquacelAg (antimicrobial hydrofiber dressing) and Tegaderm (polyurethane foam dressing). Cavilon Film Spray (alcohol-free liquid barrier film) was applied as a skin protectant to the periwound region.
With the aim of increasing the level of oxygen available to the wound bed tissues, the topical haemoglobin spray, Granulox, was introduced A thin film of Granulox was applied to the wound bed tissue of the PU that was then dressed using Aquacel ribbon (cut to size) followed by Tegaderm. On the initial application of the Granulox a VAS score of 10 was recorded. Daily dressing changes continued to be performed by community nurses, and a Tissue Viability Nurse (TVN) visited the patient each week to review the treatment protocol. Domiciliary carers continued to attend four times daily. At four of the dressing changes (treatment days 21, 42, 77, and 98), a detailed assessment of the condition of the wound was performed (Figures 2–5).

After just a few applications of Granulox, and despite the patient still spending all day sitting on the wound, the nurses started to see a positive change in its condition, where for the previous 4 years there had been none. At the initial study assessment, after 21 days of the study treatment regimen, the wound measured 26cm2 , a reduction in size of 19.3%. This provided a glimmer of hope to the nursing staff and especially the patient, who’s mood was lifted. Her positivity was increased, and she had attempted to get out of the bed into a chair. The improvement in the wound continued and, after a further 21 days of Granulox application, the depth of the wound was reduced by 50% to 0.5cm, wound exudation was reduced to moderate, and the patient reported a reduction in dressing-change related pain (VAS scores of 5 were recorded at dressing removal and on re-application).
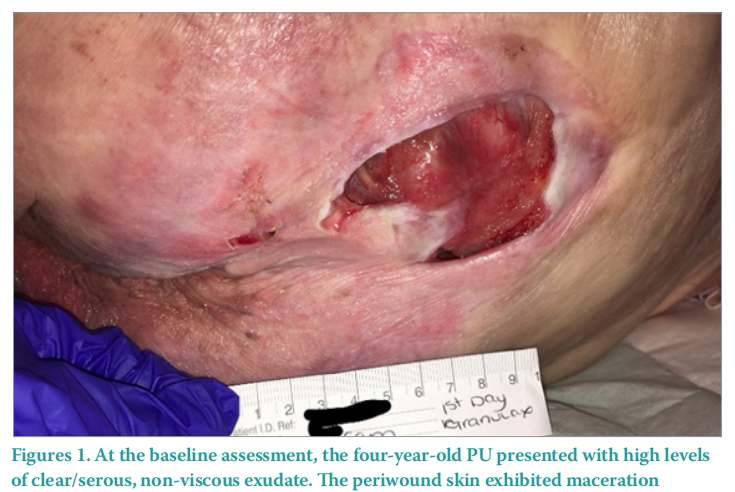
The size of the wound continued to decrease, and after 77 days of Granulox application, the wound area had reduced by 31.7% to 22cm2 , (Figure 4, Figure 6). In addition, wound-related pain was absent, indicating the resolution of clinical wound infection. At this point, the TVN considered that Granulox had completed its objective, so treatment with Granulox was discontinued. The wound was continued to be dressed daily using Aquacel and Tegaderm.
