Hard-to-heal wounds develop due to an interruption in the body’s natural healing process. It is accepted that within the normal healing trajectory, wounds should re-epithelialise within 4 weeks (Vowden and Vowden, 2016) or see a wound reduction of 20-40% after 2–4 weeks of optimal therapy (Leaper and Durani, 2008). From a patient perspective, living with a hard-to-heal wound can often mean experiencing a decrease in quality of life with the potential of increased pain and anxiety (Olsson et al, 2019).
The associated cost of these wounds and the burden they represent on both health outcomes and budgets is widely recognised across the NHS in the United Kingdom (Guest et al, 2017a) and internationally (Olsson et al, 2019). Specifically, in the UK, an average Clinical Commissioning Group (or equivalent) cared for an estimated 11,200 wounds in 2013; with prevalence growing by 9–13% per annum. In reality, this approximation sits at a 71% increase in the annual prevalence of wounds between 2012/2013 and 2017/2018 (Guest et al, 2020). Thirty per cent of all wounds are unhealing, and these disproportionately represent 67% of the total wound expenditure. This continued burden is set to be equally challenging not only for the newly commissioned NHS Integrated Care Boards, but also for other healthcare establishments globally.
Early identification of a wound that is not healing and its subsequent treatment is key to achieving successful outcomes for the patient and a cost-effective service (Guest et al, 2017b). Furthermore, unwarranted, marked variations in care in clinical practice (Gray et al, 2018), an ageing population with multiple comorbidities, complicated access to resources and a worrying lack of community nurses, mean there has never been a more opportunistic time to review current hard-to-heal wound care practice.
Understanding the burden that these wounds have on both clinical outcomes and healthcare resources is crucial for today’s clinical practitioners. Clinical effectiveness, the patient’s quality of life and the cost of wound treatment all need to be balanced in today’s target- driven climate. Over the past two decades, advances in technology, along with an increased understanding of wound bed preparation and frameworks of assessment, have encouraged clinicians to develop approaches that maximise wound healing (Harries et al, 2016).
Despite more complex patients often presenting with multiple comorbidities, wound care clinical practice should in theory have seen a reduction in the number of hard-to-heal wounds across the UK. However, recent evidence shows that this is simply not the case (Guest et al, 2020).
A growing body of evidence has discussed the benefits of using PICOTM single-use Negative Pressure Wound Therapy (sNPWT) to treat hard-to-heal wounds as part of an early intervention strategy (Hurd et al, 2014; Dowsett et al, 2017; McCluskey et al, 2020; Hughes et al, 2021). PICO sNPWT involves the controlled application of sub-atmospheric pressure to a wound, using a sealed wound dressing connected to a vacuum pump (Smith and Nephew, 2020a). PICO sNPWT is a canister-free single-use system that offers portable NPWT and has a unique air lock layer, which enables consistent negative pressure to be delivered across the full surface of the dressing — providing therapy not only to the wound, but also to the periwound area (Smith and Nephew, 2020b).
The mode of action for sNPWT on hard-to-heal wounds are reported as an increase in blood flow to the wound, reduction of local tissue oedema, and removal of fluid and bacteria from the wound bed (Schwartz et al, 2015). It has the potential, therefore, to actively treat the wound rather than simply manage the symptoms (Schwartz et al, 2015). Despite the reported health economic and clinical benefits, the view that sNPWT is a costly treatment remains one of the key barriers to use. This long-held belief has been challenged as a result of reported improved healing rates and a reduction in clinician time, which can positively impact the local health economy (Dowsett et al, 2017).
Reflecting on the financial pressures faced by the NHS in recent years, it is understandable that the cheapest solution can often be seen as the ‘best solution’ for managing local healthcare budgets. However, the cheapest option is not always the best way to reduce costs. This particularly resonates in wound care, because it is not merely the cost of the dressing that needs to be considered, but also the nursing resource required to care for these wounds, which can account for as much as 85% of the total expenditure (Lindholm and Searle, 2016). Without acknowledging the associated wound care resources, this can quickly become the very antithesis of what is trying to be achieved. Greater value can potentially be achieved by helping the wound to progress to healing, resulting in improved clinical and cost outcomes.
