Optimising glycaemic control is important to reduce risks of diabetes complications and mortality, and to improve wellbeing. In the UKPDS (UK Prospective Diabetes Study), a 1.0% HbA1c reduction was associated with a 37% reduction in microvascular complications and a 21% reduction in diabetes-related death (Stratton et al, 2000). The ADA and EASD Consensus Report on the Management of hyperglycaemia in Type 2 diabetes 2022 highlights the importance of physical activity, providing guidance on Stepping, breaking up prolonged Sitting, Sweating and Strengthening, as well as optimising Sleep (Davies et al, 2022). The report recommends at least 150 minutes of moderate to vigorous activity or 75 minutes of vigorous activity per week spread over 3 days, with no more than two consecutive days of inactivity. In addition, strength, flexibility and balance training are recommended two to three times a week (see Brown, 2022). The report also summarises the expected impact of the different types of physical activity on glucose, HbA 1c, lipids, physical function, depression and quality of life. However, the optimal dose and type of physical activity to maximise impact on glycaemia remains unknown.
In this systematic review and meta-analysis published in Diabetes Care, Gallardo-Gómez and colleagues examined the dose–response relationship between physical activity and HbA1c using data from 126 studies, mainly in the US and UK, involving a pooled 6718 participants with type 2 diabetes. Baseline HbA1c was used to allocate participants into four groups, as defined by the American Diabetes Association (2014):
● Prediabetes (<48 mmol/mol).
● “Controlled” type 2 diabetes (48 to <53 mmol/ mol).
● “Uncontrolled” type 2 diabetes (53–64 mmol/ mol).
● “Severely uncontrolled” type 2 diabetes (>65 mmol/mol)
Since 2017, there has been a move away from using stigmatising language in diabetes care (Dickinson et al, 2017), and terms such as “controlled” and “uncontrolled” glycaemia are no longer appropriate, so we can instead use the participants’ baseline HbA1c value alone to identify their group for the analyses.
Results
The optimal dose of physical activity identified to optimise HbA1c was 1100 Metabolic Equivalents of Task (MET)-minutes per week, and interestingly, this was the same irrespective of baseline HbA1c. The authors used the Compendium of Physical Activities to translate this activity dose into minutes per week of specific activities, such as just over 36 minutes of moderate-paced brisk walking daily (see Table 1 for other equivalents).
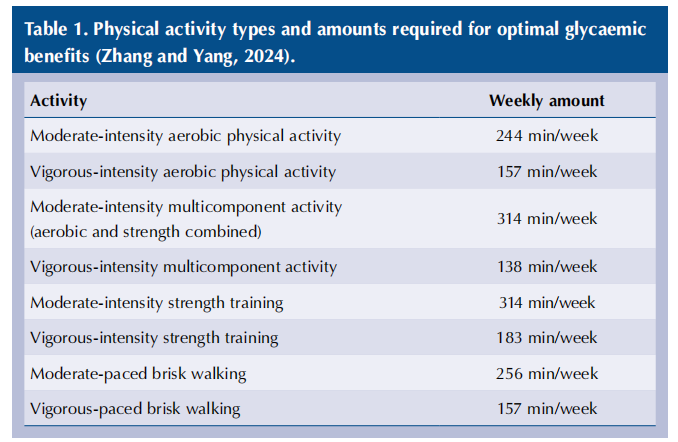
This is more than both the ADA/EASD recommendations and the 150 minutes of moderate activity and 75 minutes of vigorous activity recommended for adults without diabetes in the UK (Davies et al, 2019). In this study, multicomponent (strength and aerobic activity combined), strength training and brisk walking were the most effective activities.
As expected, achieving the optimal weekly MET dose had the greatest impact in the group with baseline HbA1c >64 mmol/mol, achieving HbA1c reductions of 0.66–1.02%. Significant reductions were also achieved in the other groups:
● 0.49–0.64% in those with baseline HbA1c 53–64 mmol/mol.
● 0.40–0.47% in those with baseline HbA1c 48–53 mmol/mol – roughly similar to adding a DPP-4 inhibitor to treatment.
● 0.24–0.38% in those with prediabetes (baseline HbA1c <48 mmol/mol) – enough to reduce risk of progression to type 2 diabetes.
The study also identified the minimal doses of physical activity required to move between different HbA1c groups according to baseline HbA1c. The minimal physical activity dose range required to improve by one glycaemic category was calculated to be as low as the following:
● 150–810 MET-minutes per week for people to move from a baseline HbA1c of 65 or 70 mmol/mol, respectively, to 53–64 mmol/mol.
● 330–990 MET-minutes per week to move from HbA1c 54 or 58 mmol/mol, respectively, to 48–53 mmol/mol.
● 570–900 MET-minutes per week to move from HbA1c 49 or 51 mmol/mol, respectively, to prediabetes.
Discussion
A MET, or “metabolic equivalent of task”, is a measure of the oxygen uptake for a given activity compared to resting oxygen consumption, with resting consumption designated as 1 MET. Some examples of activities and their MET values are shown in Table 2. Most of us are unfamiliar with discussing activity by MET values, so the translation of these findings to hours of weekly activity provided in the associated comment piece (Zhang and Yang, 2024) and taken from the supplementary material to the full paper is useful.
