Methods
Study design and ethical approval
Ethics Committee Approval was taken from the JPN Apex Trauma Centre (JPNATC), All India Institute of Medical Sciences, New Delhi, India with approval numbers IEC-265/04.05.2018, AA-4/05.04.2019, RP-2018/19.
Between 2019 and 2021, patients aged ≥18 years who presented with trauma/complex wounds were enrolled in the study and received NPWT therapy using the InoHeal Wound Healing System developed by Inochi Care Private Limited, New Delhi, India. The device is electronically powered with a suction pump unit that can provide regulated negative pressure in the range of -40 to–200mmHg. It has a disposable, transparent 500ml capacity canister that gets attached to the device and collects wound exudates. During the NPWT session, a polyurethane foam with a pore size of 400–600mm is placed on the wound bed for dressing purposes and the foam gets connected to the InoHeal device using connectors. Each therapeutic cycle lasts up to 72 hours and is set at a continuous negative pressure.
All enrolled participants were told how the NPWT system worked and the therapeutic goals of the study. Written informed consent was obtained from all the participants before their enrollment in the study. The confidentiality and privacy of the patients were protected. Each patient was assigned a specific patient ID (PID- 001, 002, etc.,) to maintain the privacy of the enrolled patients.
Inclusion criteria
Only participants fulfilling the following inclusion criteria were enrolled in the study.
■Age ≥18 years and ≤70 years
■Presence of an exuding wound
■Presence of a wound that was not healing in a timely manner
■Agreement and ability to sign the informed consent form.
Exclusion criteria:
Participants falling under the following categories were excluded from the present study.
■Pregnant woman
■Simultaneous participation of patients in another interventional study
■Untreated osteitis or osteomyelitis
■Not examined/unexplored fistulal
■Malignancy of the wound
■Exposed nerves, blood vessels, anastomotic sites.
Negative pressure wound therapy
All enrolled subjects in the study were given NPWT on the basis of wound characteristic, wound size, increase in granulation tissue and length of hospital stay. To provide NPWT, a foam-based, biocompatible wound dressing was applied to the wound and covered by the biocompatible adhesive drape that tightly seals the wound dressing at the wound bed and helps in creating a sealed environment at the wound bed.
The NPWT device is a commercially developed electronic device. The device is not a disposable unit and comes with a single use disposable canister. The NPWT device comes with customised tubings that connect to the foam dressing on one end, and to the NPWT device at the other. The NPWT device can be operated in the range of -40 to –200mmHg and health professionals can decide on the negative pressure setting based on the wound type and severity of the wound (Agarwal et al, 2019). The hospital and nursing staff took care of maintaining and overseeing regular operation of the NPWT device after obtaining necessary instructions from the clinician. The medical history of the patients was taken at the time of enrolment. The healthcare professionals involved in the study were provided training to use the NPWT device before the start of the study. The family members of the enrolled patients were taught how to manage in circumstances, such as recharging the device and immediate reporting of the alarm to hospital staff.
Outcome measures
The primary outcome measures were wound healing outcomes based on Bates-Jensen Score and the device safety. The wound was debrided and NPWT therapy was provided up to 72 hours for each session.
Measurement of Bates-Jensen Score
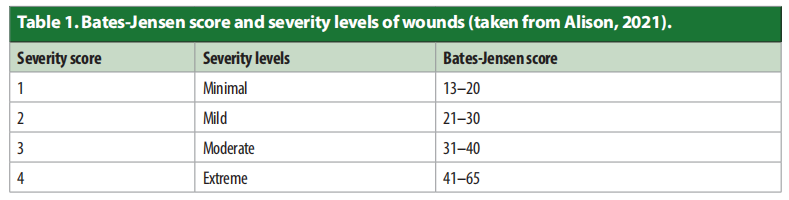
The Bates-Jensen Wound Assessment Tool (BWAT) is a useful scoring system to understand the wound healing process during a therapeutic intervention (Bates-Jensen et al, 2019). The scoring system independently scores 13 parameters to assess the wound health. In BWAT, a sub score of 1 for a parameter indicates a “non-harmful” clinical situation while a sub score of 5 is an indicator of an “extremely necrotic” clinical situation. The final sum for all 13 parameters is summed up to obtain the Bates-Jensen score for a wound. The 13 wound parameters of BWAT are: size, depth, edges, undermining, necrotic tissue type, necrotic tissue amount, exudate type, exudate amount, skin colour surrounding wound, peripheral tissue oedema, peripheral tissue induration, granulation tissue and reepithelialisation. Importantly, BWAT helps in evaluating the wound severity based on the overall BWAT score [Table 1]. In our study, BatesJensen score was calculated for all wounds independently by two researchers.