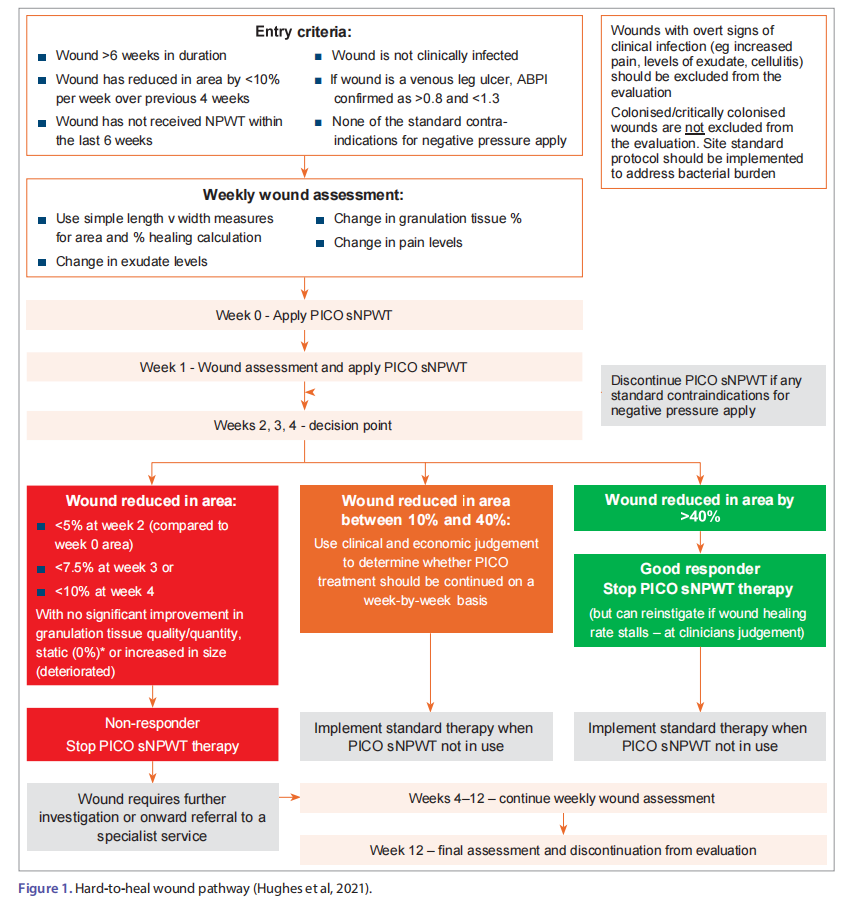
This multi-centre 323-patient service evaluation builds on the previous work of Dowsett et al (2017). A hard-to-heal wound pathway [Figure 1] was used in practice for a community patient cohort with hard-to-heal wounds.
Methods
Data were collected as part of an in-service evaluation of PICO sNPWT and were captured from 17 sites across Denmark, Ireland, Sweden and the United Kingdom between 2016 and 2022. Clinicians were trained on how to use the pathway to ensure consistency, and patients were selected according to the entry criteria on the pathway:
■ Wound >6 weeks in duration
■ <10% wound reduction over 4 weeks
■ Wound has not received NPWT within the last 6 weeks
■ Wound is not clinically infected
■ If the wound is a venous leg ulcer, the ankle brachial pressure index confirmed as >0.8 and <1.3
■ None of the standard contraindications for negative pressure apply.
PICO sNPWT device was initiated for all eligible patients in line with the hard-to-heal pathway [Figure 1]. Data were collected using two similar forms: a longer form (between 2015 and 2017) with baseline and longitudinal data designed for prospective collection, and a shorter form (between 2018 and 2022), which retrospectively captured wound progression over the evaluation period.
In all instances, data were collected weekly from primary application of sNWPT until the wound healed or up to 12 weeks, whichever came first. Data collection forms included wound size and area, wound characteristics, dressing change frequency, and patient and clinician feedback using the sNPWT device. Wound area was calculated using the formula for area of an ellipse, and wounds were considered healed once the wound reached a calculated area of 0cm2.
