Diabetic foot ulcers are often refractory to medical and surgical therapies and responses to treatment likely depend on the stages of angiopathy and peripheral neuropathy (Coppelli et al, 2018).
In the advanced stage of diabetes, angiopathy progresses to a pathological state termed “diabetic macroangiopathy”, which can lead to the development of peripheral arterial disease (PAD), characterised by the obstruction of arteries with diameters >1mm. Diabetic foot ulcers in patients with PAD typically respond poorly to therapeutic interventions, frequently resulting in limb loss.
Foot ulcers in patients with early diabetes, when angiopathy is at the stage of microangiopathy, typically have positive responses to medical and surgical therapies in hospital settings. However, foot ulcers may heal at an unexpectedly slow rate in some patients, despite close control of blood glucose levels and normal peripheral limb circulation, indicating the existence of unknown factors specific to people with diabetes that inhibit wound healing and are not related to peripheral blood flow.
Many studies have reported risk factors for poor treatment responses in patients with diabetic foot ulcers. The majority of these studies used binary variables, such as amputation or ulcer healing at certain time points (e.g. 1 year) after major therapeutic interventions (Fife et al, 2016; Hicks et al, 2018; Kee et al, 2019; Ezeani et al, 2020; Linn et al, 2020; Zhu et al, 2022). These correlations predict long-term clinical outcomes, but do not predict the healing capacity of individual wounds. The prediction of wound healing capacity is important when determining the most appropriate therapeutic strategy based on clinical factors, such as the presence of PAD or a history of poor glycaemic control, on a weekly basis in specific patients.
Aims
We aimed to identify unknown causes of impaired healing capacity in patients with diabetic foot ulcers and develop novel indices for measuring these factors.
In addition to total healing period (THP) of foot ulcers, we developed two novel indices as objective variables — granulation time (GT) and time to contraction onset (TCO). These indices represent specific aspects of the wound healing process. We then used eight factors that are presumed to affect the healing process of diabetic foot ulcers: patient age, age at diabetes onset, sex, PAD, HbA1c, Brinkman index (BI), receipt of dialysis and presence of bone infection.
The BI is commonly used to estimate the cumulative dose of smoking. It is calculated by multiplying the number of cigarettes smoked per day by the number of years of smoking.
Univariate and multivariate linear regression analyses were used to determine the correlations between these eight factors and the three wound healing indices as objective variables.
Patients and methods
Patients
The study comprised 59 patients with diabetic foot ulcers who received treatment between April 2014 and September 2019 at two facilities: Asahi General Hospital, Asahi, Chiba Prefecture, Japan and Tohoku Medical and Pharmaceutical University Hospital, Sendai, Miyagi Prefecture, Japan. Of these, 38 patients were included in the study analysis, with 21 excluded due to incomplete records of the wound healing process, amputation, transfer to another hospital, failure of healing or death before healing.
Methods
As indices that are likely to reflect different aspects of the wound healing process, we designated three objective variables, THP, GT and TCO.
THP is the number of days from the start of therapeutic interventions to complete healing. GT is the number of days from the last debridement to a state in which 100% of the raw surface was covered with good granulation tissue. TCO is the number of days from the last debridement to the onset of progressive wound contraction. GT and TCO were determined by daily examination of ulcers and subjective evaluation of photographs taken by the first author (KT).
Photographs of the affected foot were taken two to three times per week. In TCO, “contraction onset” was determined as the day when the wound surface had decreased to under 80% of the original area on the day of the last debridement. The size of the wound on the photograph was calculated using free software which counts the number of pixels in a defined area. A scale was included in photographs as an internal control.
Eight factors that were assumed to affect the healing process of ulcers were included as explanatory variables: patient age (years) on the day of hospitalisation (H-Age), patient age (years) at the onset of diabetes (O-Age), sex (1 for male, 0 for female), presence of PAD defined as a skin perfusion pressure ≤40 mmHg or clinically apparent manifestation of ischaemia of the affected foot, e.g. no pulsation of the arteries, cyanosis, or ischaemic gangrene (1 if any were present, otherwise 0), HbA1c (%), BI, receipt of haemodialysis (HD; 1 for HD, 0 not receiving HD), presence of osteomyelitis (1 if present, otherwise 0).
