Issue: Volume 56 - Issue 1 - January, 2010
Login or Register to download PDF
Abstract
An ileal conduit is the most common urinary diversion following radical cystectomy for invasive bladder cancer. Unlike internal complications commonly described in urological literature, reports about the incidence of external complications are sparse.
A Medline database review (1996–2008) of English-language literature was conducted to: 1) describe and compare external stoma and peristomal complications and complication rates among outpatients with ileal conduit diversion following radical cystectomy, and 2) summarize commonly used prevention and management strategies. Fourteen publications (mostly retrospective, single-center studies) met inclusion criteria. The reported incidence of complications ranged from 15% to 65%. Divided according to pathogenesis, the most commonly reported complications are 1) stoma or abdominal wall-related changes — parastomal hernia, stoma prolapse, stenosis, and retraction; and 2) peristomal skin changes — chemical injury: irritant contact dermatitis, pseudoverrucous lesions, and alkaline crustations; mechanical injury: pressure ulcers, skin stripping injuries, mucocutaneous separation; infection: candidiasis, folliculitis; immunologic disorders: allergic contact dermatitis; and disease-related lesions: varices, pyoderma gangrenosum, malignancy. Peristomal complications also appear to be under-recognized and under-reported. Research to establish the validity and reliability of assessment tools and long-term follow-up studies are needed to improve the evidence-base of prevention and care.
Potential Conflicts of Interest: Dr. Kassouf, Dr. Szymanski, and Ms. St-Cyr have nothing to disclose. Mr. Alam is an employee of Hollister Ltd., Aurora, Ontario, Canada.
Please address correspondence to: Wassim Kassouf, MD, CM, FRCSC, Montreal General Hospital, 1650 Cedar Avenue, L8-315, Montreal, Quebec H3G 1A4 Canada; email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。.
External stoma complications are the most frequent indication for reoperation after cystectomy.1 They represent the most common reason for outpatient ostomy service visits and are important predictors of patient quality of life.2 In addition, although the majority of peristomal skin disorders are mild and can be easily managed on an outpatient basis, they can progress in severity when unattended.3 Evidence-based approaches are sparse for primary and secondary prevention of complications.
There appears to be a certain disconnect between the prevalence of cystectomy with ileal conduit creation and the knowledge regarding long-term stoma complications in the literature and among patients and urologists. In a cross-sectional study (N = 202),3 62% of participants with a peristomal skin disorder did not believe they had a disorder and more than 80% of participants did not seek professional attention.
Following radical cystectomy and ileal conduit creation at the authors’ institution, patients are followed-up by an interdisciplinary team, which includes experienced enterostomal therapy nurses (ETNs) and urologists. The high frequency of external stoma and peristomal complications observed in these patients, along with questions about evidence-based management principles, were motivating factors for conducting and synthesizing a literature review to describe and compare epidemiology, management, and assessment of long-term external stoma and peristomal complications among patients with ileal conduit diversion following radical cystectomy.
Methods
A literature review of the Medline database (1966 to 2008) was conducted to find English-language epidemiological data on outpatient external stoma complications. Studies and reviews selected pertained to external complications among patients following ileal conduits after radical cystectomy. Articles that did not include this patient population and/or report external peristomal (involving the stoma or peristomal area) complication rates were excluded. Search terms included stoma, ileal conduit, urostomy, radical cystectomy, parastomal, peristomal, stoma complications, hernia, stenosis, retraction, dermatitis, and ulcer. Rate ranges were combined from different studies for reporting purposes. Studies about peristomal skin assessment tools also were identified. To illustrate review results, photographs were obtained with patient consent by an ETN.