Data were collected via digital forms or paper forms transcribed into the digital system. All data were stored in a secure environment compliant with ISO27001. No patient identifiable variables were captured at any stage of the evaluation. Due to this and the nature of in-service evaluation, ethics considerations were not applicable; however, in each centre, full consent and approvals were sought and granted prior to any data collection as deemed necessary.
All data were analysed using Microsoft Excel. Frequency counts were conducted for each pertinent variable. Wounds were analysed for both healed and non-healed, time to healing (when applicable), duration of sNPWT usage and dressing change frequency throughout the differing phases of the evaluation. Comparisons of proportion of healing per feature of the wound were made using chi-square testing.Comparison of means for healing duration and duration of sNPWT treatment were performed using a two-sample T-test.
Economic model development
The data were used to develop an economic model to estimate the impact of using the PICO sNPWT device compared to standard care on material and nursing costs over 12 weeks. In this model, the following estimations were made:
■ Dressing change was estimated at 31 minutes
■ Standard care costs were estimated at £9.18* per change (standard care costs were determined by data captured at week 0, which included dressings used and dressing change frequency)
■ Cost per week of PICO sNPWT was estimated at £164.89
■ Nursing cost per change (standard care and PICO sNPWT phase) was estimated at £29.28†.
A baseline costing was estimated assuming none of the 323 wounds would heal within 12 weeks without sNPWT initiation and that dressing change frequency prior to sNPWT would have remained consistent had the patient remained on standard care. After the evaluation, data on time to healing, average weekly dressing change frequencies during and post sNPWT use, and duration of sNPWT use were used to calculate comparative material and nursing costs for the evaluation. The baseline economic estimate was compared to the post-evaluation estimate was to measure the economic impact of the 12-week evaluation.
Results
Wounds characteristics
Data were collected on 323 patients with 323 wounds who received PICO sNPWT as per the hard-to-heal pathway during the period from 2016 to 2022 in 17 centres [Table 1]. Open surgical wounds were the most frequent wound type (30.7%; n=99).
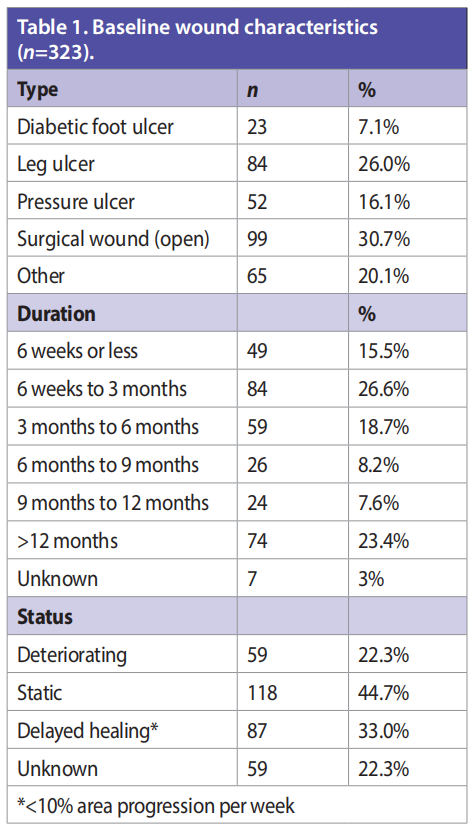
In terms of wound duration, 42.1% of wounds had a duration of less than 3 months and 23.4% of wounds were over a year old at time of treatment. The estimated mean wound duration at time of application was 26.5 weeks.
Over two thirds of the wounds presented were considered static (44.7%) or deteriorating (22.3%). The remaining third of wounds were described as having delayed healing (defined as <10% area progression per week).
Healing outcomes
Over the evaluation, more than half of the wounds (52%; n=168) healed, 40.6% (n=131) wounds progressed and 7.4% (n=24) did not respond. Among the wounds that progressed but did not fully heal, there was an average weekly percentage wound reduction of 8.0%.
Healing was observed to be most likely in surgical wounds, where over two thirds (66.7%) healed within the 12 weeks. Leg ulcers and pressure ulcers were less likely to heal (39.3%, 34.6% respectively; Table 2).
