Keywords
Issue: Volume 65 - Issue 2 - February 2019 ISSN 2640-5245
Index: Wound Management & Prevention 2019;65(2):20–28.
Login or Register to download PDF
Abstract
Pressure ulcers (PUs) are a common problem with serious health care implications. Purpose: This study was conducted to assess PU prevalence, incidence, clinical features, nursing care measures, and patient variables and outcomes among inpatients admitted to 13 internal medicine departments at a university hospital in Turkey between 2010 and 2014. Methods: Using a cross-sectional, retrospective design, records of all hospitalized patients were reviewed and records from patients with a PU abstracted. Patient demographics, diagnosis, Braden Scale score, and PU information were abstracted from patient files/electronic records. Data were collected to an electronic data collection form between January and December 2015 and analyzed using descriptive statistics, chi-squared, one-way analysis of variance, and Student’s t test. Results: From a population of 20 175 patients, the records of 664 patients showed the presence of a PU; the total PU prevalence rate was 3.3% and the overall PU incidence rate for 5 years was 1.8%. Ulcers were most often Stage 1 (326. 49.1%), located at the sacrum (364, 54.8%), and hospital-acquired (370, 55.7%; 175 (56%) of PU patients were oncology patients, followed by dementia/Alzheimer’s patients (31, 9.2%). A significant relationship between Braden scores and general diagnoses was found (P <.01). Conclusion: PU incidence was highest in patients with cancer and patients >65 years old, and patients with a diagnosis of dementia/Alzheimer’s were at highest risk. Many patients outside of acute care settings have a PU. Risk assessments should be conducted and appropriate nursing interventions should be provided during facility admission and follow-up care. Prospective studies on the prevention of PU development in patients at risk are warranted.
Introduction
Pressure ulcers (PUs), also referred to as pressure injuries, bed sores, pressure sores, and decubitus ulcers, appear as localized injuries on the skin, in the tissue beneath the skin, or both. They usually arise over a protruding bony area due to pressure or pressure in combination with shear and friction.1 As described in PU guidelines,1 the presence of PUs complicates hospital inpatient care.
As indicated in the Wound Ostomy Continence Nursing Society guidelines,2 pressure injuries are particularly problematic for bedbound individuals. Although advances in acute posttraumatic care and rehabilitation are improving life expectancy, an increase in PU incidence among bedridden and wheelchair-bound patients has occurred; in addition, pressure injuries are associated with increased morbidity.2,3 According to a prospective, cross-sectional analysis conducted by Skogestad et al4 among 328 patients in a hospital ward in Oslo, Norway, between 2012 and 2014, PU prevalence was 11.9%. In a cohort study conducted by Ahtiala et al5 in 2010 among 1629 high-dependency care patients in a medical-surgical intensive care unit (ICU), PU prevalence was 11.8%. In a prevalence study by Amlung et al6conducted among 42 817 patients in internal, surgery, high-dependency, orthopedic, and ICUs in United States-based acute care facilities, total PU prevalence was 14.8%. In a prevalence/incidence study conducted by Davis et al7 in 2 long-term health care facilities in Canada, PU prevalence was 36.8% and 53.2%, respectively.
A PU prevalence study8 conducted in Spain (N = 740) found rates to be 8.24% in hospitalized patients, 8.34% in patients in home care programs, and 6.43% among patients in long-term health care facilities. Wann-Hansson et al9 reported a point prevalence rate of 27% in a Swedish university hospital in a study of 66 facilities representing 11 584 patients from medical, surgical, pediatric, neurologic, urologic and obstetric, psychiatric, and geriatric units, and ICUs in Germany reported a PU prevalence of 11.7%10 Uzun and Tan11 reported an 11.6% PU prevalence in a group of 344 patients in Turkey.
Many factors contribute to the formation of PUs. Prospective, descriptive, and retrospective studies1,12,13have shown that regardless of the causative factors, PUs result in extended hospital stays and increased surgical procedures, treatment costs, and nursing care. PUs can exert a life-threatening impact on a patient’s physical health. Furthermore, they can lead to psychological problems such as loss of independence and social isolation. In a descriptive study by Lepistö et al14 involving 164 patients with PUs, 29% experienced a sense of poor psychological well-being. PU prevention has been shown to go a long way in improving the health status of patients. Timely and appropriate prophylactic nursing interventions, especially those employing risk assessment, have been shown in a prospective study11 and descriptive, retrospective studies13,15 to reduce PU prevalence and incidence. Such care includes implementation of prevention strategies such as assessing PU risk, using supportive surfaces, repositioning patients, maintaining proper skin care, using hygienic interventions, and improving nutrition status.
