Reducing length of hospital admission, where appropriate, is a stated aim of health services across the UK. As highlighted in the National Diabetes Foot Care Audit (NDFA), diabetes foot ulcer (DFU) patients occupy a large number of bed days. Between 2015 and 2018, over 90,000 bed days were occupied by foot disease-related admissions within 6 months of first expert assessment in the 211 participating centres of the NDFA, with a median length of stay of 9.0 days. There is a drive to reduce intravenous antibiotic use and move patients onto oral antibiotic therapy for the shortest possible duration to expedite discharge and reduce the risk of healthcare associated infection and the risks associated with antibiotic overuse. However, premature discharge can lead to readmission.
C-reactive protein (CRP) has been advocated as a measure of infection progress and prognosis in DFU patients but it has not been used directly to guide treatment. This observational retrospective audit sought to determine if CRP could be used to establish the optimum point for discharge of patients admitted with infected DFUs.
Patients and methods
From September 2019 to December 2021, we identified 198 admissions of 105 people with DFU admitted with foot ulcer infections. The patients were 84 men and 21 women, 19 with type 1 diabetes and 86 with type 2 diabetes. The average age was 60.8 years old (SD 14.1 years) and median duration of diabetes was 16.2 years at time of first admission (range 0–45 years). The median HbA1c was 66.5 mmol/mol (range 32–138 mmol/ mol) (8.2% (5.0-13.8%)), eGFR 54 (6–>60) and BMI 34 (range 18–57). Of the 105 people, 70 were being treated with insulin and 35 with non-insulin therapies. Only 45 had never smoked and 60 were ex- or current smokers. These are similar to other UK diabetes foot ulcer clinic populations.
Data were collected from the hospital patient record system Trak and from SCI-Diabetes, the Scottish National Diabetes Database. As this was a retrospective observational audit, rather than a prospective study, six admissions did not have an admission CRP (both were readmissions within one day of discharge) and 12 did not have a discharge CRP. There were, therefore, 186 discharge CRPs that could be used for analysis of the risk of readmission or major amputation or death within 12 weeks of discharge. CHI square tests were performed for 5, 10, 15, 20 and 25mg/l levels of CRP to determine the optimum CRP to discriminate between likelihood of remaining out of hospital or having an adverse outcome and an odds ratio with 95% confidence intervals was calculated. Patients who had more than one adverse outcome (i.e. readmission, amputation or death) were only counted once.
This was an audit of the outcomes of existing practice and, therefore, did not require separate ethical approval as covered under NHS Lothian clinical and research governance.
Results
The median number of admissions was 1 (range 1–6) with 56 patients only admitted once and 49 more than once. All had clinical infection at the time of admission. The bacterial species detected on culture are detailed in Table 1. Sixty-five per cent of the microbiological samples were tissue or liquid pus and only a third were from swabs. More than two-thirds of patients had polymicrobial cultures, but the predominant species were Staphylococci. There were only small numbers of MRSA and vancomycin-resistant Enterococci (VRE). One patient had no significant growth on culture but had changes of osteomyelitis on radiological examination.

The median length of admission was 21 days (range 1–204). In total, nine patients had a major amputation, including three patients progressing from minor or below-knee to above knee amputation. Fourteen patients died during the observational period within 12 weeks after discharge following admission for foot infection.
The median admission CRP was 83 (IQ range 27–196mg/l) and the median discharge CRP was 16 (IQ range 7–38mg/l). The odds ratios and confidence intervals for adverse events at 5mg/l intervals of CRP values are detailed in Table 2. Patients whose discharge CRP was over 10mg/l were significantly more likely to be readmitted or have another adverse outcome (amputation or death), OR 14.4 (95% CI 6.6–31.4, p<.0001) than any other CRP value, regardless of whether or not they were on oral antibiotics.
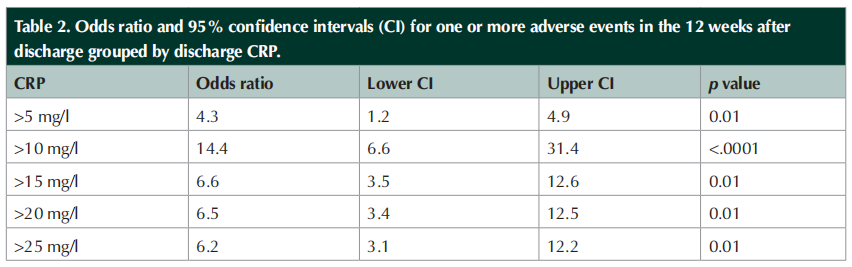
After publicising the findings of the first audit a second cohort of 58 admissions in 30 patients was used to determine if outcomes could be improved. In cohort two, 18 people were admitted once only and 12 were admitted more than once. The median admission CRP was 99mg/l and on discharge 6mg/l. Using a discharge CRP value of 11 or above mg/l as a cut-off resulted in an odds ratio of 17.9 (95% CI: 4.1–78.0, p=0.0001) for an adverse outcome, readmission or amputation.