Results
Fourteen publications were found from which complication rates could be extracted1,3-15 (see Table 1). Of these, five (36%) were published in nursing journals,3,5,7,8,13 three were reviews,7,9,13 and two were long-term retrospective studies of patients who had exclusively undergone radical cystectomy or exploration for bladder cancer with ileal conduit creation.1,6 Two other publications (a review2 and a retrospective single-center series of 319 patients with urinary diversions followed for 3 years16) were used for descriptive and risk factor data.2,15,16
The reported overall rate of external stoma complications was found to range from 15% to 65%.1,3-6,8-12,14Complications were reported in the literature and categorized following an accepted pathogenesis-based classification2: 1) stoma, or abdominal wall-related changes — parastomal or peristomal hernia, stoma prolapse, stenosis, and retraction, and 2) peristomal skin changes — chemical injury (irritant contact dermatitis, pseudoverrucous lesions, alkaline encrustations), mechanical injury (pressure ulcers, skin stripping injuries, mucocutaneous separation), infection (candidiasis, folliculitis), immunologic disorders (allergic contact dermatitis), and disease-related lesions (varices, pyoderma gangrenosum, malignancy). Three articles describing peristomal skin assessment tools were identified.4,17,18
Understanding “Normal” Peristomal Skin
Skin care begins with an understanding of “normal” (intact and healthy) peristomal skin.2 Even when covered with an adhesive skin barrier, this skin is similar to the other side of the abdomen. Chronic irritation is abnormal. Covering peristomal skin is the primary method used to protect it from stoma effluent. Results of one cross-sectional study3 suggest that contact with irritating effluent causes 75% of peristomal skin disorders. Appropriate stoma siting is also important — considerations include abdominal scars,14 contour, and clothing (ie, the stoma should not automatically be placed in the middle of an abdominal quadrant or below a low belt line).7 There must be ample flat area around the stoma (2 to 3 inches) for the pouching system to adhere adequately because a poorly located stoma also can lead to pouching system leakage.7 The stoma should be located at the crest of an abdominal bulge where it can be easily seen by the patient.7 The pouching system needs to be reassessed and refitted as stoma edema resolves postoperatively and patients gain weight.
Overall Complication Risk
Despite the wide use of ileal conduits in urinary diversion and a high cumulative incidence of external complications involving the stoma (15% to 65%),1,3-6,8-12,14 literature addressing this issue remains scant.1 This range of ileal conduit complications is comparable to the 10% to 70% risk for enterostomies.3,5,19 In one study (see Table 1),3 peristomal skin disorders were noted in 48% of patients with ileal conduits, 57% with ileostomies, and 35% with colostomies. However, the true incidence of complications is difficult to assess. Estimates vary widely across studies and most do not include definitions or details of the complications assessed.2 In two analyses of retrospective, single-center data of more than 1,600 patients with enterostomies, preoperative siting of an enterostomy and education by an ETN have been found to decrease overall postoperative enterostomal complications by 25% to 43%.20,21
Need for Long-term Follow-up
Studies suggest that external peristomal complications can occur at any time after surgery. In one long-term study6 of patients living with ileal conduits with a median follow-up of 98 months, the median time to stoma complications was 54 months, with almost 20% occurring 10 years after surgery (see Table 1).The one exception appears to be mucocutaneous separation, which usually occurs within 1 month following surgery.2 For these reasons, follow-up with an ETN is recommended at 2 to 4 weeks after surgery, 3 months, 6 months, and then annually for the life of the patient.2
Stoma or Abdominal Wall-related Complications
Abdominal wall-related complications (parastomal hernia, stoma prolapse, stenosis, and retraction) not only have a significant morbidity, but they also increase the risk of a concurrent peristomal skin disorder by altering the abdominal contour and pouching system fit, leading to urine leaks and pooling.2,5 They remain the most common cause for reoperation after ileal conduit surgery.9
Parastomal hernia. A parastomal, or peristomal, hernia is an incisional hernia secondary to a fascial defect surrounding the conduit.9,22 A recent review1 on parastomal hernias proposed two comprehensive definitions. Clinically, a parastomal hernia is any palpable defect or bulge adjacent to the stoma detected with the patient supine with legs elevated or with a standing patient coughing or straining22 (see Figure 1a). Radiologically, it is any intra-abdominal content protruding along the ileal conduit on a CT scan. With regard to ileal conduits, the 2-month, postoperative incidence is 12%5 and prevalence is 5% to 28%1,6,9-12 — by comparison, prevalence among enterostomies is 5% to 65%.22 Parastomal hernias can appear years after surgery; average time to herniation is 8 to 22.4 months.1,10,11,13 In a single-surgeon case series1 of 137 patients who had undergone ileal conduit diversion after radical cystectomy for bladder cancer, overweight (body mass index [BMI] 25 to 30 kg/m2) and obese (BMI >30 kg/m2) patients were found to be four to six times more likely than those with a normal BMI to develop parastomal hernias over 5 years. Other cited9 contributing factors include malnutrition, chronic cough, and use of steroids, although studies are often small, patient populations include all stomas, and risk ratios are unknown. In the enterostomal literature, emergency surgery has not been shown to be a risk factor for a parastomal hernia.23
Placing the stoma in, rather than lateral to, the rectus abdominis sheath is the gold standard; in a retrospective, single-center case series24 of 130 patients with colostomies, this approach has been shown to decrease parastomal hernia risk from 22% to 3%. Before stoma creation, all facial layers should be aligned so the entire opening is within the sheath.9 A randomized study22,25of 47 persons with colostomies showed that placing a large-pore mesh during the primary operation reduced the parastomal herniation rate (50% versus 5% at 12 months). In this study, no wound or mesh infection, fistula formation, or pain associated with the stoma was recorded among the mostly overweight patients (mean BMI 27.5) followed for a mean of 24 months. However, no data are available on the role of mesh during primary operations in patients receiving an ileal conduit.