Although many PU-related studies have been conducted in Turkey, the number of studies involving bedridden patients using the risk assessment criteria remain limited.15 The aim of this study was to assess PU prevalence, incidence, risk, clinical features, and outcomes among patients hospitalized in the internal medicine departments in a Turkish hospital between 2010 and 2014.
Methods and Procedures
Study design and sample selection. The study used a retrospective, cross-sectional design. The study sample consisted of patients with a PU hospitalized in a major university hospital in various internal medicine departments (geriatrics, oncology, diabetes, general internal medicine, pneumonia, nephrology, hematology, hepatology, gastroenterology, rheumatology, endocrinology, bone marrow, and special internal medicine wards) between January 1, 2010, and December 31, 2014.
All admitted patients were evaluated for PUs by trained nurses using the Braden Scale during initial hospital admission and subsequent hospitalization. Inclusion criteria specified study participants must be at least 18 years old, hospitalized for at least 24 hours, and have a PU indicator monitoring form included in their records. All patients with current and developing PUs were followed with this form. All patients with PUs were included in the study.
Measurements/Instruments. Data were extracted from patient files and electronic patient records retroactively using the Patient Information Form, scores/assessments from the Braden Scale instrument, and the Pressure Ulcer Indicator Form.
Patient Information Form. This form contains patient sociodemographic characteristics (age and gender) and clinical information (medical diagnoses and hospital department).
The Braden Scale. The Braden Scale was developed by Barbara Braden and Nancy Bergstrom in 1987.16 It has 6 subscales: moisture, mobility, activity, nutrition, sensory perception, and friction/shear. Scores can vary between 6 and 23. The lower the score, the higher the predicted risk. Ayello and Braden17 identified incremental changes in risk based on the percentage of patients who can be expected to develop PUs: a score of 15 to 16 indicates the patient is at risk; 13 to 14, at moderate risk; 10 to 12, at high risk; and 9 or below, at very high risk. In patients age 75 and above, a score of 15–18 represents low risk.17,18 Levels of risk also may be used to determine the aggressiveness of preventive efforts and to assess their success. This study also grouped PU risk assessment according to these criteria. Braden Scale validity and reliability for use in Turkey was determined by Pınar and Oğuz18 in 1998 (Cronbach alpha value of 0.88).
Pressure Ulcer Indicator Form. Used to monitor patient medical diagnosis, this instrument contains the Braden score, the department where the PU occurred, PU stage according to NPUAP classification,1 PU location, and the treatments and results of those treatments. All patients are evaluated for PU risk on admittance to the hospital using the Braden Scale. If the patient is determined to be at risk, the score is entered into the risk section on the Pressure Ulcer Indicator Form. If the patient already had a PU, patient information was entered into the follow-up section. If the ulcer developed after admission, it was recorded again. The Pressure Ulcer Indicator Form includes only the monitoring data of patients developing PU in 2010; as of 2012, the Braden Scale was added to the indicator form,19 noting patients admitted to the hospital who have extant PUs and a Braden score of <17.
The Pressure Ulcer Indicator Form also contains a protocol for necessary nursing interventions (depending on the risk assessment scores and ulcer features) to be used to prevent PUs. Examples of measures in this section include conducting risk assessment and skin evaluation, ensuring proper nutrition, repositioning the patient, and providing support surfaces. Patients with PUs transferred to the acute care unit are monitored with this form until they are either discharged from the hospital or die.
A monthly PU monitoring form was maintained for all patients who already had PUs. The information on this form was recorded as an indicator of nursing care. This form determined nursing care interventions and ulcer characteristics.
According to a review by Dealey20 of current evidence related to skin care and PU prevention, the most important principle in skin care is personal hygiene. The skin should be kept clean and dry and washed with a hypoallergenic soap. A moisturizing lotion should be used on dry, cracked, or flaking skin to prevent skin moisture loss. In addition, hot water should be avoided and sheets should be kept dry and wrinkle-free.
Relevant terminology.
Clinical status change/patient outcome. This refers to provision of health care measures determined on the basis of the clinical status of the patient. For example, once treatment is no longer necessary, a patient is discharged. If his/her condition worsens, he/she is transferred to the ICU.
Healing process. This refers to the process through which the ulcer improves or heals. If the ulcer was no longer visible, it was considered healed. The term stable was used if the ulcer stage remained unchanged. If the ulcer worsened, it was considered to be deteriorating.
Data collection/procedures. Digital data bank records were used to identify eligible patients admitted between January 1, 2010, and December 31, 2014. Information was obtained manually from the hospital archives by one of the authors between January and December 2015 and recorded on the electronic data collection form in the patient records.
