Diabetic foot ulceration is one of the most devastating complications that can occur in adults with diabetes. The worldwide annual incidence of diabetic foot ulcers (DFUs) is between 9.1 to 26.1 million, and it affects 15% of all diabetic patients (Oliver et al, 2023; Akkus and Sert, 2022). Patients with DFUs are 2.5 times more likely to develop a 5-year risk of mortality compared to those without (Akkus and Sert, 2022). Factors contributing to diabetic foot ulceration include poor glycaemic control, peripheral neuropathy, peripheral vascular disease, poor foot care and repetitive trauma to the stress area of the foot (Oliver et al, 2023). DFUs affect the patient’s quality of life, with a decline in the functional status and increased risk of sepsis, potentially leading to limb amputation and death (McDermott et al, 2023). The use of a combination of silver gelling fibres with a foam dressing tremendously accelerates the healing of DFU wounds.
Objective
To assess the effectiveness of silver gelling fibres with foam dressing in DFU treatment.
Materials and methods
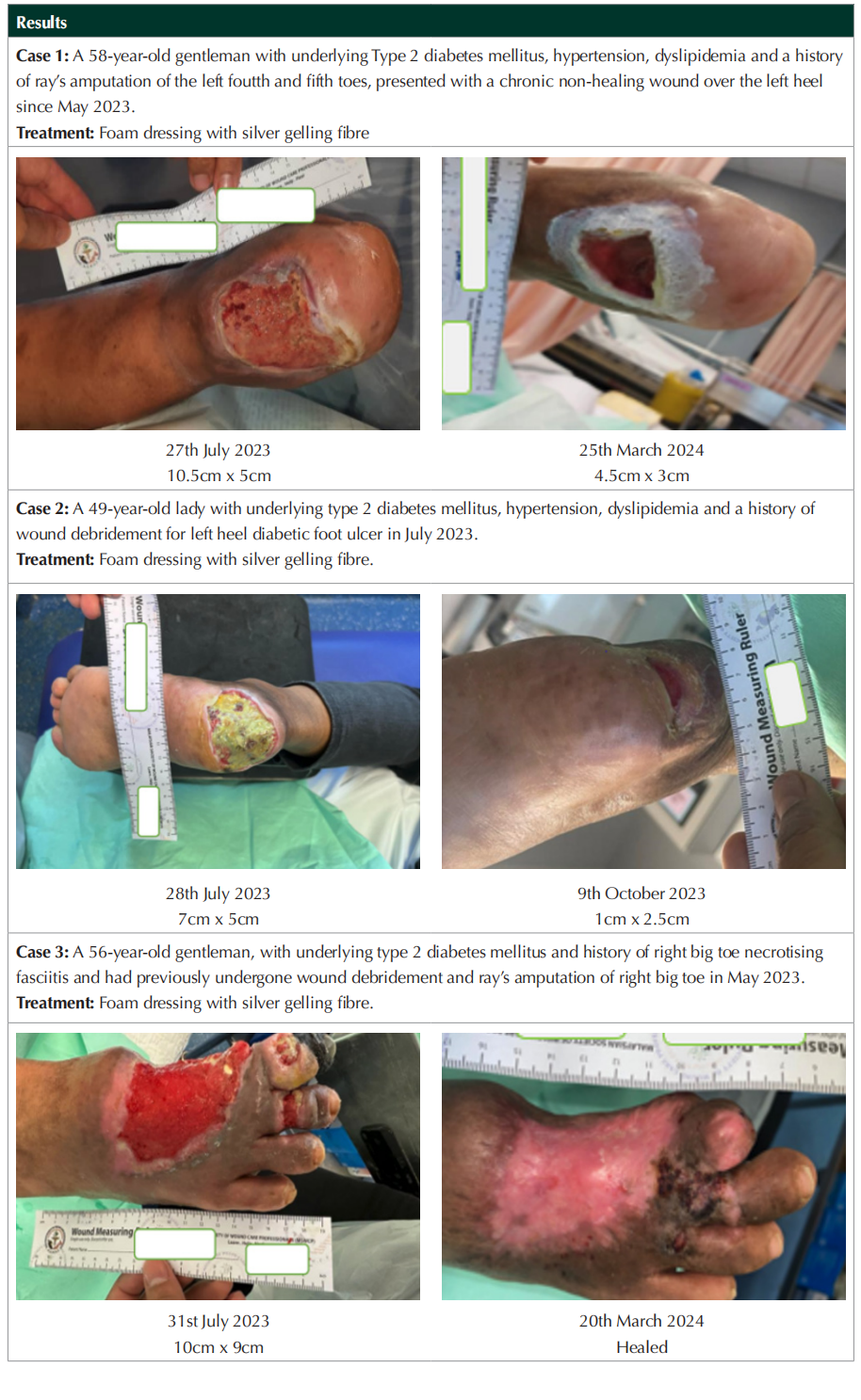
A total number of three patients attending the wound care clinic at Hospital Kuala Lumpur were selected for the study. All wounds were foot ulcers presenting on diabetic patients. No limits were put on age/gender, premorbid illness, condition duration or intensity. The patient’s wounds were cleaned, the silver gelling fibre was applied, and the wounds were subsequently covered by the foam dressing. Patients were followed up and wound dressings were changed at least twice a week. Patient permission was obtained to use their details and clinical images prior to the study.