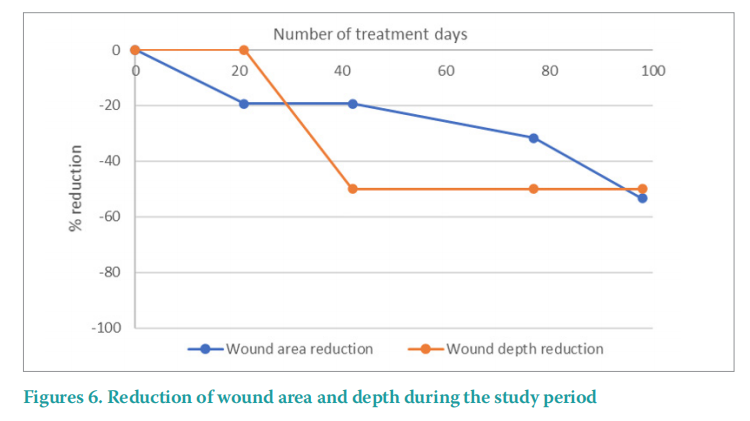
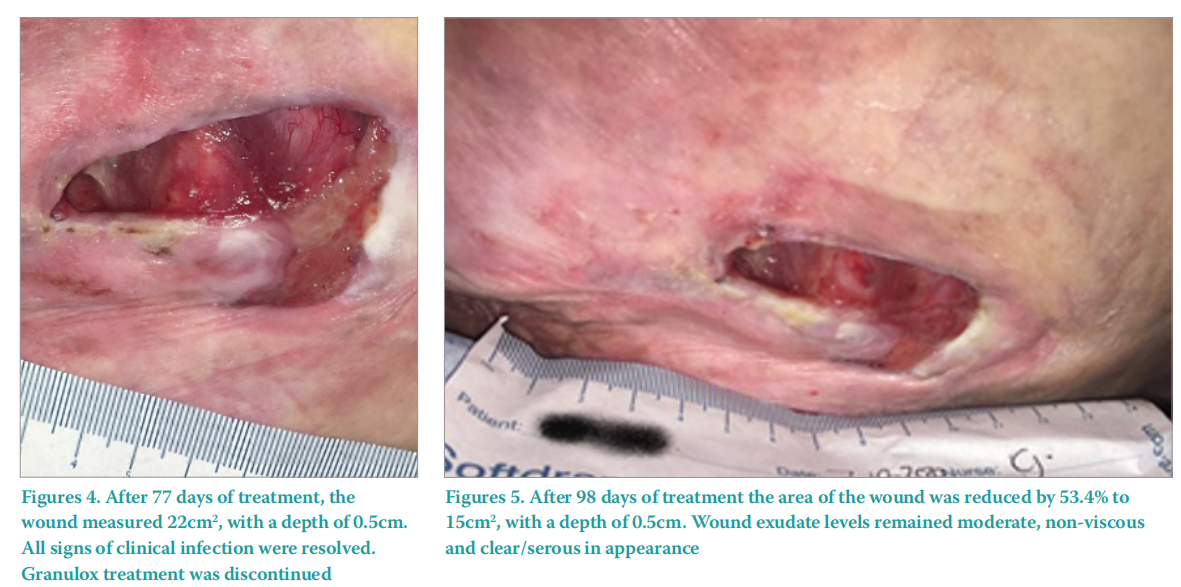
Following the discontinuation of Granulox, the wound continued along the healing trajectory and, after a further 21 days of treatment, had reduced by a further 7cm2 to 15cm2 , an overall reduction in wound area of 53.4% (Figure 5–6). The wound bed tissue was consistent throughout (100% granulating tissue), at the final assessment due to a wound infection 5% sloughy tissue was observed. Following treatment for the infection, Granulox was re-applied to the wound bed to facilitate the healing once again.
After the initial reduction in wound exudate, the levels were unchanged; exudate appearance was non-viscous and clear/serous throughout the study. Maceration of the periwound skin failed to be resolved, possibly because of the continued problems of faecal incontinence and catheter bypassing.
After the study had ended, wound treatment continued unchanged, and after a further 56 days the wound had reduced by 76.6% of its original size to 7.5cm2 (Figure 7). The patient was excited and making plans for her future, including the planning of a much longed for holiday.

DISCUSSION
The use of the topical haemoglobin spray, Granulox resulted in the significant improvement of a stalled PU of 4 years duration, bringing relief to the patient. The nursing staff found Granulox an easy product to apply, and considered it a product that would lend itself to self-application by a patient. They were surprised at how quickly Granulox positively influenced the condition of wound, especially how the wound continued along the healing trajectory after the application of Granulox was stopped. Both woundrelated and dressing change-related pain were reduced, allowing pain control measures to be reviewed, and importantly the patient’s quality of life was improved, as she managed to take a much longed for holiday.