Significantly, the likelihood of complete healing reduced in line with the wound’s duration at commencement of sNPWT: with 63.0% of wounds under 6 months old healed compared to 28.4% of wounds greater than a year old (p<0.01, chi-square test; Table 2).
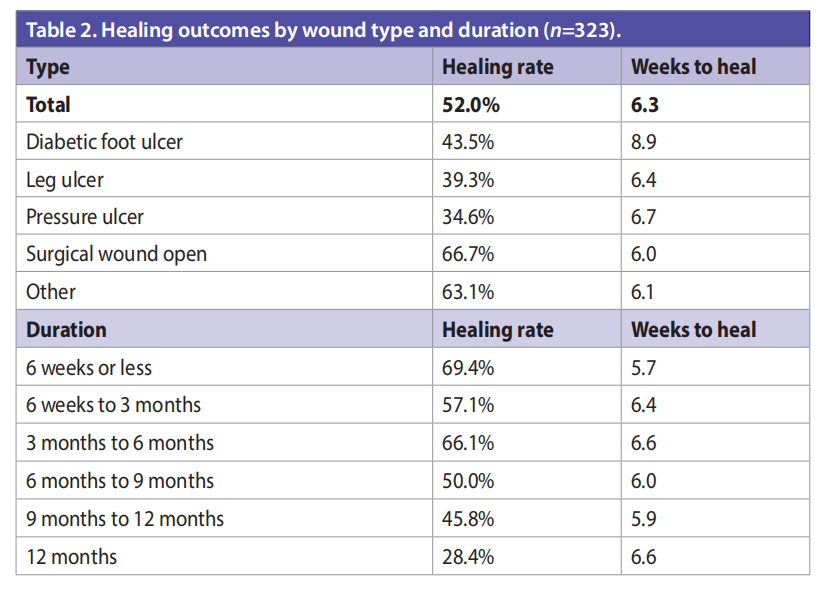
Healthcare resources and durations
sNPWT was used for an average duration of 3.3 weeks during the 12-week period. No significant variation in the duration of use of sNPWT was identified in relation to wound type or duration. When the wound healed, on average this occurred 6.3 weeks after commencement with sNPWT [Table 2]. It was observed that diabetic foot ulcers took significantly longer to heal than the ‘other’ wound aetiologies (8.9 weeks versus 6.1 weeks respectively; p<0.01; Table 2). No significant differences in healing time for the wounds that healed were observed when analysed using wound duration or status at the start of sNPWT.
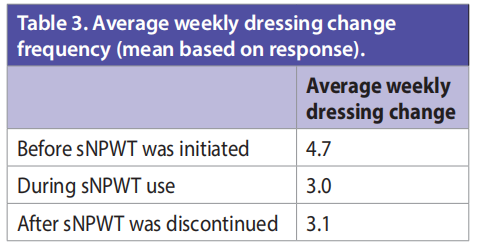
Clinicians documented weekly dressing change frequency before, during and after use with sNPWT. There was an approximate third reduction of a third of dressing changes between the pre- and during phase. After sNPWT use, weekly dressing change was 3.1, which is similar to when sNPWT was in use [Table 3].
Economic evaluation
If standard care was used without following the hard-to-heal pathway or sNPWT across the 323 patients in the 12-week evaluation, the estimated total cost would be £700,634. The model suggests that the estimated material costs of wound management would be £167,234 and estimated nursing costs would be £533,400 [Figure 2].