Data analysis. Raw data collected from patient records were entered into the statistical analysis packet program and grouped (eg, by Braden scores, disease diagnoses, number of PUs, nursing interventions). Data were analyzed using SPSS for Windows, version 13.0 (SPSS Inc, Chicago, IL). The results are presented as number, percent distributions, and averages. Main pathology, clinical process, and healing process were compared using Pearson’s chi-square. One-way analysis of variance was used to compare Braden score means according to diagnoses; Student’s t test was used to compare age groups. The level of significance was set at P <.05 for all analyses.
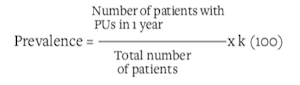
Incidence and prevalence calculations. Prevalence is a frequently used epidemiological measure of how commonly a condition or disease occurs in a population. Incidence measures the rate of occurrence of new cases of a condition or disease.19 Prevalence and incidence calculations included all patients with PUs in the hospital. All hospitalized patients were evaluated using the Braden Scale. Prevalence rates were calculated for the different years.
Prevalence was calculated using the following formula:
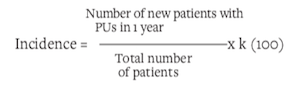
The incidence is calculated using the following formula:
Ethical considerations. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study protocol was approved by the Istanbul University Cerrahpasa Medical Faculty Ethics Committee (Voucher no:/references: 83045809/8255). Informed consent was not obtained because the study was retrospective. All data analyzed were collected as part of routine diagnosis and treatment.
Results
During the time of the study, 20 175 patients were admitted. Of those, 664 were found to have PUs. The mean age of patients with PUs was 64.77 ± 17.62 years; gender was equally divided (332 men and women each) (see Table 1).
PU prevalence and incidence. In 2010, the PU prevalence was 4.9% (see Figure). From 2010 to 2012, PU prevalence decreased to 2.3%, then rose to 2.5% in 2013. In 2014, the prevalence increased to 4.1% for a total 5-year prevalence of 3.3%. A significant difference in PU prevalence among in-patients was noted between 2010 and 2014 (χ2 = 53.93, P <.001) (see Figure).
In 2010, hospital-acquired PU incidence was 3.3%. It declined to 1.1% in 2012, then increased to 1.2% in 2013 and to 1.9% in 2014. Overall, PU incidence decreased from 3.3% in 2010 to 1.9% in 2014. Total PU incidence for 5 years was 1.8%. The difference in PU incidence between 2010 and 2014 was significant (χ2= 58.46, P <.001) (see Figure).
PU characteristics. The majority of patients (326, 49.1%) had a Stage 1 PU, followed by Stage 2, Stage 3, and Stage 4 (286 [43.1%], 42 [6.3%], and 10 [1.5%], respectively); 457 (68.8%) of patients had 1 ulcer, 294 (44.3%) had acquired their PU outside the hospital (ie, the ulcer was present on admission), and 370 ulcers (55.7%) were hospital-acquired. The preponderance of ulcers were located on the sacrum (364, 54.8%), ischium (218, 32.8%), and heels (32, 4.8%) (see Table 1). The most common preventive nursing interventions were skin care (used in 636 cases [95.8%]), turning schedule (537, 83.9%), and dressings (539, 81.2%) (see Table 1). Documented hygiene interventions included skin care (assessment, moisture control, cleaning) and changing bedsheets and patient underwear. Regardless of the preventive nursing care methods used, 420 patients (63.3%) experienced no change in wound condition. Healing was achieved in 122 patients (18.4%) while they were hospitalized (see Table 1).
Braden scores of PU patients. The Braden Scale scores of the PU patients (n = 310) are described in Table 1: 354 patients (53.3%) did not have a completed risk Braden Scale score in their files. Of the 310 patients with Braden evaluations, 285 (91.9%) were found to be at risk (mean score 12.92 ± 2.85, range 6 to 22). The average Braden scores of persons >65 years old (12.5) were lower than scores of younger persons (13.3); older patients were at comparatively greater risk for developing PUs than younger patients (t = 2.34; P <.01) (see Table 2). The illness associated with the highest risk according to the Braden score was dementia/Alzheimer’s (10.93 ± 2.46), followed by pulmonary disease (12.45 ± 4.05), cancer/oncology diagnosis (12.96 ± 2.37), and diabetes (12.92 ± 3.93). A significant difference between Braden Scale scores and primary diagnosis was found (F = 2.87; P <.01) (see Table 2).
