文献精选
章 晾
(武汉美莱医疗美容整形医院,湖北 武汉,430000)
【摘 要】 目的 探讨应用手术和非手术联合治疗方案恢复眼周年轻化的临床管理概念。方法 综合分析患者眼周衰老临床表现,选择上睑松弛矫正术、眼袋整形术等手术治疗方案联合肉毒素、玻尿酸、光电治疗等非手术治疗方案进行个性化的治疗。
结果 患者 22 例,术后回访 3-18 个月,眼周年轻化联合治疗方案越全面效果满意度越高。结论 应针对眼周衰老制定个性化联合治疗方案,达到眼周年轻化的目的。
【关键词】眼周年轻化;眼整形术;肉毒素;透明质酸;单极射频
DOI:
The clinical management of the combined treatment of peri-orbital rejuvenation ZHANG Liang (Mylike Cosmetic Hospital, Hubei Province, 430000, China)
[ABSTRACT] Objective To explore the concept of clinical management in the application of combined surgical and non-surgical treatment to restore the peri-orbital rejuvenation. Methods The clinical manifestations of peri-orbital aging were analyzed comprehensively, and surgical treatment (Blepharoplasty and Eyebag surgery ) combined with non-surgical treatment was selected. Non-surgical treatment includes: Botulinum toxin injection , Laser therapy (Radio frequency ; Picosecond) and Microneeding therapy. Results 22 patients were followed up for 3-18 months. The more comprehensive the treatment, the higher the satisfaction. Conclusion It is necessary to make a Personalized combination therapy for peri-orbital aging, so as to achieve the goal of peri-orbital
[KEY WORDS] peri-orbital rejuvenation; Blepharoplasty; botulinum toxin; hyaluronic acid; monopolar radiofrequency
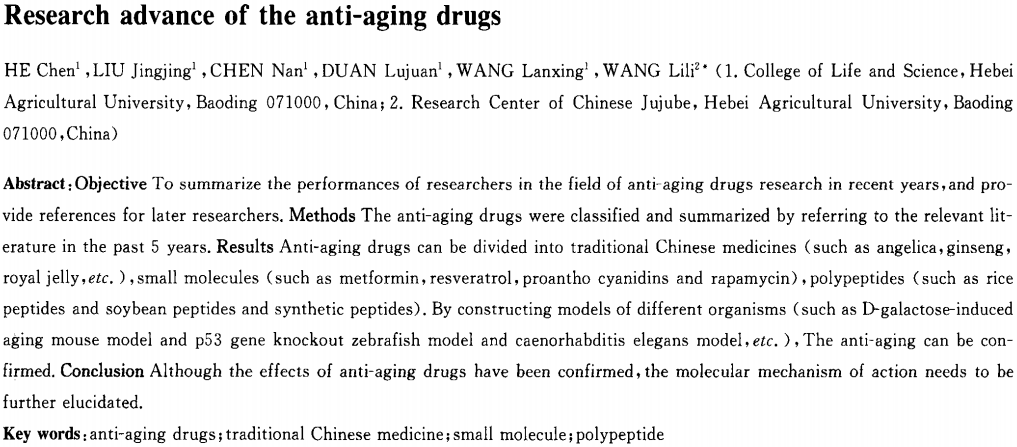
何晨1,刘晶晶1,陈楠1,段路娟1,王斓星1,王丽丽2+(1.河北农业大学生命科学学院,保定071000;2.河北农业大学中国枣研究中心,保定071000)
摘要:目的
总结近年来研究人员在抗衰老药物研究领域的发现,为后期研究提供参考。方法通过查阅近5年的相关文献,对抗衰老药物进行分类归纳。结果抗衰老药物大致可分为中药类(如当归、人参和蜂王浆等)、小分子类(如二甲双胍、白藜芦醇、原花青素和雷帕霉素)和多肽类(如大米多肽、大豆多肽和人工合成多肽),通过构建不同的生物模型(如D半乳糖致衰老小鼠模型、p53基因敲除斑马鱼模型和秀丽隐杆线虫模型等)可证实其抗衰老作用。结论尽管抗衰老药物的作用效果得到了证实,但其分子作用机制有待进一步阐明。
关键词:抗衰老药物;中药类;小分子类;多肽类
DOI:10.3969/i.issn.1004—2407.2020.01.035
中图分类号:R977
文献标志码:A
文章编号:1004—2407(2020)01一0154一04
袁 悦1 ,纪晓晖1 ,顾敬喜2 ,陈官芝1*
1 青岛大学附属医院皮肤科,山东 青岛
2 山东省郯城县皮肤病防治站,山东 临沂
收稿日期:2024年2月27日;录用日期:2024年3月21日;发布日期:2024年3月29日
摘 要
目的:点阵CO2激光疗法在改善皮肤老化方面已经得到了广泛的应用,由于眶周皮肤的脆弱、易造成瘢痕的特性,目前针对眶周皮肤年轻化的激光治疗开展较少。本研究旨在确定点阵CO2激光联合疗法在眶周皮肤再生表面修复中的有效性和安全性。方法:截至2023年12月01号,在3个主要数据库中进行了系统搜索。纳入的研究包括点阵CO2激光或联合其他疗法来改善眼周老化的有效性及并发症,并报告了治疗的有效性和安全性;多篇文章报道同一组患者时,选择最近的报道完整数据的文章。排除标准包括体外研究、动物研究、未使用点阵CO2激光、专家述评、书信、会议摘要、数据不完整或不能获取、CO2点阵激光治疗但未声明关于眶周皱纹或年轻化的研究。结果:筛选后纳入7项临床试验,共纳入166例患者。研究汇总发现眶周皮肤老化及皱纹深度绝大部分都得到了改善,大多数患者都对这项技术感到满意。研究中发现患者在CO2激光术后耐受性良好,主要产生的并发症有包括红斑(n = 8)、色素沉着过度(n = 8)、渗出、渗血、局部水肿、结痂、疼痛、灼热、瘙痒、水疱等。随访时均再未观察到疱疹感染等其他不良反应。术后7天无瘢痕及表皮萎缩再形成。大多数并发症轻微且短暂。治疗后红斑发生率为0.10 (95% CI:0.03~0.18, p < 0.01),色素沉着发生率为0.08 (95% CI: 0.03~0.16, p < 0.01)。结论:研究发现,点阵CO2激光治疗眶周皮肤年轻化是有效且安全的。由于缺乏高质量的报告,有必要进行更多的试验来证实这些结果。
关键词 年轻化,点阵CO2 激光,眶周,Meta分析
A Systematic Review and Meta-Analysis of Efficacy, Safety, and Satisfaction Rates of Fractional CO2 Laser in Periocular Skin Rejuvenation