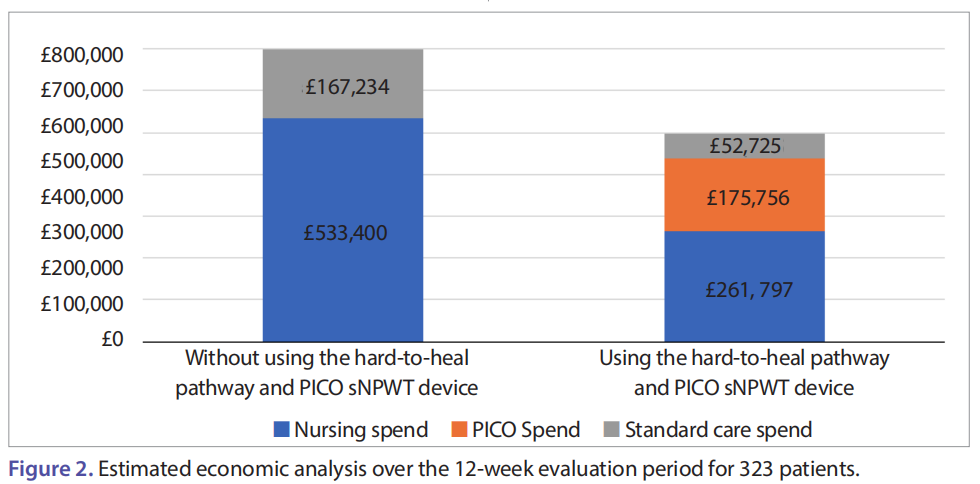
During the 12-week period following the hard-to-heal pathway and using PICO sNPWT, the total spend was estimated to be £490,278: standard care costs were £52,725, the PICO sNPWT intervention was estimated to cost £175,756, and nursing spend was estimated at £261,797, with estimated standard care costs reducing to £52,725.
In the baseline estimate, the nursing spend accounted for an estimated 18,000 dressing changes; during the 12-week evaluation, there were 8,941 dressing changes, equating to a 50.9% reduction in the number of dressing changes. The reduction in dressing changes is estimated to release 4,792 nursing hours (approximately 200 days or 28.5 weeks). Therefore, the associated nursing cost for using sNPWT would be £261,797.
It can be surmised that by using the hard-to-heal pathway and PICO sNPWT over the 12-week period, there was the potential to reduce costs by 30%. The model suggests that there could be a saving of £651 per patient (from £2,169 to £1,518).
Product feedback
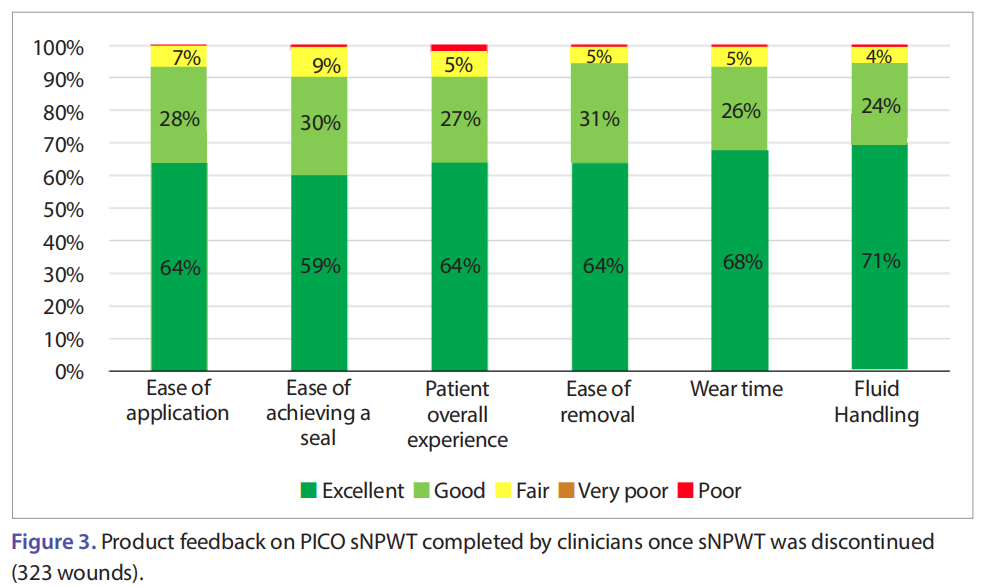
Clinicians were asked to complete feedback on their experience of using the PICO sNPWT device either once the wound had healed or at 12 weeks, whichever came first. All sections of the feedback were completed for each of the 323 wounds. On average for the six parameters evaluated, 93% of product feedback for the PICO sNPWT device was rated as better than ‘fair’, and 65% of overall feedback was rated as ‘excellent’ [Figure 3]. In total, 91% of the completed evaluations rated the patient’s overall experience as ‘good’ or ‘excellent’. The ease of achieving a seal was rated as ‘good’ or ‘excellent’ in 89% of the completed evaluations.