Although most parastomal hernias can be managed nonoperatively, a retrospective, single-surgeon case series1 of 137 patients with ileal conduits and a retrospective, single-center case series24 of 130 patients with colostomies have shown approximately 30% require surgical intervention secondary to obstruction, pain, bleeding, poorly fitting pouching systems, or leakage. Surgical outcomes have been shown to be poor, with recurrence rates often >50%1,27 and complication rates up to 88% for surgical bowel obstruction, stoma prolapse, wound infection, fistula, and mesh erosion.26 In the general surgery literature,22 contralateral stoma resiting and primary fascial repair are reported to have recurrence rates of 24% to 86% and 50% to 76%, respectively; ipsilateral or second resitings have even higher risks of recurrence (71% to 86%). Given the poor surgical outcomes and the (albeit) small likelihood of life-threatening complications, many authors16-27 propose avoiding repair and advocate primary prevention, which includes proper siting and surgical technique, weight loss, and management of other risk factors.
Both open and laparoscopic repair of ileostomy and colostomy parastomal hernias with tension-free mesh are promising surgical approaches. In a review article22 and a retrospective, single-center case series26 of 24 laparoscopically repaired parastomal hernias, recurrence rates have been reported at 5% to 11%, but long-term follow-up is lacking. Laparoscopy recently has been implemented to treat patients with ileal conduits.1,26 The laparoscopic intraperitoneal onlay mesh technique carries risks of converting to open surgery (15%), bowel injury (22%), and mesh infection with subsequent mesh removal (9%).22,26 In one case series24 of laparoscopic intraperitoneal onlay mesh repairs that included nine patients with ileal conduits, one required laparoscopic reoperation for an obstructed conduit.
Stoma prolapse. Although the clinical distinction between a parastomal hernia and stoma prolapse has been reported to not always be clear,22 in the authors’ experience the distinction is usually unmistakable. A parastomal hernia presents as a bulge of the peristomal skin, at times associated with stoma retraction. Stoma prolapse involves eversion of the stoma through the abdominal wall28 and telescoping ileal mucosa7 (see Figure 1b). In one study,14 stoma prolapse was defined as stomal protrusion >30 mm.
Stoma prolapse occurs most often in loop colostomies (2% to 46%); it is relatively rare in other types of stomas, affecting 1.5% to 8% of ileal conduits7,11,14,19 at a median time of 2 years after surgery.11 Nonsurgical management includes the use of a prolapse belt to reduce the prolapse, but carries the risk of stoma necrosis.7 A case of stoma prolapse with a parastomal hernia was successfully repaired with tension-free mesh.1
Stoma stenosis. Stoma stenosis is a narrowing of the ostomy lumen, either at the level of skin or fascia, leading to impaired drainage29 (see Figure 1c). It is thought to occur secondary to ischemia, leading to retraction and scarring,7 particularly in the setting of circumferential mucocutaneous separation. Chronic local inflammation and hyperkeratosis, possibly due to an ill-fitting pouching system, are possible causes.9
Historically, the incidence of stoma stenosis was cited as 20% to 25%9; more contemporary research6,7,9-11 notes an incidence of 2.5% to 8.5% at a median of 10 years after surgery.11 This is similar to rates observed among patients with ileostomies and colostomies.7
Stenosis at the skin level can be managed by dilating the stoma opening, usually by inserting a lubricated digit down to the fascial layer for several minutes.7,11 This technique, taught to select patients at the authors’ institution, may need to be frequently and regularly repeated12 and carries a small risk of forming a false passage or opening. Stenotic bowel can be excised; fascial stenosis usually requires surgical revision or resiting.9
Stoma retraction. Stoma retraction has been defined in one enterostomal study19 as a stoma surface >0.5 cm below the skin level (see Figure 1d). Information in ileal conduit literature with regard to this complication is sparse. Stoma retraction can result from persistent tension on the stoma due to short mesentery, inadequate bowel mobilization, or the presence of a thick abdominal wall.7 In relevant literature, it has been associated with obesity19 and Crohn’s disease.30
Stoma retraction occurs in 9% to 15% of ileal conduits10,12 and 1% to 11% of all stomas.7,8 Management is usually conservative and involves use of a convex pouching system and patient education.19
Chemical Injury
Irritant contact dermatitis. Dermatitis presents as erythematous, moist, painful, shallow peristomal erosions in areas of substance contact with the skin2 (see Figure 2a). Irritants include mucus, urine, and skin care products. Dermatitis can be related to poorly sited stomas, urine pooling in skin creases, or stoma pouching system openings that are too large.7 Errors in stoma care technique also can contribute and include inconsistent pouching system changes, reinforcing rather than changing a leaking pouching system, and inappropriate use of protective skin products. Prevention includes optimal stoma placement and creation, patient education, selecting a pouching system of optimal size and convexity, and facilitating patient and caregiver use (eg, a one- or two-piece pouching system).