As case studies generate descriptive, nonexperimental clinical evidence, they are considered to represent the lowest level in the so-called hierarchy of evidence. On the other hand, case reports are highly valued by those involved in the provision of wound care-related training and education. This article is a classic example of how a case report can provide an indepth review of the challenges that complex wounds pose to healthcare providers, patient and their families and how those challenges can be overcome through thorough wound assessment and implementation of appropriate care regimes, i.e. things that may not be captured in the larger studies (e.g. randomised controlled trials) that are undertaken to evaluate wound care interventions.
REFERENCES
1. Bishop A (2008) Role of oxygen in wound healing. J Wound Care 17(9): 399–402. https://doi.org/10.12968/jowc.2008.17.9.30937
2. Castilla D.M, Lui Z-J, Velazquez OC (2012) Oxygen: Implications for wound healing. Adv Wound Care (New Rochelle) 1(6):225–30. https://doi. org/10.1089/wound.2011.0319
3. Chadwick P, Edmonds M, Fox A et al (2019) Expert panel report. The role of topical oxygen therapy in the management of diabetic foot ulcers. Diabetic Foot Journal. https://tinyurl.com/3uxtz8cd (acessed 31 May 2022)
4. Dissemond J, Kröger K, Storck M et al (2015) Topical oxygen wound therapies for chronic wounds: a review. J Wound Care 24(2):53–63. https://doi. org/10.12968/jowc.2015.24.2.53
5. Elg F, Bothma G. (2019) Cost-effectiveness of adjunct haemoglobin spray in the treatment of hard-to-heal wounds in a UK NHS primary care setting. J Wound Care 28(12):844–49. https://doi.org/10.12968/ jowc.2019.28.12.844
6. European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP), Pan Pacific Pressure Injury Alliance (PPPIA) (2019) Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Haesler E (ed)
7. Gorecki C, Nixon J, Madill A et al (2012) What influences the impact of pressure ulcers on health-related quality of life? A qualitative patientfocused exploration of contributory factors. J Tissue Viability 21(1):3–12. https://doi.org/10.1016/j.jtv.2011.11.001
8. Gottrup F, Dissemond J, Baines C et al (2017) Use of oxygen therapies in wound healing. J Wound Care 26(5 Supplement):S1–42. https://doi. org/10.12968/jowc.2017.26.sup5.s1
9. Guest JF, Ayoub N, McIlwraith T et al (2015) Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 5:e009283. https://doi.org/10.1136/bmjopen-2015-009283
10. Guest JF, Fuller GW, Vowden P et al (2018) Cohort study evaluating pressure ulcer management in clinical practice in the UK following initial presentation in the community: costs and outcomes. BMJ Open 8(7):e021769. https://doi.org/10.1136/bmjopen-2018-021769
11. Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 10(12):e045253. https://doi.org/10.1136/ bmjopen-2020-045253
12. Hunt S, Elg F. (2017) The clinical effectiveness of haemoglobin spray as adjunctive therapy in the treatment of chronic wounds. J Wound Care 26(9):558–68. https://doi.org/10.12968/jowc.2017.26.9.558
13. Hunt SD, Elg F, Percival SL (2018) Assessment of clinical effectiveness of
14. haemoglobin spray as adjunctive therapy in the treatment of sloughy wounds. J Wound Care 27(4):210–19. https://doi.org/10.12968/ jowc.2018.27.4.210
15. National Health Service (NHS) Improvement (2018) Pressure ulcers: revised definition and measurement. Summary and recommendations. https:// tinyurl.com/24kpwv9k (accessed 31 May 2022)
16. National Pressure Injury Advisory Panel (NPIAP). Pressure injury stages https://npiap.com/page/PressureInjuryStages (accessed 31 May 2022)
DECLARATION OF INTEREST:
This article was funded by an educational grant from Mölnlycke Health Care
ACKNOWLEDGEMENT:
The author would like to thank Nevis Scientific Services for its support in writing this article
This article is excerpted from the Wounds UK | Vol 18 | No 2 | 2022 by Wound World.