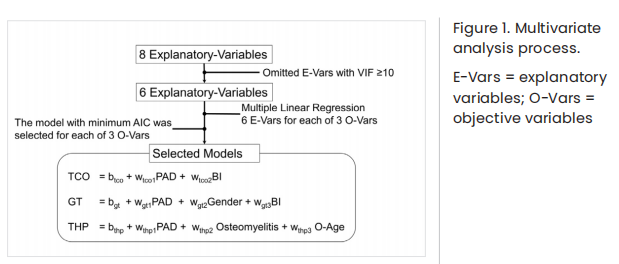
Firstly, we performed a simple linear regression analysis to determine the correlations between each of the eight explanatory variables and each of the three objective variables. The second phase of evaluation used multivariate linear regression analysis, where the explanatory variables with a variance inflation factor (VIF) that exceeded 10 were omitted to avoid multicollinearity. The linear regression models included all combinations of explanatory variables and the model with the lowest Akaike information criterion (AIC; an estimator of prediction error) was selected for each objective variable. Each selected model was identical to the one selected using the stepwise regression method with AIC (backward elimination). All statistical analyses were performed with Python (version 3.8.8). Statsmodels (version 0.12.2, a library of Python) was used for linear regression analyses [Figure 1].
This study was conducted in accordance with ethical standards and was approved by the ethics committee of Tohoku Medical and Pharmaceutical University Hospital.
Results
The characteristics of the explanatory variables are shown in Table 1. Most patients were men (78.9%), seven patients (18.4%) were receiving regular HD, and 16 patients (42.1%) had active osteomyelitis at some point during the hospitalisation period. In the simple linear regression analysis, THP was positively associated with PAD. GT was positively associated with H-Age, PAD, and BI, and inversely associated with HbA1c. TCO was positively associated with PAD [Table 2].