A 12% 2-month postoperative incidence rate5 and prevalence of 14% to 20%7,11,12 have been reported. These rates are lower than among patients with a colostomy (29% to 31%) or an ileostomy (5% to 70%).7 Irritant contact dermatitis can be managed by resizing the stoma pouching system and possibly refitting with a convex adhesive surface. Peristomal skin creases can be filled with a skin barrier paste or strip. Eroded peristomal skin can be prepared by dusting a hydrocolloid powder to absorb exudate and provide a dry adhesion surface.7
Pseudoverrucous lesions. This complication consists of benign, thickened epidermis with white, grey, brown, or dark red papules or nodules in areas chronically exposed to effluent and causes hemorrhage or pain2 (see Figure 2b). The lesions are also known as chronic papillomatous dermatitis, hyperkeratosis, and pseudoepitheliomatous hyperplasia. Pathogenesis involves epidermal hyperplasia secondary to chronic chemical irritation and often occurs among patients lost to follow-up who wear a pouching system without an anti-reflux valve and too large an opening.2
In one study,14 pseudoverrucous lesions affected 21% of 66 ileal conduits, were seen exclusively after 5 years of follow-up, and were associated with stomas protruding <10 mm. Another study4 noted a cumulative incidence of 23% of 57 patients at 7 years of follow-up.
Management of pseudoverrucous lesions includes refitting the pouching system to cover the lesions and shortening the pouch change intervals to 3 to 4 days until lesions resolve.2 Hydrocolloid powder is used to absorb moisture in the fissures of the lesion; its irregular surface can be covered with strips of extended-wear skin barrier. Although usually not necessary, silver nitrate may be helpful for lesions that are considerably raised and hemorrhaging.2
Alkaline encrustation. Crystal deposition on exposed peristomal skin is a complication unique to urostomies2 (see Figure 2c). Stoma bleeding can occur when crystals are manipulated. Encrustations are associated with pseudoverrucous lesions, alkaline, concentrated urine; renal calculi, and urinary tract infections. In a retrospective, single-center case series11 of 123 patients with ileal conduits followed for a median of 3 years, 23.6% developed encrustation.
Management includes increasing oral fluid intake and acidifying urine with a maintenance dose of 1g daily of ascorbic acid.2Vitamin C should be used with care in patients with glucose-6-phosphate dehydrogenase deficiency, recurrent oxalate renal calculi, and hemochromatosis.31 Patients at the authors’ institution are counselled to dissolve the encrustations with 33% to 50% vinegar-soaked pads applied to the stoma for 20 minutes when changing the pouching system every 3 to 4 days. The stoma can temporarily blanch when applying the pads.
Mechanical Injury
Pressure ulcer. When the pouching system component or accessory delivers too much pressure, early stage pressure ulcers (Stage I) that present as nonblanching erythema that does not resolve in 1 to 2 minutes after removal of the device can occur.2 With enough pressure, tissue ischemia and necrosis lead to further skin breakdown, including partial-thickness (Stage II), full-thickness ulceration (Stage II) (see Figure 3a), or exposure of underlying muscle (Stage IV).32 No incidence data about this complication is available.
