文献精选









This article is excerpted from the 《Frontiers in Microbiology》 by Wound World


This article is excerpted from the 《Journal of Agricultural and Food Chemistry》 by Wound World
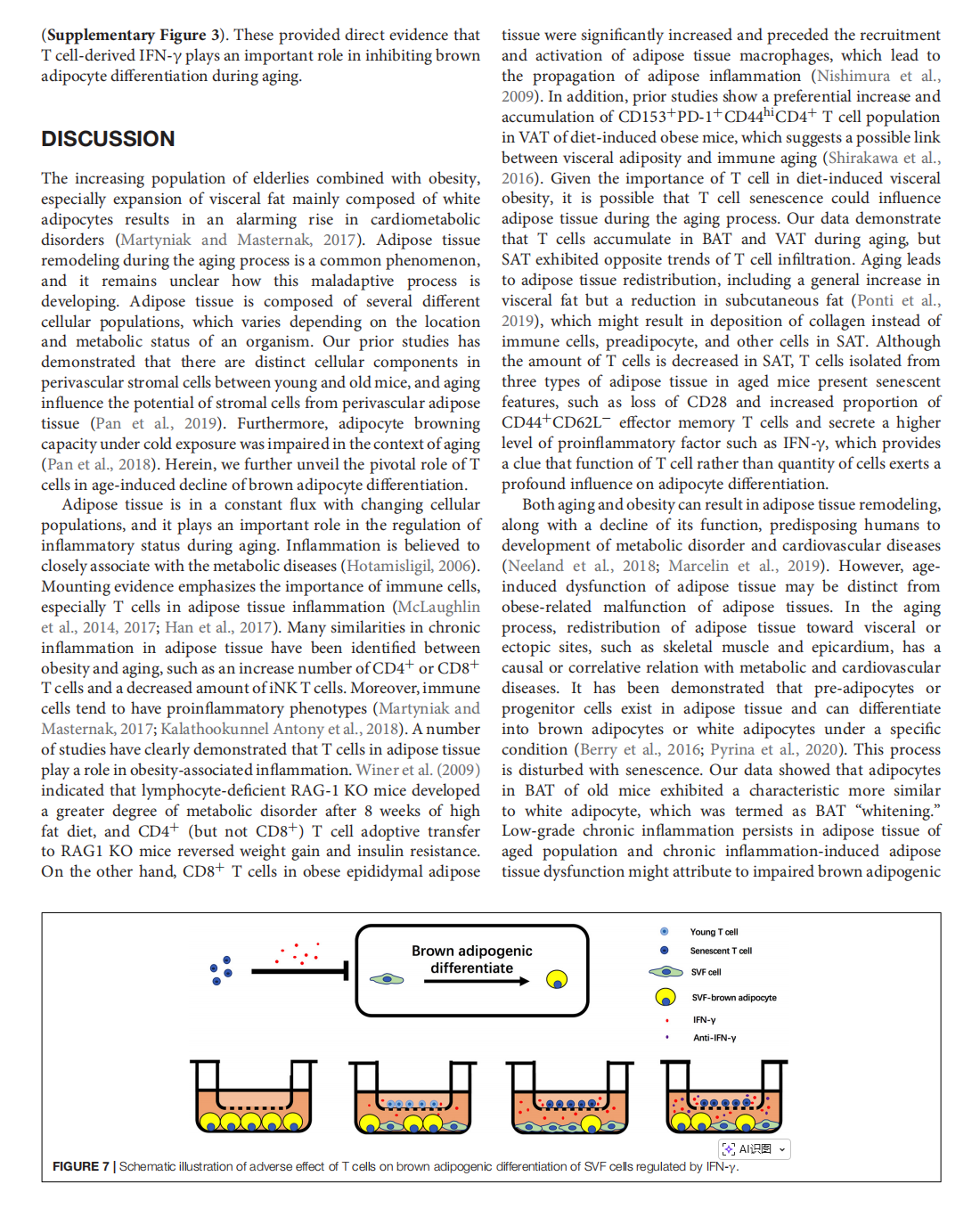

This article is excerpted from the《Frontiers in Cell and Developmental Biology》by Wound World



This article is excerpted from the 《Frontiers in Pharmacology》 by Wound World