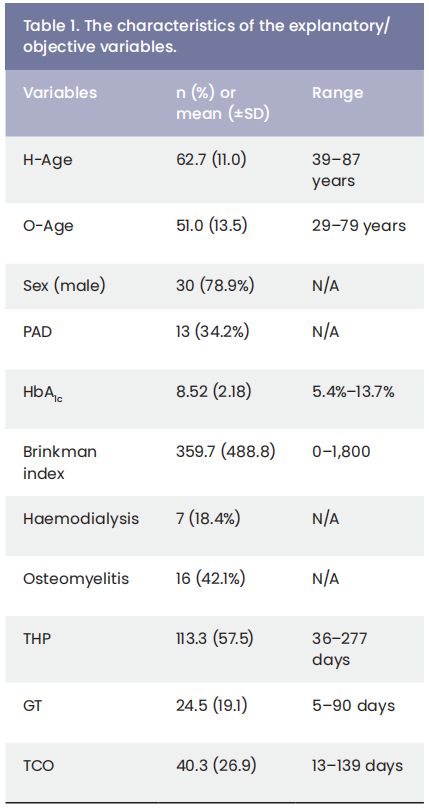
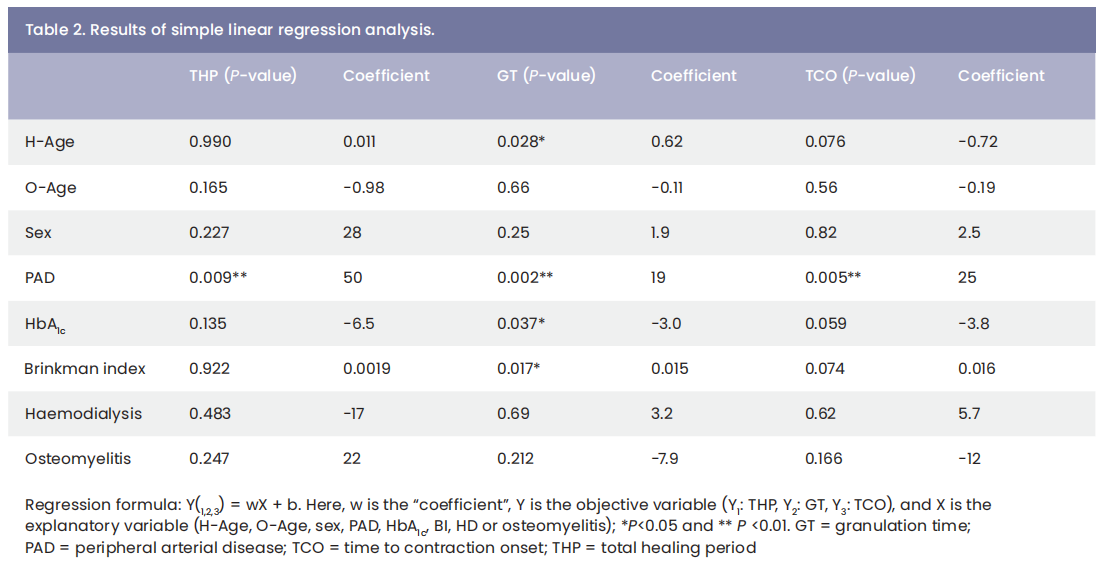
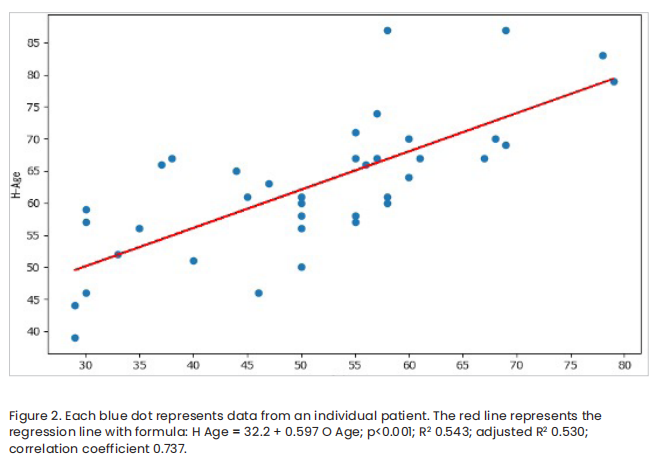
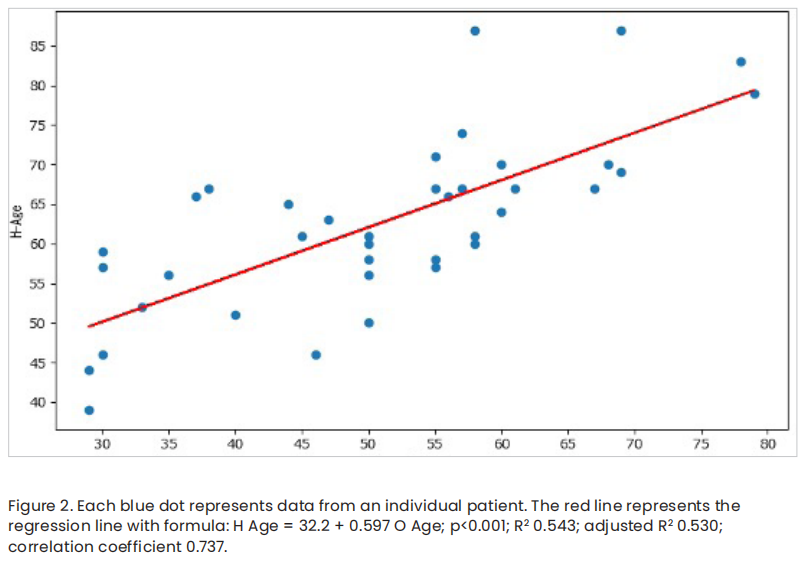
Before the multivariate linear regression analysis, multicollinearity between explanatory variables was assessed, with H-Age, O-Age, and HbA1c found to have VIF >10 [Table 3]. The VIFs of H-Age and O-Age were 64.2 and 43.4, respectively. The VIF of O-Age was <10 when H-Age was removed from the analysis, whereas the VIF of H-Age was substantially reduced but still exceeded 10 when O-Age was removed. Furthermore, a strong correlation was observed between these two variables based on Pearson’s product-moment correlation coefficient [Figure 2]. Accordingly, we decided to omit H-Age from the study analysis.
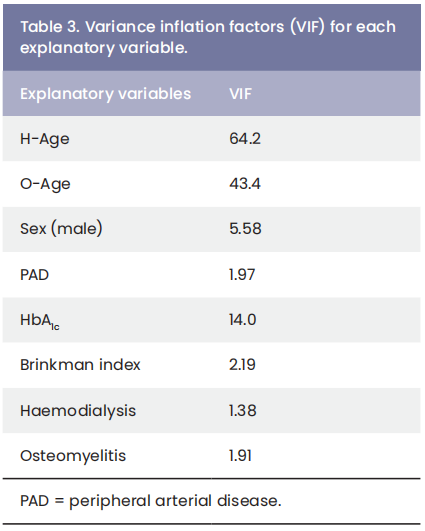
As the VIF of HbA1c exceeded 10 and was not correlated with any specific explanatory variable, the reason for the multicollinearity of HbA1c was considered to be multifactorial. Further analysis revealed a significant trend toward lower HbA1c levels in patients regularly receiving HD compared to patients not receiving HD (Mann-Whitney U test: P=0.0079); however, this result may have been biased due to HbA1c having a VIF >10. Therefore, multivariate linear regression was used to evaluate the correlations between each of the three objective variables and the remaining six variables (O-Age, gender, PAD, BI, HD and osteomyelitis).