Discussion Validation of the hard-to-heal pathway
Clinical pathways have been used in practice for many years and are seen as a tool to not only improve quality across patient services (Deneckere et al, 2012), but also support teams to implement evidence-based interventions that have the potential to reduce variations in practice (Latina et al, 2020). However, without measuring and validating their impact on both the service and patient in practice, it is difficult to truly know the extent of their success in quality improvement strategies. The work of the National Wound Care Strategy Programme in the UK and the focus on best practice clinical pathways will no doubt go some way to mitigating these disparities. Furthermore, with the advent of value-based healthcare, the focus of validated clinical pathways also needs to demonstrate reduced cost and resource (Seys et al, 2021). As part of this multi-centre evaluation, the hard-to-heal pathway was validated on its impact on clinical and health economic outcomes, and the effectiveness of the clinical decision points. The data set presented suggests that the hard-to-heal pathway had positive outcomes for the validation points investigated. This included how often to re-assess and optimising sNPWT use according to stages of healing by following the coloured clinician decision boxes.
The impact of early intervention on healing outcomes and consideration of the impact of wound aetiology
Successful outcomes for patients with a hard-to-heal wound are founded on accurate assessment and identification of the wound aetiology, alongside consideration of both local and systemic factors that may be contributing to poor wound healing (Werdin et al, 2009). Wounds that appear to be moving away from a normal healing trajectory despite receiving optimal care should be, as part of best practice, referred to a healthcare practitioner with specialist skills to allow for the best clinical outcomes for the patient (Shamsian, 2021).
The data set presented here confirms previous studies that if sNPWT is applied at the early stages of a wound’s duration, significantly improved healing can be achieved (Hurd et al, 2014; Dowsett et al, 2017; McCluskey et al, 2020; Hughes et al, 2021).
In terms of wound aetiology, it is not surprising that leg ulcers and pressure ulcers were the most difficult to heal (39.3% and 34.6%, respectively). Venous leg ulcers due to a complicated pathophysiology and issues with incorrect or delayed diagnosis can become recalcitrant in nature, with a high percentage recurrence rate (Raffetto et al, 2021). These complexities can often mean that venous leg ulcers do not heal within the best practice 12-week timeframe (Wounds UK, 2019).
Likewise, pressure ulcers are equally challenging due to a variety of intrinsic and extrinsic factors. Diabetic foot ulcers took significantly longer to heal than ‘other’ wound aetiologies (8.9 versus 6.1 weeks; p<0.01), and although the definitive reason for this is unknown, the authors suggest the delay in healing could potentially be due to ischaemia and walking pressure issues.
If improved clinical and health economic outcomes are to be realised, then early identification and subsequent treatment of a hard-to-heal wound should be at the forefront of wound assessment. Reassessment of wounds is crucial for those wounds that fail to achieve sufficient healing after 4 weeks of standard care, considering underlying pathology (Frykberg and Banks, 2015). However, potential changes in treatment following reassessment, such as the introduction of advanced therapies that could help kick start the wound, are often not considered. Sub-optimal care not only impacts on delayed healing and the development of wound complications, but also increases the requirement of wound care resources and spend (Johnson, 2017). Data from the evaluation demonstrates that healing outcomes are dependent on the duration of the wound when sNPWT is first initiated [Table 2]. The earlier the hard-to-heal wound is treated with sNPWT, the better the outcome for both healing rates and the associated health economic burden.
Additionally, the impact on the patient who is living with a wound can be profound. Living with a wound long-term can have a significant impact on anxiety and depression levels, which can themselves be precursors to poor nutrition and hygiene and lack of sleep, further impacting the hard-to-heal wound (Augustin et al, 2012).
The ability of sNPWT to kick-start the wound onto a healing trajectory; the clinical outcomes seen in the data, in terms of total healing (52%) and weekly reduction in wound area (8%) in wounds that had been static or deteriorating, suggests that sNPWT facilitated the progression of the wound healing. In addition, the observed reduction in average weekly dressing from before to during sNPWT use correlates with increased healing rates.