Dicussion
From the study, we can see that two out of three patients achieved 50% wound healing, while one patient achieved 100% wound healing. Wound healing is the body’s normal physiological response to tissue injury that involves cellular and humoral responses (Hegazi et al, 2024). Normal wound healing in diabetic patients is affected by factors such as impaired oxygenation, venous insufficiency, infections, immune dysfunction, dry environment and age-related changes (Hegazi et al, 2024). Particularly within developing countries, a greater emphasis has been placed on the selection of suitable dressings to manage these complications associated with the diabetic foot.
The use of an ideal dressing will inhibit the propagation of microbes and eventually accelerate wound healing processes (Huang et al, 2021). Silver dressings are bactericidal and fungicidal and, most importantly, have action against the common pathogens found within chronic wounds such as aureus and Pseudomonas spp (Leaper, 2006). Silver ions within the dressing act by merging with the negative charges on the surface of bacterial proteins. This interferes with microbial proliferation, leading to fatal structural changes of the bacterial cell walls and membranes through the alteration of the RNA and DNA (Huang et al, 2021; Lo et al, 2008).
An equally important consideration in DFU dressing selection is the management of wound exudate. Heavily exuding wounds are at greater risk of periwound maceration and excoriation to surrounding skin, resulting in delayed wound healing (McIntosh et al, 2019). These wounds also cause discomfort, produce malodour and negatively affect the patient’s quality of life due to leakage (McIntosh et al, 2019). Foam dressings are used in medium to heavily exudating wounds and will absorb exudate while adhering to the surrounding skin to keep the dressing in place (Nielsen and Fogh, 2015).
Limitations
The main limitations of the study were the variability of the healing factors in the diabetic foot patients. These include the age factor, severity of patient’s peripheral vascular disease, the diabetic control of the HbA1c level, presence of infection, compliance to dressing, site and the depth of wound, all of which play a pivotal role in wound healing.
Conclusion
This case series demonstrated the clinical efficacy of silver gelling fibre with foam dressing in enhancing DFU healing.
Declaration of interest
The author has no conflict of interest to declare.
References
1. Oliver TI, Mutluoglu M (2023) Diabetic Foot Ulcer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537328/
2. Akkus G, Sert M (2022) Diabetic foot ulcers: A devastating complication of diabetes mellitus continues non-stop in spite of new medical treatment modalities. World J Diabetes 13(12): 1106–21
3. McDermott K, Fang M, Boulton AJM et al (2023) Etiology, Epidemiology, and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care 46(1): 209–21
4. Hegazi S, Aly R, Mesilhy R, Aljohary H (2024) Diabetic Foot Ulcer Wound Healing and Tissue Regeneration: Signaling Pathways and Mechanisms. In: Chowdhury MEH, Zughaier SM, Hasan A, Alfkey R. eds, Diabetic Foot Ulcers - Pathogenesis, Innovative Treatments and AI Applications. IntechOpen. Available from: http://dx.doi.org/10.5772/ intechopen.1004267
5. Huang C, Wang R, Yan Z (2021) Silver dressing in the treatment of diabetic foot: A protocol for systematic review and metanaiysis. Medicine 100(7): p e24876
6. Leaper DJ (2006) Silver dressings: their role in wound management. Int Wound J 3(4): 282-94. doi:10.1111/j.1742- 481x.2006.00265.x. PMID: 17199764; PMCID: PMC7951582
7. Lo S-F, Hayter M, Chang C-J et al (2008) A systematic review of silver-releasing dressings in the management of infected chronic wounds. Journal of Clinical Nursing 17(15): 1973-85. doi:10.1111/j.1365-2702.2007.02264
8. McIntosh C, Ivory JD, Gethin G (2019) Managing wound exudate in diabetic foot ulcers. Diabetic Foot Journal 22(1): 46–53
9. Nielsen J, Fogh K (2015) Clinical utility of foam dressings in wound management: a review. Chronic Wound Care Management and Research 2: 31–8. https://doi.org/10.2147/ CWCMR.S50832
This article is excerpted from the 《The Diabetic Foot Journal Vol 27 No 1 2024》by Wound World.