Management includes resizing and refitting the pouching system that may be too convex or too firm, as well as loosening or discontinuing the ostomy belt, hernia support binder, or prolapse belt causing the ulcer.2
Stripping injury. Stripping injury can cause erythema with scattered areas lacking epidermis and often corresponds to the adhesive surface or its borders2 (see Figure 3b). It is usually associated with too-frequent adhesive removal or poor technique. In a prospective, single-center series5 of 220 patients with stomas, 7% of patients were affected 2 months after surgery.
Management includes skin support during gentle removal of the pouching system in the direction of hair growth. A liquid skin sealant sometimes is used and wear-time extended to the recommended period.2
Mucocutaneous separation. This complication is an interruption of the suture line with skin separation at the mucocutaneous junction19 (see Figure 3c). It occurs in 12% of patients with enterostomies; no data are available for ileal conduits. Etiology includes compromised healing, infection, a large skin opening, poor surgical technique, and excessive tension at the mucocutaneous junction.2,7
Management involves irrigating and filling the defect with an absorptive powder or dressing (ie, alginate or hydrofiber) while the pouching system covers the packing material and the entire peristomal field.2,7 If infection or an abscess is suspected, the defect is incorporated in the opening size of the pouching system, exposing the wound and allowing it to drain until it resolves. In this situation, the defect heals by secondary intention.33
Infection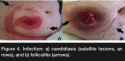
Candidiasis. Fungal infection initially presents as pustules, often progressing to pruritus; burning; and confluent, erythematous plaques with satellite lesions2 (see Figure 4a). It is associated with increased perspiration from activity or fevers, frequent leakage episodes of the pouching system, or recent antibiotic treatments. It has been observed in 2% of patients 2 months after surgery.5
Treatment involves applying antifungal powder with each pouch change until the candidiasis resolves, as well as drying off the pouching system after exercise or swimming.2 The application of a skin sealant may be useful during humid weather.
Folliculitis. This bacterial infection most often involves Staphyloccocus aureus presenting as erythematous or pustular lesions originating at the hair follicles2 (see Figure 4b). No prevalence or incidence data are available.
Because this infection often is associated with shaving, management includes trimming hair with scissors or clippers to leave hair short and above skin level, washing with antimicrobial soap, and applying a skin sealant. Minimizing skin trauma by supporting the skin during gentle removal of the pouching system in the direction of hair growth is an additional preventive measure.
Immunologic Disorder
Allergic contact dermatitis. This allergic reaction to skin care products applied with or composing the stoma pouching system adhesive manifests as erythema, pruritus, vesicles, papules, bullae, skin induration, and erosions2 (see Figure 5). This type of complication should be suspected when the lesion corresponds exactly to an area covered by a specific product or component of the pouching system (eg, tape border or skin barrier). Dyes, perfumes, adhesives, soaps, lotions, and preservatives can be allergens. A retrospective, single-center study11 of 123 patients reported a cumulative incidence of 1.6% over 3 years. The sensitizing product needs to be identified and removed from the ostomy care protocol. A patch test can be helpful to determine allergens; corticosteroid cream applied between appliance changes and antihistamines can relieve symptoms.2
Disease-related Lesions
Varices. Varices occur secondary to portal hypertension and present as purple skin discoloration with dilated, tortuous veins on the stoma2 (see Figure 6a). No incidence data are available. Although the skin usually remains intact, the veins are vulnerable to bleeding, requiring protection of the mucosa. Convex, rigid devices and belts should be used only when necessary and the pouching system should always be removed gently. Minor bleeding can be managed with local pressure and application of silver nitrate, ice packs, and a hemostatic dressing. Uncontrolled hemorrhage requires medical attention.2
Pyoderma gangrenosum. This rare, painful, inflammatory ulceration of the skin often begins with pustules that break open and form full-thickness ulcers with red to purple edges2,7 (see Figure 6b). Although its etiology is unknown, about 50% of cases are associated with underlying systemic disease (eg, inflammatory bowel disease, polyarthritis, and hematologic disorders).2 Because this condition is diagnosed by exclusion, a dermatology referral may be helpful to rule out other diseases, especially skin malignancy. No incidence data are available.
