Pyoderma gangrenosum is a rare disease presenting as extremely painful and rapidly enlarging ulcers. It is one of a group of autoinflammatory disorders known as neutrophilic dermatoses (Skopis and Bag-Ozbek, 2021). There are no widely used or standardised guidelines regarding management and it is often based on prior experience and practices. Here we present the case of a 69-year-old female with an extremely painful multitreatment resistant pyoderma gangrenosum of the left shin, which clinically improved in both appearance and pain levels following maggot debridement and hyperbaric oxygen therapy. The improvements seen in this case may guide future management in similar recalcitrant cases of pyoderma gangrenosum.
CASE REPORT
A 69-year-old female was referred with a non-healing left medial malleolar wound, she also had peripheral venous disease. Her relevant medical history included autoimmune hepatitis, Sjögren’s syndrome, hypothyroidism, Parkinson’s disease, vocal cord palsy, vertigo and irritable bowel syndrome. Initially the wound was deemed vascular in nature, however, upon repeat review some months later an enlarging painful wound was noted and this, along with subsequent histopathological findings supported a diagnosis of pyoderma gangrenosum.
The standard initial treatment of systemic corticosteroid therapy was commenced (Skopis and Bag-Ozbek, 2021). High dose oral prednisolone, 0.5mg/kg daily for two weeks, was then escalated to 1mg/kg daily for six weeks resulting in a modest improvement in her pain levels. A switch to ciclosporin 5mg/kg daily was made as a steroid sparing agent, despite which, the pain continued. On review she had a 10kg unintentional weight loss in the preceding year and paraneoplastic investigations were undertaken. No malignancy was identified, however, following the development of a new face and neck rash, biopsies were performed. Histopathological findings of interface dermatitis supported a new diagnosis of cutaneous lupus. This is an autoimmune condition and has been reported, albeit rarely, to be associated with pyoderma gangrenosum (Skopis and Bag-Ozbek, 2021).
Based on this diagnosis hydroxychloroquine was started and after one year of only modest effect, it was discontinued. Other immunosuppressive agents were discussed. The patient was already on low dose azathioprine for management of autoimmune hepatitis, but she was noted to have neutropenia on higher doses. She also had a chronic normocytic anaemia. Therefore, dapsone, an antibiotic used for its anti-inflammatory effect, was deemed undesirable in this case, as haemolytic anaemia is a known potential side effect of this drug.
Throughout this time and despite immunosuppressive therapy, our patient’s main complaint was severe pain. The use of the pain visual analogue scale (VAS) revealed peak pain of 9/10 at this time. This was limiting her mobility and severely affecting her quality of life. Her ability to perform activities had been severely curtailed. Oral analgesia, including opioids, were insufficient and the provision of nerve blocks on two separate occasions provided significant but temporary relief. The use of compression therapy could not be tolerated due to the level of pain.