Conclusions
The duration of admission for treatment of diabetes foot infection is typically determined by clinical measures alone. However, this risks the infection not being suppressed or resolved. Therefore, patients are at risk of readmission with a recurrence of infection, progression to amputation or death. Among the patients in the first cohort of the audit, 47% were readmitted or had another adverse outcome within 12 weeks of discharge following treatment for a diabetes foot infection and potentially this can be improved.
The high number of polymicrobial infections supports the view of the Infectious Diseases Society of America that patients admitted with diabetes foot infections should be initially treated with broad spectrum, usually combination antibiotic therapy. The choice of antibiotics will depend on local circumstances. However, the low numbers of anaerobes seen in this audit does not support the routine use of metronidazole in our patients. The guidelines on duration of antibiotic therapy suggest that shorter is better, but these are primarily based on consensus statements rather than randomised trials.
The high average HbA1c is similar to that seen in other diabetes foot clinic populations. Together with the high rate of current or ex smoking (compared to 41% in the NHS Lothian diabetes population as a whole). Current smoking is a strong predictor of poor healing, amputation and death in the national Diabetes Foot Care Audit of England and Wales. These factors have prompted a drive to improving diabetes control and encouraging smoking cessation in the people attending our diabetes foot clinic as part of our continuing efforts to improve outcomes and reduce cardiovascular mortality.
After making the results of cohort one known to the wider inpatient diabetes team, discharges from these wards with a CRP of >10mg/l reduced. The majority of discharges with a CRP of greater than 10mg/l were from the other main hospital in Edinburgh or surgical wards.
This audit shows that the higher a person’s discharge CRP, the greater the risk of that patient experiencing a subsequent adverse event (i.e. readmission, amputation or death). However, given that extending hospital stays is not itself without risk, clinicians must balance these risks when determining the optimum point of discharge. We suggest that waiting until the CRP is less than 10mg/l before discharging from hospital may represent a pragmatic balance of the risks of subsequent adverse events with the detrimental effects of extended hospital admission and excessive antibiotic use.
Acknowledgements
MY, CJ and JJ conceived edited and approved the content of the paper. They were no conflicts of interest or funding for this study. The authors would like to thank Emma Brewin, Stephanie Magill and Nasrin Khosravi, the permanent members of the diabetes foot clinic podiatry team, for their hard work in compiling the patient information.
References
1. Barwell ND, Devers MC, Kennon B et al; on behalf of the Scottish Diabetes Foot Action Group (2017) Diabetic foot infection: Antibiotic therapy and good practice recommendations. Int J Clin pract. 71: e13006
2. Hadavand F, Amouzegar A, Amid H (2019) Pro-Calcitonin, Erythrocyte Sedimentation Rate and C-reactive Protein in Predicting Diabetic Foot Ulcer Characteristics; a Cross Sectional Study. Archives of Academic Emergency Medicine 7(1): e37
3. Hauck K, Zhao X, Jackson T (2012) Adverse event rates as measures of hospital performance. Health Policy104(2): 146–54
4. Ince P, Kendrick D, Game F, Jeffcoate W (2007) The association between baseline characteristics and the outcome of foot lesions in a UK population with diabetes. Diabetic Medicine 24: 977–81
5. InterSystems Creative Data Technoology (2022). TrakCare Built for a Changing Healthcare World. Available at https://www.intersystems. com/au/products/trakcare (accessed 26.03.2022)
6. Jeandrot A, Richard JL, Combescure C et al (2008) Serum procalcitonin and C-reactive protein concentrations to distinguish mildly infected from non-infected diabetic foot ulcers: a pilot study. Diabetologia 51: 347–52
7. Lipsky BA, Berendt AR, Cornia PB et al (2012) Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections. Clinical Infectious Diseases 54(12): e132–73
8. National Institute for Health and Care Excellence (2015) NICE guideline [NG15] Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use. Available at https://www. nice.org.uk/guidance/ng15 (accessed 26.03.2022)
9. NHS Digital (2019) National Diabetes Footcare Audit Fourth Annual Report. Available at https://files.digital.nhs.uk/FC/18ED7F/ NDFA%204AR%20-%20Main%20Report%20v1.1.pdf (accessed 26.03.2022)
10. NHS England (2022) Reducing length of stay. Available at https://www. england.nhs.uk/urgent-emergency-care/reducing-length-of-stay/ (accessed 26.03.2022)
11. NHS Scotland (2020) Scottish Diabetes Survey 2020. Available at www.diabetesinscotland.org.uk/wp-content/uploads/2022/01/ Diabetes-Scottish-Diabetes-Survey-2020.pdf (accessed 26.03. 2022)
12. Scottish Care Information Diabetes Collaboration (2022) SCI-Diabetes home page. Available at https://www.sci-diabetes.scot.nhs.uk/ (accessed 26.03.2022)
13. van Asten SAV, Jupiter DC, Mithani M et al (2017) Erythrocyte sedimentation rate and C-reactive protein to monitor treatment outcomes in diabetic foot osteomyelitis. Int Wound J 14: 142–48
14. Young MJ, McCardle JE, Randall LE, Barclay JI (2008) Improved survival of diabetic foot ulcer patients 1995-2008: possible impact of aggressive cardiovascular risk management. Diabetes Care 31(11): 2143–47
This article is excerpted from the 《The Diabetic Foot Journal Vol 27 No 1 2024》 by Wound World.