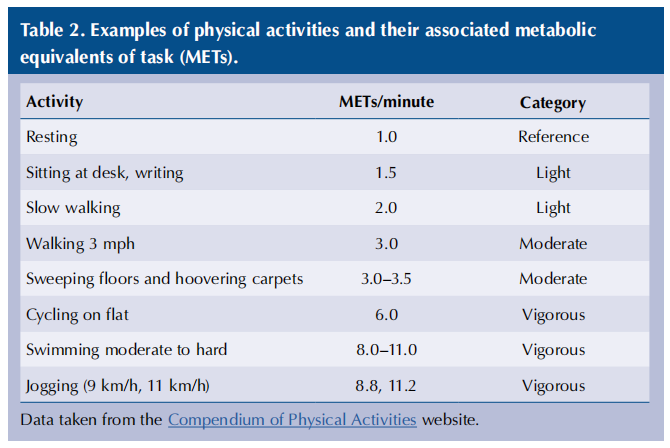
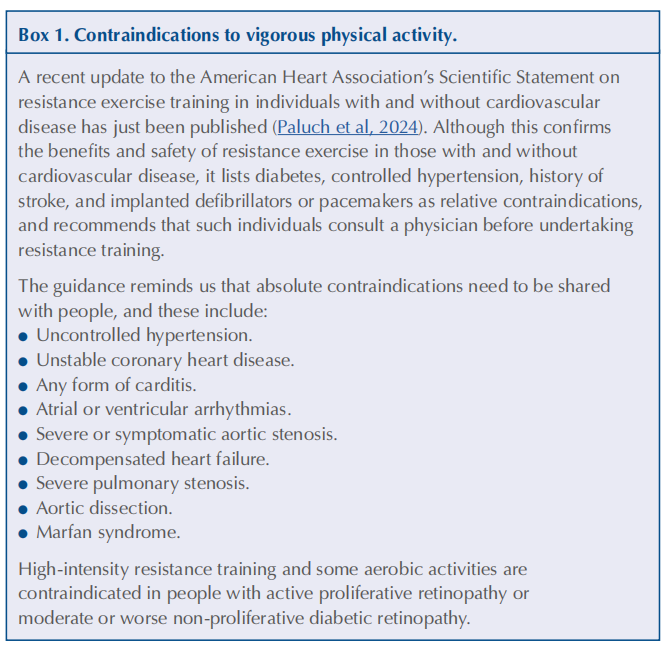
To help people understand the intensity of an activity, we can explain that during light activities they should be able to both talk and sing; when pursuing moderately vigorous activities, they would be able to talk but not sing; and during vigorous activity – which may need clinician assessment beforehand (see Box 1) – it is hard to talk in sentences.
In their associated comment, Zhang and Yang recognise the individualised and more specific and user-friendly types of physical activity examined in this review compared to previous studies, and how this may improve real-world
Some limitations to this study were identified. Although the optimal dose of physical activity is now clearer, the duration over which these activity levels need to be maintained to achieve HbA1c changes remains unclear, since the included studies varied in length and design. Furthermore, although a J-shaped curve of HbA1c versus activity was identified, this was not a symmetrical J shape and may have been limited by lack of data on individuals with very high activity levels; further randomised controlled trials with varying levels of activity intensity are recommended. Trials involving people with severe health conditions, such as mental health problems, were excluded from the analysis and, therefore, these findings cannot be extrapolated to all people with type 2 diabetes.
Implications for practice
Helping people with diabetes make lifestyle changes to improve glycaemia, cardiovascular risk and general health is an important role for healthcare professionals. This study provides us with the data to help people with type 2 diabetes quantify the activity needed to achieve the greatest impact on their HbA1c. Rather than offer generic recommendations, we can now encourage people to tailor their weekly activity plan to optimise personal glycaemic impact.
However, the types of activity encouraged must take into account any individual diabetes complications or comorbidities. Professor Tom Yates offers a how-to guide on this, as well as providing a ready-made, self-administered walking programme we can share with people with diabetes.
These analyses suggest that people with diabetes may need more physical activity than previously recommended to optimise its glycaemic impact. Since we know that many do not achieve current recommendations consistently, helping people undertake these doses of physical activity is likely to need support from a multidisciplinary team, including exercise professionals and coaches, as well as from family and friends.
References
1. American Diabetes Association (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37(Suppl 1): S81–90
2. Brown P (2022) So what should we recommend to people with diabetes about lifestyle? Updated ADA/EASD advice. Diabetes & Primary Care 24: 157
3. Davies SC, Atherton F, McBride M, Calderwood C (2019) UK Chief Medical Officers’ Physical Activity Guidelines. Available at: https://bit.ly/49zBJYO
4. Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycaemia in type 2 diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65: 1925–66
5. Dickinson JK, Guzman SJ, Maryniuk MD et al (2017) The use of language in diabetes care and education. Diabetes Care 40: 1790–9
6. Paluch AE, Boyer WR, Franklin BA et al; American Heart Association (2024) Resistance exercise training in individuals with and without cardiovascular disease: 2023 update: A Scientific Statement From the American Heart Association. Circulation 149: e217–31
7. Stratton IM, Adler AI, Neil HA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 321: 405–12
8. Zhang C, Yang J (2024) Personalizing physical activity for glucose control among individuals with type 2 diabetes: Are we there yet? Diabetes Care 47: 196–8
This article is excerpted from the Diabetes & Primary Care Vol 26 No 1 2024 by Wound World.