Results
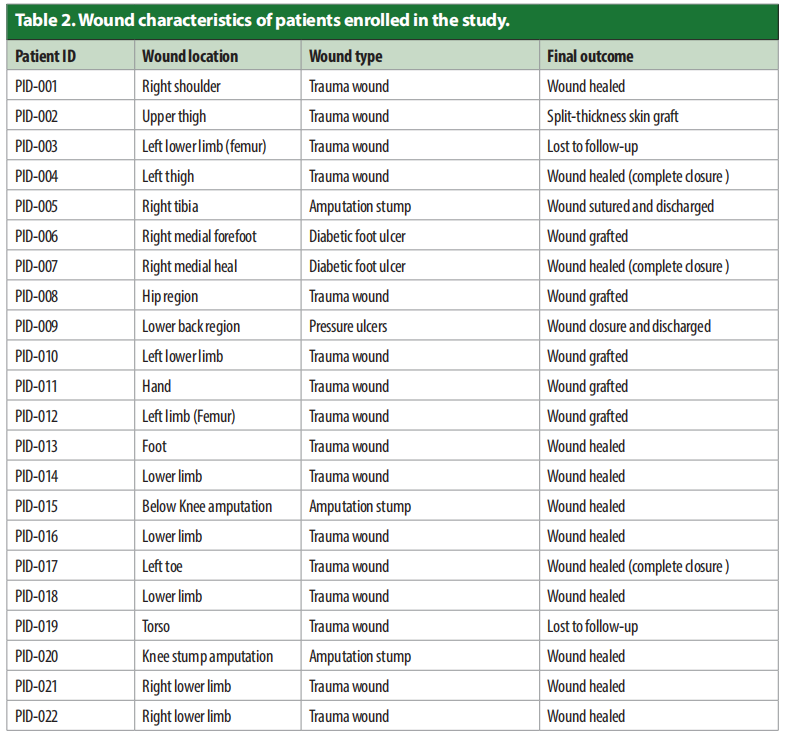
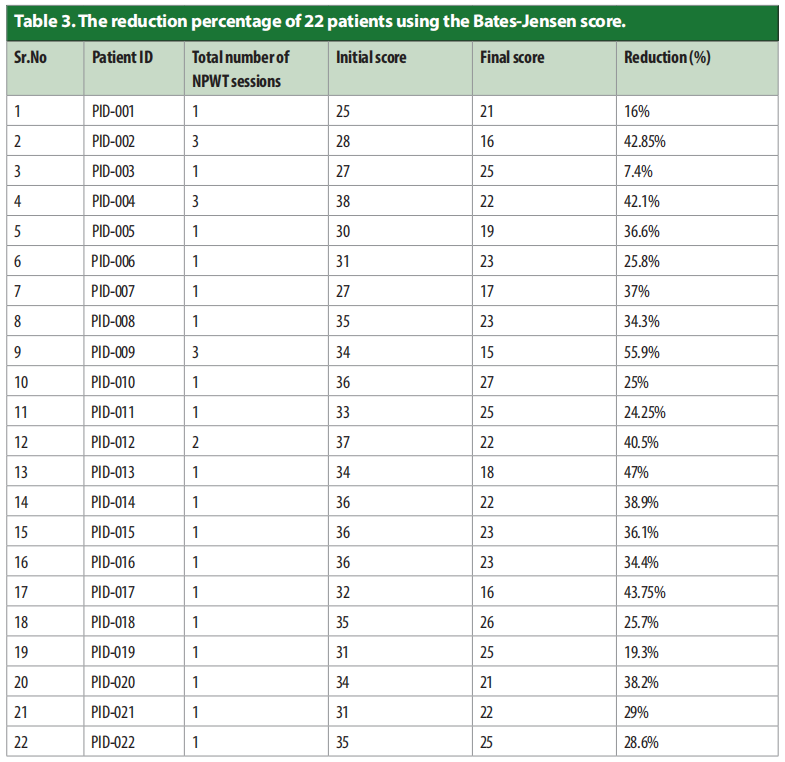
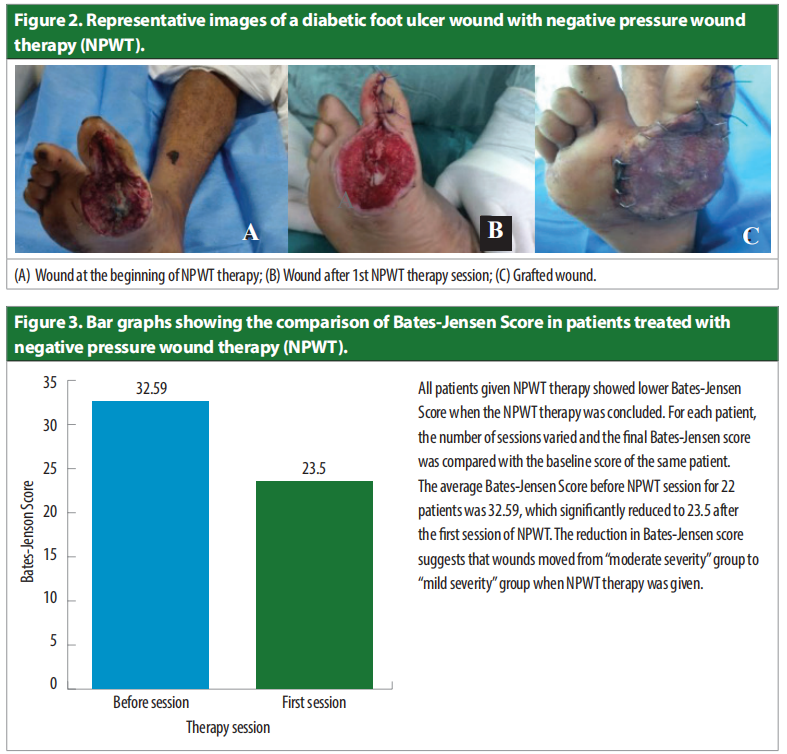
In this study, 22 patients were enrolled the wound characteristics are shown in Table 2. A summary of patient ID, wound location, wound type, and the final treatment outcome is presented in Table 3. As shown in Table 3, a majority of wounds fall in the category of trauma wounds (16/22; 72.7 %), followed by amputation stumps (3/22; 13.6; %), DFUs (2/22; 9.09%) and pressure ulcers (1/22; 4.54%). Clinical outcomes demonstrated that several wounds showed wound healing post-NPWT. In our analysis, we did not include wound length in calculating the Bates-Jensen Score due to non-availability of scale in the patient pictures and, therefore, the Bates-Jensen Score reported in the present study is a sum of 12 parameters. All wounds [Figures 1–2] were analysed using the Bates-Jensen Scoring system and the final score for all 12 items obtained after summing up the score assigned to individual items. We observe that the average Bates-Jensen score significantly reduced after the first session of NPWT therapy (32.59 versus 23.5; n=22, ***P<0.001; Figure 3), indicating that NPWT sessions given to patients improved wound healing and wound health. The reduction in the average Bates-Jensen score for 22 patients shows that wounds moved from “moderate severity” to “mild severity” group. All patients given NPWT therapy showed a decline in BatesJensen score [Table 3], an indicating that NPWT is therapeutically effective in improving wound healing in a wide-range of complex and nonhealing wounds.