Following sNPWT use, the average weekly dressing change did not return to pre-sNPWT frequency, which suggests that the healing trajectory was maintained in the absence of sNPWT. A reduced dressing change frequency supports undisturbed wound healing — which, although a relatively new concept, is gaining traction across wound care practice (Rippon et al 2012; Wiegand et al, 2015; Davies et al, 2019). Undisturbed wound healing involves maximising the wound’s healing capacity without interrupting the healing process and protecting the wound from trauma and contamination potentially leading to infection (Davies et al, 2019).
The impact on nursing resource and the health economy
In the UK, it is well verbalised that the community/homecare clinician workforce is facing pressure like never before. An ageing nurse population set to retire over the next 10 years, workplace shortages and down banding of nursing roles are seen to be the major force behind these pressures (Fields et al, 2015; Royal College of Nursing, 2014; Drennan and Ross, 2019). Strategies and investments in services need to be considered if these pressures are to be managed in the face of an increasingly older patient population with multiple complexities and comorbidities. The economic model devised from the data suggests that using the hard-to-heal pathway to implement PICO sNPWT in clinical practice, an estimated 4,792 of nursing hours could be released with an estimated intervention cost reduction of £271,603.
Limitations
The findings from this service evaluation should be considered in conjunction with some limitations. It is important to note that the data collection did not capture what wound care plan was in place before using sNPWT and what steps had been taken to optimise the patient and wound for healing; therefore, it is not possible to attribute the improved healing rates to the effect of sNPWT in every case.
The absence of bias and consistency cannot be fully excluded, as full autonomy over the wound care episode for each patient lay with the clinician. Standardising nursing cost and time across international systems can be problematic due to variations in practice. Likewise, the distribution of type and number of wounds may affect the estimated cost models.
Recommendations
The authors believe that due to this body of practice-based data, it would be timely to revise the hard-to-heal pathway and include some additional patient factors and history. Knowledge of whether the wound had been optimised in terms of treatment prior to and during sNPWT application would help to promote standardised wound care practice. Additionally, consideration of the patient’s comorbidities could potentially help to identify the impact of said complexities on healing rates. Finally, it would be valuable to capture the impact that living with a wound has on a patient’s quality of life as part of the hard-to-heal pathway. While improved clinical and budget outcomes are vital for today’s service leads, a continued effort is required to ensure the best possible patient experience.
Conclusion
The burden of hard-to-heal wounds on community caseloads and the associated fiscal cost is becoming more of a challenge for healthcare providers. Larger sets of practice-based evidence can provide insights into ways of working that can be beneficial for both the patient, the wound and the health economy. Understanding and recognising when a wound is not on a favourable healing trajectory should be a call to action for healthcare practitioners to change treatments to ensure patients are not living with a wound for any longer than they need to.
References
1. Augustin M, Carville K, Clark M et al (2012) International Consensus. Optimising wellbeing in people living with a wound. An expert working group review. London: Wounds International, 2012. Available from: http://www. woundsinternational.com (accessed 10.05.2022)
2. Davies P, Stephenson J, Manners C (2019) Understanding undisturbed wound healing in clincial pracitce — a global survey of healthcare professionals. Wounds UK 15(4)
3. Deneckere S, Euwema M, Van Herck P et al (2012) Care pathways lead to better teamwork: Results of a systematic review. Social Science Medicine 75(2): 264–8
4. Drennan VM, Ross F (2019) Global nurse shortages : the facts, the impact and action for change. Br Medical Bulletin 130(1): 25–37
5. Drew P, Posnett J, Rusling L; Wound Care Audit Team (2007) The cost of wound care for a local population in England. Int Wound J 4(2): 149–55