Healing, main diagnosis, and clinical status change/patient outcome. Of the 664 patient records assessed, 372 PU patients (56%) were oncology patients, followed by dementia/Alzheimer’s patients (31, 9.2%); 43.3% of the PUs in these patients healed and the patients were discharged. A significant difference was noted between diagnosis and healing process (χ2 = 41.25; P <.001) (see Table 3).
PUs remained unhealed in 130 patients (82.8%) transferred to the ICU. A significant difference was found between the patient’s clinical status change and healing status (χ2 = 85.24; P <.001) (see Table 3).
Discussion
Nurses deal with the complexities of PU care, tending to the patient’s PU and taking precautions to ensure new PUs do not develop. This study provided detailed information concerning PU prevalence and incidence and the characteristics of patients, ulcers, nursing care interventions, and outcomes in a hospital in Turkey.
PU prevalence and incidence. PUs vary in incidence and prevalence across acute care facilities and countries; a review21 of international health care publications reported an incidence of 1% to 11% and a prevalence of 3% to 22% among inpatients. Between 2006 and 2013 among 5354 patients in Spain, Alonso-Lorente et al22 found a 4.5% PU prevalence; in India, Mehta et al23 reported a 7.8% PU prevalence. Incidence and prevalence rates for PUs ranging between 2.7% and 29.5% and 16.6% and 18.5%, respectively, also have been reported in Iceland24 and in Norway.25 Turkish hospital publications report incidence rates of 14.3% to 54.8% and prevalence rates of 7% to 10.4% in hospitalized patients.2,11,26,27 In an evaluation of 404 patients 18 years and older treated in medical, surgical, and critical care units in a university hospital, Inan and Öztunc3 reported an overall PU prevalence of 10.4% and a prevalence of 7.0% in internal medicine. Aygör et al28 found a PU prevalence of 5.8% in a group of 209 patients in medical and intensive care units. In the current study, the 5-year PU prevalence and incidence rates were 3.3% and 1.8%, respectively — lower than other studies.
With a growing awareness of the importance of preventing PUs comes the realization that using assessment tools to identify the risk for PU development is important.25 Identifying patients at risk of developing PUs and engaging in interventions that prevent their formation are increasingly emphasized. A descriptive, analytic, prospective study17 reported the incidence of PUs is higher in institutions not performing risk assessment.
The decline in PU prevalence seen in the first years of the study was followed by an increase in 2013. That year, the use of care indicators including the assessment of PU was initiated; protocols were created according to risk groups. These changes and improvements in care indicator monitoring may have led to an increase in the identification of PU patients in 2013 and the subsequently observed decrease in PU prevalence, which was similar for incidence between 2010 and 2012.
PU characteristics. Almost half of the PUs assessed in this study were Stage 1 and Stage 2 ulcers (49.1% and 43.1%, respectively) that occurred on the sacrum (54.8%). This is similar to hospital data from other countries.25,29,30 In other studies,31,32 70% to 87% of wounds were Stage 1 and Stage 2 ulcers. These relative frequencies are generally the same in both general hospital wards and ICUs. In the multilevel analysis of medical patients by Bredesen et al,25 ulcers were also most commonly Stage 1 (64.7%) and Stage 2 (22.4%). The most commonly occurring ulcer in Inan et al3 was Stage 2 (45.2%). In contrast, ulcers occurring with the most frequency in the study by Uzun and Tan11 were Stage 1 ulcers (72.3%). Stage 1 and Stage 2 PUs highlight the need for greater attention to prevention. Not only should health care providers treat a patient’s PU, but measures to prevent the development of new PUs also should be taken because ulcers in their earlier stages are more common and may be easier to treat/prevent.
Similar to previous research, the sacrum and ischium are the most common locations of PUs in this study. The Uzun and Tan11 study noted 38.3% of PUs were located in the sacrum and 25.5% were in the ischium. In Mehta et al,23 46.4% were in the sacrum and 28.5% in the ischium. In the Bredesen et al25 study, 40.0% of PUs occurred in the sacrum and 21.2% in the heel. Fernandes et al30 reported the areas where PUs most commonly occurred, in order of frequency, were the sacrum, trochanter, and heel.
There are numerous opportunities for improving PU prevention. Use of prevention guidelines and attention to support surfaces, the latter found to be particularly important in the retrospective study by Amir et al,33are promising for the reduction of PU. In the current study, the main nursing care interventions were attention to hygiene, maintaining a turning schedule, and the application of dressings. Appropriate support surfaces ranked fourth in the measures taken. As a result of this study, it was suggested that the use of support surfaces in the hospital where the study was conducted should be increased when caring for patients with PU, and leaflets providing necessary information on PU prevention were distributed in all hospitals.