Discussion
NPWT or vacuum-assisted wound closure has been in clinical practice since the early 1990s to accelerate wound healing. In NPWT, the wound is covered using a wound dressing and a connected device creates a controlled subatmospheric pressure in the wound bed to remove the wound exudate and collects the wound exudate in a container attached to the device. The use of NPWT has gained widespread acceptance in clinical settings for wound management and wound care (Meloni et al, 2015; Raj et al, 2020; Zens et al, 2020). NPWT works by reducing oedema, lowering the risk of microbial infection, removing exudate, and promoting tissue granulation (Ramula et al, 2020). A prospective controlled study by Ramula et al (2020) in non-healing ulcer patients reported higher patient discharge rate and better granulation tissue appearance in patients given NPWT therapy as compared with the conventional dressing group.
In the present study, the therapeutic efficacy of a newly developed NPWT system was assessed using improvement in BatesJensen score (InoHeal Wound Healing System, Inochi Care Private Limited, New Delhi, India) in a tertiary care hospital (AIIMS, New Delhi, India). We used the Bates-Jensen Score to measure the therapeutic efficacy of the InoHeal system. A lower score on Bates-Jensen Score is a reflection of wound healing, and wounds following the normal wound healing process show a gradual decline in the Bates Jensen Score. The Bates-Jensen Wound Assessment Tool is a globally accepted tool to measure wound health and evaluate the therapeutic efficacy of clinical interventions. In our study, we evaluated Bates-Jensen Score after each NPWT session and calculated a composite score for all the parameters considered in Bates-Jensen Score. In our analysis, we omitted wound length due to non-availability of scale in the patient pictures and, therefore, we calculated the Bates-Jensen Score using 12 parameters.
Interestingly, all patients showed a gradual decline in Bates Jensen Score, an indication of improved wound bed and wound health. An average of 22 Bates-Jensen Scores before NPWT session and after the first session of NPWT showed a significant decline in BatesJensen Scores (Figure 3; n=22; 32.5 versus 23.5; ***P<0.0001). A significant reduction in the Bates-Jensen Score post-NPWT therapy suggests that NPWT improved the healing process. However, the reduction in BatesJensen Scores as displayed in Table 2 was not the same for each patient and reduction in the score was in the range of (7.4% to 55.9%).
A large variation in Bates-Jensen Score can have several possible reasons such as complexity of the wound, varied response to the NPWT therapy by patients, and type of wound. A reduction in Bates-Jensen Scores indicates an overall improvement in wound health such as lower wound exudate volume, reduced tissue necrosis, improved health of skin surrounding the wound, reduced peripheral tissue oedema, reduced peripheral tissue induration, increased tissue granulation and increased re-epithelialisation. It is important to highlight that chronic wounds with a duration >3 months and the BatesJensen scores >25 are more prone to develop polymicrobial infection by several bacterial species, such as Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis, and Klebsiella pneumonia.
Our analysis shows that out of 22 patients, 16 patients were shifted towards a BatesJensen score of <25 post-NPWT therapy, indicating a lower risk for microbial infection post-NPWT sessions. The improved wound health and lower risk for microbial infection may further improve wound healing outcomes and, therefore, reduce the risk for wound-associated adverse events such as amputation. During NPWT sessions, no patient reported adverse events such as allergy, skin macerations and skin inflammation. Overall, the device and wound dressing was found safe and biocompatible for wounds of various aetiologies. Taken together, the present clinical trial demonstrated that the NPWT device is a safe and effective therapeutic intervention for treating trauma and other complex wounds and can be employed for wound management and wound care.
Conclusion
The present study showed that the NPWT device (InoHeal System) is a promising therapeutic option to provide negative pressure wound therapy in trauma wounds. As assessed by the Bates-Jensen Wound Assessment Tool, the NPWT treatment improved wound healing by increasing tissue granulation and epithelialisation, lowering wound exudate volume and reducing necrotic tissue amount. In addition, improved wound healing after NPWT sessions can improve wound management and wound care by reducing pain and wound oedema, therefore, may have a positive impact on quality of life.
Conflicts of interest
The authors have no conflict of interest to declare.
Acknowledgement: We would like to thank All India Institute of Medical Sciences, New Delhi, India for providing the research facilities and technical assistance. We would also like to thank Inochi Care Private Limited, New Delhi, India for providing the wound healing system used in the present study.