Yue Yuan1, Xiaohui Ji1, Jingxi Gu2, Guanzhi Chen1*
1 Dermatology Department, The Affiliated Hospital of Qingdao University, Qingdao Shandong
2 Skin Disease Prevention Station of Tancheng County, Shandong Province, Linyi Shandong Received: Feb. 27th, 2024; accepted: Mar. 21st , 2024; published: Mar. 29th, 2024
Abstract
Objective: Fractional CO2 laser therapy has been widely used in improving skin aging. Due to the fragile and scarring properties of periorbital skin, laser therapy for periorbital skin rejuvenation is rarely carried out now. The aim of this study was to determine the efficacy and safety of fractional CO2 laser combined therapy in periorbital skin regeneration surface repair. Methods: As of December 01, 2023, a systematic search was conducted in three major databases. Included studies included the efficacy and complications of fractional CO2 laser or combined with other therapies to improve periocular aging, and reported the efficacy and safety of the treatment. When multiple articles report on the same group of patients, select the most recent article reporting completedata. Exclusion criteria included in vitro studies, animal studies, no use of a fractional CO2 laser, expert reviews, letters, conference abstracts, incomplete or unavailable data, and studies on periorbital wrinkles or rejuvenation that did not claim fractional CO2 laser treatment. Results: After screening, 7 clinical trials were included, involving a total of 166 patients. The study summary found that periorbital skin aging and wrinkle depth were largely improved, and most patients were satisfied with this treatment. The study found that patients were well tolerated after fractional CO2 laser surgery, and the main complications included erythematosis (n = 8), hyper pigmentation (n = 8), exudation, bleeding, local edema, scab, pain, burning, pruritus, blisters, etc. No other adverse reactions such as herpes infection were observed during follow-up. No scar or epidermal atrophy was found 7 days after surgery. Most complications were mild and short-lived. The incidence of erythema after treatment was 0.10 (95% CI: 0.03~0.18, p < 0.01), and the incidence of hyper pigmentation was 0.08 (95% CI: 0.03~0.16, p < 0.01). Conclusion: It is found that fractional CO2 laser is effective and safe in the treatment of periorbital skin rejuvenation. Due to paucity of high-quality reportings, additional trials are warranted to corroborate these results.
Keywords Rejuvenation, Fractional CO2 Laser, Periorbital, Meta-Analysis
Copyright © 2024 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/