The multivariate linear regression model was optimised for each objective variable according to minimum AIC selection. The model for THP comprised O-Age, PAD, and osteomyelitis as explanatory variables. THP was positively correlated with PAD. The model for GT comprised gender, PAD, and BI as explanatory variables. GT was positively correlated with BI and PAD. The model for TCO comprised PAD and BI as explanatory variables. TCO was positively correlated with PAD [Table 4].
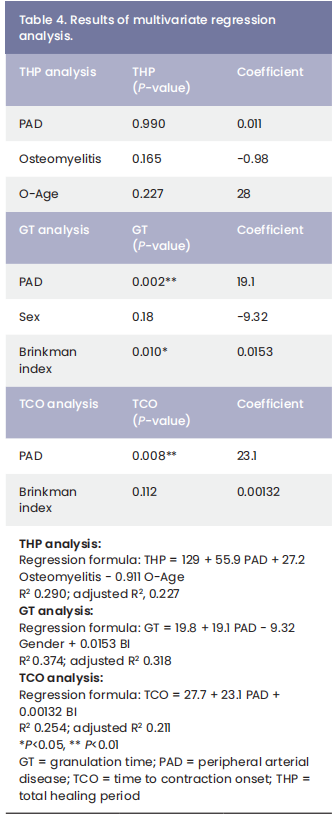
In the multivariate linear regression analyses, the regression coefficients of selected explanatory variables were interpreted as follows. The mean THP was 55.9 days longer in patients with PAD, 27.2 days longer in patients with osteomyelitis, and 0.911 days longer if the onset of diabetes was more than 1 year prior to admission. The mean GT was 19.1 days longer in patients with PAD, 9.32 days longer in female patients, and 1.53 days longer for each increase in the BI of 100. The mean TCO was 23.1 days longer in patients with PAD and 0.132 days longer for each increase in the BI of 100. Among the selected explanatory variables, only PAD was significantly associated with each of the objective variables, whereas GT was only significantly associated with the BI.
Discussion
To better gauge the wound healing capacity of diabetic foot ulcers, we introduced two new variables, GT and TCO, alongside the traditional THP. These new indices focused on some partial aspects of wound healing, granulation formation and wound contraction, and thus could be sensitive to small variations in healing ability, which is crucial for tailoring patient specific treatments.
The eight explanatory variables used in the study analysis are routinely evaluated in diabetic foot ulcer clinics as they are considered to provide information on wound healing capacity. H-Age was omitted from the multivariate linear regression analysis as it was significantly correlated with O-Age [Figure 2]. This correlation may be explained by earlier onset of diabetes leading to earlier age a hospitalisation and vice versa.
Similarly, HbA1c was omitted from the multivariate linear regression analysis due to its multicollinearity with regular HD (dialysis). This is likely to be because both are influenced by conditions like renal failure and anaemia, which shorten the lifespan of blood cells and thus lower HbA1c levels.
Consequently, multivariate linear regression analyses were performed to determine the associations between each of the objective variables and the remaining six explanatory variables. After minimum AIC selection, a multivariate linear regression model for each objective variable was optimised with two or three parameters out of the six selected explanatory variables to increase best fitting and simplicity by restricting the number of explanatory variables.
In both simple linear regression and multivariate linear regression analyses, PAD was significantly associated with THP, GT and TCO. In each analysis, the coefficient value for PAD was the largest compared to all other binary explanatory variables. This result indicates that PAD significantly and negatively affects wound healing in patients with diabetic foot ulcers, as shown by many previous studies. The coefficient of PAD to THP was 55.9 days in the multivariate linear regression, which implies that PAD delays discharge from hospital by almost 2 months.
The multivariate linear regression analyses performed in the present study also demonstrated that the BI was significantly associated with GT and there was a trend toward decreasing THP with increasing O-Age, although this association did not reach statistical significance. Smoking is a recognised risk factor for delayed wound healing owing to the toxic chemicals in smoke, including nicotine, carbon monoxide and hydrogen cyanide. Nicotine is a vasoconstrictor that reduces blood flow to the skin, thereby resulting in tissue ischaemia and impaired healing of injured tissues. Carbon monoxide diminishes oxygen transport and metabolism, while hydrogen cyanide inhibits the enzyme systems necessary for oxidative metabolism and oxygen transport at the cellular level (Silverstein, 1992). According to a systematic review by Sørensen (2012), smoking attenuates epidermal regeneration and neovascularisation. These phenomena are likely to be at least partly caused by impaired epithelial and endothelial proliferation, and also by reduced collagen production by fibroblasts, which negatively affects tissue proliferation and remodelling. Even after smoking cessation, epidermal regeneration, fibroblast proliferation, and collagen production remain impaired, whereas tissue oxygenation, neutrophil function, monocyte-macrophage function, and antibacterial immunity are rapidly restored. Given these smoking-related effects on wound healing, the positive correlation between GT and BI values may be attributable to longterm smoking accumulatively and irreversibly compromising the granulation process in foot ulcers, which requires collagen production by fibroblasts.