References
1. Agarwal P, Kukrele R, Sharma D (2019) Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma 10(5):845–8. https://doi.org/10.1016%2Fj. jcot.2019.06.015
2. Bates-Jensen BM, McCreath HE, Harputlu D, Patlan A (2019) Reliability of the Bates-Jensen wound assessment tool for pressure injury assessment: The pressure ulcer detection study. Wound Repair Regen 27(4):386–95. https://doi.org/10.1111/wrr.12714
3. Dhivya S, Padma VV, Santhini E (2015) Wound dressings - a review. Biomedicine (Taipei) 5(4):22. https://doi. org/10.7603%2Fs40681-015-0022-9
4. Fortune Business Insights (2018) The global negative pressure wound therapy (NPWT) market size stood at USD 1.85 billion in 2018 and is projected to reach USD 2.74 billion by 2026, exhibiting a CAGR of 5.1% during the forecast period. https://tinyurl.com/5925x836 (accessed 29 September 2020)
5. Guan H, Dong W, Lu Y et al (2021) Distribution and antibiotic resistance patterns of pathogenic bacteria in patients with chronic cutaneous wounds in China. Front Med (Lausanne) 17(8):609584. https://doi. org/10.3389/fmed.2021.609584
6. Huang C, Leavitt T, Bayer LR et al (2014) Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 51(7):301–31. https://doi.org/10.1067/j. cpsurg.2014.04.001
7. Itani HE (2015) Reviewing the benefits and harm of NPWT in the management of closed surgical incisions. Br J Community Nurs 28(30):32-4. https://doi.org/10.12968/ bjcn.2015.20.sup6.s28
8. Knight R, Spoors LM, Costa ML et al (2019) Wound Healing in Surgery for Trauma (WHIST): statistical analysis plan for a randomized controlled trial comparing standard wound management with negative pressure wound therapy. Trials 20(1): 186. https://doi.org/10.1186/ s13063-019-3282-y
9. Leaper DJ (2006) Traumatic and surgical wounds. BMJ 332(7540):532–5. https://doi. org/10.1136%2Fbmj.332.7540.532
10. Meloni M, Izzo V, Vainieri E et al (2015) Management of negative pressure wound therapy in the treatment of diabetic foot ulcers. World J Orthop 6(4): 387–93. https://doi.org/10.5312%2Fwjo.v6.i4.387
11. Nussbaum SR, Carter MJ, Fife CE et al (2018). An economic evaluation of the impact, cost, and medicare policy implications of chronic nonhealing wounds. Value Health 21(1): 27–32. https://doi.org/10.1016/j. jval.2017.07.007
12. Pilehvar-Soltanahmadi Y, Dadashpour M, Mohajeri A et al (2018) An overview on application of natural substances incorporated with electrospun nanofibrous scaffolds to development of innovative wound dressings. Mini Rev Med Chem 18(5): 414–27. https://doi.org/10.2174/1389557517666170308112 147
13. Raj A, Benu GD, Kumar A et al (2020) Indigenous negative pressure wound treatment: Easy, effective and affordable. Int J Orthop Sci 6(1): 262–5. https://doi. org/10.22271/ortho.2020.v6.i1e.1870
14. Ramula M, Arivzhagan N (2020) VAC (Vacuum assisted closure) in the management of chronic non-healing wounds: Institutional study. Int J Surg Sci 4(4): 82–6. https://doi.org/10.33545/surgery.2020.v4.i4b.543
15. Sen CK (2019) Human wounds and its burden: An updated compendium of estimates. Adv Wound Care (New Rochelle) 8(2):39–48. https://doi.org/10.1089/ wound.2019.0946
16. Settipalli, S. [online] A robust market rich with opportunities: advanced wound dressings. https:// tinyurl.com/52szya3y (29.09.2020)
17. Zens Y, Barth M, Bucher HC et al (2020) Negative pressure wound therapy in patients with wounds healing by secondary intention: a systematic review and meta-analysis of randomized controlled trials. Syst Rev 9(238): 238. https://doi.org/10.1186/s13643-020-
This article is excerpted from the Wounds International 2023 | Vol 14 Issue 4 | ©Wounds International 2023 | www.woundsinternational.com by Wound World.