Management of the underlying systemic condition should be the initial focus of the intervention, especially in moderate and severe cases; topical or intralesional steroids may be effective for mild disease.34 Although case reports show effective treatment of pyoderma gangrenosum lesions with topical immunosuppressors (eg, 0.1% tacrolimus35), topical treatment should be considered an adjuvant to systemic therapy36 and should include the application of an absorptive dressing to control excessive exudate (eg, alginate or hydrofiber) and topical or systemic agents to control pain.2
Malignancy. Although sporadically reported for ileostomies and colostomies, malignancy has not been reported in ileal conduits. In the enterostomal literature,2 malignancy can present with peristomal skin or stoma growth, pouch leakage, or a friable, brownish or grey mass. A history of gastrointestinal tumors should increase clinical suspicion. Confirmatory biopsy is required.
Standardized Peristomal Skin Assessment Tools
Despite several decades of descriptive literature on peristomal skin complications among patients with ileostomies, colostomies, and urostomies, no standardized, clinically validated instrument to grade and classify these problems has gained international acceptance. The authors’ research identified three published classification tools.4,17,18
A Classification of Peristomal Skin,4 developed by an ETN and a dermatologist, was published in Sweden in 1988. It focused strictly on dermatologic changes beneath the ostomy appliance, dividing them into irritative lesions, erythematous/erosive lesions, and pseudoverrucous lesions. Severity was based on the area involved (severe erythematous lesions: >2 cm2, erosive: >1 cm2) and height of pseudoverrucous lesions (>3 mm to 5 mm).
In 2007, Bosio et al17 (an Italian team of seven ETNs and four surgeons) proposed a system based on lesion severity and location. It included five lesion descriptions (hyperemic, erosive, ulcerative, necrotic, and proliferative) and five possible locations (four quadrants and total).
The Ostomy Skin Tool,18 recently was developed by an international group of 12 expert ETNs working in collaboration with Coloplast (Minneapolis, MN) and a dermatologist. The tool is based on clinical observations of lesion area and severity in three domains: discoloration, erosion, and tissue overgrowth. Each of the six observations can be scored as 0, 1, or 2. The scores are added to calculate a composite score and implement a diagnosis algorithm. This tool can help guide investigations; allow reliable, quantitative monitoring of treatment effectiveness; and improve interdisciplinary communication. The tool is currently being validated in a large, multicenter international study.
Discussion
A review of the literature revealed 14 published reports1,3-15 of complication rates among patients living with ileal conduits. External peristomal complications after radical cystectomy are common; overall complication rate estimates vary widely between 15% and 65%.1,3-6,8-12,14 Studies typically include small populations and lack consistent definitions, making comparison between case series difficult. Causes of peristomal skin complications are multifactorial and include poor surgical technique, poorly fitting appliance, inappropriate use of the appliance and products, infection, poor healing, and patient risk factors such as obesity.
Studying ileal conduit complications is difficult because conduits are usually a subset of all the stomas investigated and not all complications are stratified by stoma type. This is particularly important, given varying complication rates and complications unique to ileal conduits, such as alkaline encrustations. Study populations identified were heterogeneous in terms of time since surgery. Some case series spanned well over 20 years6,10; five studies included patients operated in the last decade1,3,5,8,10; and only two case series focused strictly on patients operated in the last 10 years.1,5 In light of changing surgical techniques and stoma care standards, complication rates among patients operated decades ago may not apply to patients operated on today.
The primary goal of the current endeavor was to study complication rates among patients with ileal conduits after radical cystectomy. All but two studies1,6 reported rates for all ileal conduits, regardless of indication. Because rates of ileal conduit complications have been reported to be higher among women with urinary incontinence,10,14 results of such studies might be biased.
Three published assessment tools for stoma complications also were identified.4,17,18 The most recently developed, the Ostomy Skin Tool, is currently being validated in a multicenter trial.18 The Coloplast Dialogue Study is ongoing and expected to end in June 2010 (see www.coloplast.com/ostomycare/topics/educationtools/the ostomyskintool/about/pages/validityofthetool.aspx). An objective, validated, comprehensive, and widely accepted classification system should facilitate documentation and comparisons, allow effective communications among physicians and ETNs responsible for the care of ostomy patients,4 and guide therapy. Current stoma care guidelines rely heavily on expert opinion rather than scientific evidence.5,7 Standardized reporting of complications is a crucial step toward assessing the true incidence of peristomal complications using prospective, multicenter studies as well as toward studying the effectiveness of therapies by taking into account predisposing factors, clear interventions, and objective outcomes.
Conclusion
A review of the literature found that external peristomal complications affect more than 50% of patients with ileal conduits after radical cystectomy and often go unrecognized. The few studies available have low enrollment and use inconsistent definitions. Evidence-based management approaches and long-term follow-up studies are needed.