Conversely, prolonged high blood glucose levels in patients with long-lasting diabetes are thought to impair the microvascular circulation in foot tissues (Abularrage et al. 2005; Sharma et al, 2020). Although O-Age, which partly reflects the duration of diabetes, was not significantly associated with the wound healing-related objective variables examined in the present study, persistent hyperglycaemia may cause subclinical vascular impairment and therefore delay the wound healing process. Hyperglycaemiainduced vascular damage is associated with increased intracellular accumulation of reactive oxygen species in vascular cells, which are both initiators and final effectors of four hyperglycaemia-driven mechanisms, namely the polyol pathway, formation of advanced glycation end-products, the protein kinase C-diacylglycerol pathway and hexosamine pathways (Hicks et al, 2018; Madonna and De Caterina, 2011).
Recently, AGEs have been shown to play an important role in the pathogenesis of arteriosclerosis by causing microvascular inflammation. As AGE-modified collagens are resistant to degradation and persistent in the vasculature of diabetic patients, they act as a “metabolic memory” and continuously damage microvessels (Yamagishi et al, 2017).
Taken together, these findings suggest that prolonged hyperglycaemia and long-term smoking may lead to subclinical peripheral angiopathy and/or fibroblast dysfunction, eventually resulting in diabetic foot ulcers that are refractory to treatment in patients without evidence of peripheral vascular disorder.
Conclusion
The present study evaluated factors that may affect the healing speed of diabetic foot ulcers. PAD was associated with delayed wound healing according to every measure analysed. The BI was significantly associated with slower granulation formation. The measurement of GT, and possibly TCO, may have utility in predicting the healing capacity of individual ulcers and may contribute to decision making regarding the most effective therapies for patients with diabetic ulcers, as well as estimating the likely time to healing. Future work will aim to develop an artificial intelligence system capable of autonomously recognising granulation tissue and measuring contraction speed, thereby providing instantaneous insights into the healing capabilities of each diabetic foot ulcer.
References
1. Abularrage CJ, Sidawy AN, Aidinian G et al (2005). Evaluation of the microcirculation in vascular disease. J Vasc Surg 42(3): 574–81
2. Coppelli A, Abbruzzese L, Goretti C et al (2018) Does microangiopathy contribute to the pathogenesis of the diabetic foot syndrome? In: Piaggesi A, Apelqvist J (eds.). The diabetic foot syndrome. Frontiers in Diabetes. Karger, Basel: pp 70–82
3. Ezeani IU, Ugwu ET, Adeleye FO et al (2020) Determinants of wound healing in patients hospitalized for diabetic foot ulcer: results from the MEDFUN study. Endocr Regul 54(3): 207–16
4. Fife CE, Horn SD, Smout RJ et al (2016) A predictive model for diabetic foot ulcer outcome: the Wound Healing Index. Adv Wound Care 5(7): 279–87
5. Kee KK, Nair HKR, Yuen NP (2019) Risk factor analysis on the healing time and infection rate of diabetic foot ulcers in a referral wound care clinic. J Wound Care 28(Suppl 1): S4–13
6. Linn YL, Chan SL, Soon SXY et al (2020) Heal or no heel: outcomes of ischaemic heel ulcers following lower limb revascularization from a multi-ethnic Asian cohort in Singapore. Int Wound J 17(6): 2010–8
7. Madonna R, De Caterina R (2011) Cellular and molecular mechanisms of vascular injury in diabetes – part I: pathways of vascular disease in diabetes. Vascul Pharmacol 54(3-6): 68–74
8. Sharma S, Schaper N, Rayman G (2020) Microangiopathy: is it relevant to wound healing in diabetic foot disease? Diabetes Metab Res Rev 36(Suppl 1): e3244
9. Silverstein P (1992) Smoking and wound healing. Am J Med 93(Suppl 1A): 22S–4
10. Sørensen LT (2012) Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg 147(4): 373–83
11. Yamagishi SI, Nakamura N, Matsui T (2017). Glycation and cardiovascular disease in diabetes: a perspective on the concept of metabolic memory. J Diabetes 9(2): 141–8
This article is excerpted from the Wounds International 2024 | Volume: 15 Issue: 1 by Wound World.