6. Dowsett C, Hampton J, Myers D, Styche T (2017) Use of PICOTM to improve clinical and economic outcomes in hard-to-heal wounds. Wounds International 8(2): 52–9
7. Fields D, Brett A, Kavanagh J, Rutter L (2015) Safe staffing for adult nursing care in community settings Evidence review. NICE, London. Available at: https://www.nice.org.uk/media/ default/news/safe-staffing-community-nursing-evidence review.pdf (accessed 23.04.2022)
8. Frykberg RG, Banks J (2015) Challenges in the Treatment of Chronic Wounds. Advances in Wound Care 4(9): 560–82
9. Gray TA, Rhodes S, Atkinson RA et al (2018) Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 8(3): 1–9
10. Guest JF, Ayoub N, McIlwraith T et al (2017a) Health economic burden that different wound types impose on the UK’s National Health Service. Intern Wound J 14(2): 322–30
11. Guest JF, Vowden K, Vowden P (2017b) The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care 26(6): 292–303
12. Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: Update from 2012/2013. BMJ Open 10(12): 1–15
13. Harries RL, Bosanquet DC, Harding KG (2016) Wound bed preparation: TIME for an update. Intern Wound J 13(3): 8–14
14. Hughes J, Costello M, Belshaw M et al (2021) The burden of dehisced wounds in the community: Using early results from a multi-centre service evaluation to propose a standard of care to improve patient outcomes and safeguard woundcare budgets. Br J Health Care Manage 27(1): 16–25
15. Hurd T, Trueman P, Rossington A (2014) Use of a portable, single-use negative pressure wound therapy device in home care patients with low to moderately exuding wounds: a case series. Ostomy/Wound Management 60(3): 30–6
16. Johnson S (2015) Five steps to successful wound healing in the community. JCN 29(5): 30–9
17. Latina R, Salomone K, D’angelo D et al (2020) Towards a new system for the assessment of the quality in care pathways: An overview of systematic reviews. Intern J Environ Res Public Health 17(22): 1–16
18. Leaper DJ, Durani P (2008) Topical antimicrobial therapy of chronic wounds healing by secondary intention using iodine products. Intern Wound J 5(2): 361–8
19. Lindholm C, Searle R (2016) Wound management for the 21st century: combining effectiveness and efficiency. Intern Wound J 13: 5–15
20. McCluskey P, Brennan K, Mullan J et al (2020) Impact of a single-use negative pressure wound therapy system on healing. JCN 34(1): 36–43
21. Olsson M, Järbrink K, Divakar U et al (2019) The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen 27(1): 114–25
22. Raffetto JD, Ligi D, Maniscalco R et al (2021) Why venous leg ulcers have difficulty healing: Overview on pathophysiology, clinical consequences, and treatment. J Clin Med 10(1): 1–33
23. Rippon M, Waring M, Bielfeldt S (2015) An evaluation of properties related to wear time of four dressings during a five-day period. Wounds UK 11(1): 45–54
24. Royal College of Nursing (2014) Moving care to the community: an international perspective. RCN Policy and International Department. Policy briefing 12/13. London: Royal College of Nursing
25. Schwartz JA, Goss SG, Facchin F et al (2015) Single-use negative pressure wound therapy for the treatment of chronic lower leg wounds. J Wound Care 24: S4–S9
26. Seys D, Coeckelberghs E, Sermeus W et al (2021) Overview on the target population and methods used in care pathway projects: A narrative review. Intern J Clin Pract 75(10): 1–7
27. Shamsian N (2021) Wound bed preparation: An overview. British J Community Nursing 26(September): S6–S11
28. Smith and Nephew (2020a) Understanding NPWT/Available at: https://www.smith-nephew.com/uk/products/wound_ management/product-search/picointro/understanding_ npwt/ (accessed 03.05.2022)
29. Smith and Nephew (2020b) What is PICO. Available at: https://www.smith-nephew.com/uk/products/wound_ management/product-search/picointro/whatispico/ (accessed 03.05.2022)
30. Vowden P, Vowden K (2016) The economic impact of hard-to-heal wounds promoting practice change to address passivity in wound management. Wounds International 7(2): 10–5
31. Werdin F, Tennenhaus M, Schaller HE et al (2009) Evidencebased Management Strategies for Treatment of Chronic Wounds. Eplasty 9: e19
32. Wiegand C., Tittelbach J, Hipler U-C, Elsner P (2015) Clinical efficacy of dressings for treatment of heavily exuding chronic wounds. Chronic Wound Care Manage Res 2: 101–11
33. Wounds UK (2019) Best Practice Statement: Addressing complexities in the management of venous leg ulcers. London: Wounds UK. Available at: https://bit.ly/3spUFG6 (accessed 10.05.2022)
This article is excerpted from the Wounds International 2022 by Wound World.