Braden Scale score. Assessing the risk of PU occurrence is crucial to prevention. The most widely used PU risk assessment scale worldwide is the Braden Scale.34,35 In Bredesen et al,25 19.4% of the ulcers occurred in persons with a Braden score of <17; in Mehta et al,23 31.8% of the patients developing PUs had a Braden score of <16. In the study by Tel et al,15 PUs formed in 41% of patients determined to be at risk.15
In studies conducted in Turkey and abroad, PU prevalence was greatest in persons with Braden Scale high-risk categories, underscoring the effectiveness of the Braden score in evaluating the risk of PU.36,37In the present study, 91.9% of the PU patients were found to be at risk. Knowing which risk group patients fall into is crucial for preventing and treating PU.
Diagnoses and clinical status changes/patient outcomes. Disease diagnosis is important in patients with PUs.29 In the current study, more than half of the patients with a PU had been diagnosed with a malignancy. Literature that considers the specific risk factors related to PU development for the patient with cancer is scarce. However, a retrospective analysis38 and descriptive, cross-sectional study39 have demonstrated the relationship between skin disturbances and cancer. Advanced cancers may result in anorexia, cachexia, malnutrition, anemia, movement disorders, circulation difficulties, and neurological disturbances. A retrospective study40 and a literature review41 on the specific risk factors regarding PU development have reported a link between skin disorders and cancer. In their review of the literature, Esper and Harb42 reported that in half of all cancer patients, eating disorders such as cachexia play a major role in morbidity and mortality; low caloric intake is a common complication of cancer affecting 80% of advanced cancer patients.
A retrospective study involving the elderly by Jaul and Rosenzweig43 uncovered a significant relationship between PU and dementia and a decline in life expectancy. In the current study, 9.2% of PU patients had dementia/Alzheimer’s and 31.1% of ulcers in these patients healed before discharge.
In the current study, 44.3% of the patients were admitted to the hospital with a PU and 56.7% of the patients were discharged from the hospital with a PU. A cross-sectional study44 showed PUs developed at home, and according to a descriptive study45 the severity of PUs increased with the length of time patients were bedridden and that home care patients were at high risk for PU.
In the descriptive study of pressure injury in a community population conducted by Corbett et al46 of 44 202 hospital admissions over a 1-year period, 2309 adults were admitted to the hospital with at least 1 PU and the overall prevalence of present-on-admission pressure injuries upon hospital admission was higher than previously published.
Limitions
This study has limitations. First, a retrospective study has inherent limitations regarding the accuracy of the recorded/extracted data. Second, this was a single-center study and PU incidence and prevalence can vary among different medical centers. In some cases, data such as Braden scores and length of hospital stay were missing from patient records, information that is needed to assess the healing process. Expert nurses performed the initial assessment of patient PUs and recorded their observations on the indicator observation form, but there may have been internal inconsistencies among their reports. For example, incontinence-associated dermatitis cannot easily be distinguished from Stage 1 and Stage 2 PUs, and no differentiation between incontinence-associated dermatitis and PUs appears on the indicator forms, further limiting study findings. In addition, healing outcomes following hospital discharge were not assessed, limiting the validity of this study variable.
Conclusions
A retrospective study of 5 years of patient records showed an overall decline in the incidence and prevalence of PUs, but the data also suggest that reporting practices and policies affect documentation and resultant rates. Braden scores were lowest in patients with dementia, and PUs were noted to be more prevalent in patients with a diagnosis of malignancy. The proportion of patients whose ulcer healed while hospitalized was lower in patients transferred to intensive care and in persons who died than in patients who were discharged. A considerable proportion of patients were admitted (44.3%) or discharged (56.5%) with a PU, suggesting a need for PU prevention and care in the postacute and home care environment.
Affiliations
Dr. Biçer is an Assistant Professor, Department of Medical Nursing, Hatay School of Nursing, Mustafa Kemal University, Hatay, Turkey. Ms. Güçlüel is Head Nurse of Internal Medical Nursing,; Ms. Türker is a Quality Management Nurse; and Ms. Kepiçoğlu is an Internal Medical Nurse, Department of Internal Medicine, Cerrahpaşa Medical Faculty, Istanbul University, Fatih, Istanbul, Turkey. Dr. Şekerci is an Assistant Professor, Department of Community Health Nursing, Hatay School of Nursing, Mustafa Kemal University. Ms. Say is Head Nurse of Internal Medical Nursing, Department of Internal Medicine, Cerrahpaşa Medical Faculty, Istanbul University.
Correspondence
Please address correspondence to: Emine Kır Biçer, PhD, RN; email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。.