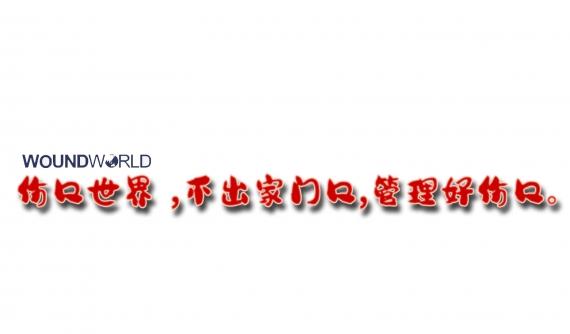
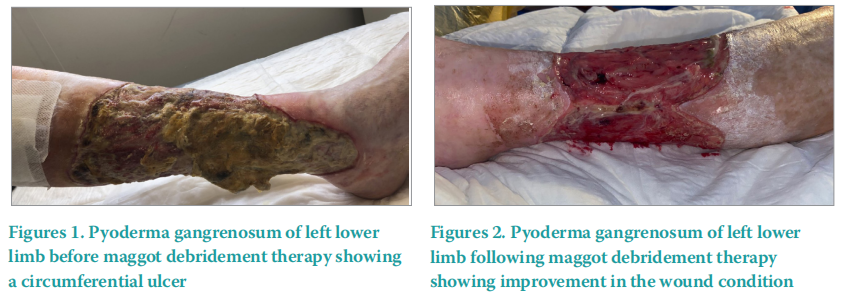
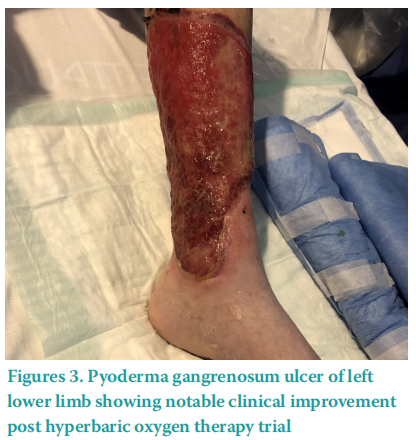
The ulceration had also deteriorated becoming circumferential (Figure 1) despite regular autolytic debridement. Novel treatments were therefore considered given the recalcitrance of disease, excruciating pain and comorbidities. A decision was made to first trial maggot debridement therapy followed by hyperbaric oxygen therapy (HBOT) to assist wound healing, pain reduction and to aid as an adjuvant to further immunosuppressive therapy. Maggot debridement therapy was applied over the course of two weeks. Following this trial our patient’s pain was noted to have reduced from 9/10 on VAS to 6/10, and removal of non-viable tissue was significant (Figure 2). Then, 20 sessions of HBOT were undertaken. Further reductions in pain levels were noted, with a decrease from 6/10 to 4/10 on VAS following HBOT. Wound healing was also observed (Figure 3). Our patient’s analgesia requirement reduced, and she began a physiotherapy rehabilitation programme. Ongoing immunosuppression was required and mycophenolate mofetil was introduced. Mycophenolate mofetil has been uptitrated to a therapeutic dose, with reductions in overall ulcer circumference.
Ongoing immunosuppression is essential to ensure the switching off of the immune process and treat the pyoderma gangrenosum .
DISCUSSION
Pyoderma gangrenosum is a rare condition encompassing a group of disorders known as neutrophilic dermatoses (Skopis and BagOzbek, 2021). The pathophysiology is not fully understood. It is currently considered an autoinflammatory condition with proposed involvement of the innate and adaptive immune systems with an underlying genetic predisposition (Skopis and Bag-Ozbek, 2021). Pyoderma gangrenosum presents as rapidly enlarging painful skin ulcers with classically a violaceous undermined border (Skopis and Bag-Ozbek, 2021). Subtypes include classic, pustular, peristomal, bullous and granulomatous (Ashchyant al et, 2019). Diagnosis can be difficult and is based on careful history, clinical presentation, histopathological findings and exclusion of other causes of cutaneous ulceration (Alonso‐León et al, 2020). Pathergy is demonstrated in approximately 30 to 50% of cases (Ashchyan et al, 2019). Pyoderma gangrenosum lesions can commonly occur in people with underlying systemic illness such as inflammatory bowel disease (up to 30%), haematological malignancies and rheumatoid arthritis (Skopis and Bag-Ozbek, 2021). Pyoderma gangrenosum also has more rare associations with a number of autoimmune conditions including systemic lupus erythematosus and autoimmune hepatitis as in our patient, however the mechanisms between this link remain unclear (González-Moreno et al, 2014).
The treatment of pyoderma gangrenosum can be challenging. There are no standardised guidelines, furthermore, management is largely based on case reports and case series. The main goal is immunosuppression leading to wound healing, noting that comorbidities such as diabetes or peripheral vascular disease may prolong and adversely affect healing (Skopis and Bag-Ozbek, 2021).
Wound care is an important aspect of pyoderma gangrenosum management and debridement of non-viable tissue may be required. Debridement strategies in chronic wound care are well established and are most commonly surgical, autolytic, osmotic or maggot debridement therapy types. In maggot debridement therapy, the larvae are held within a mesh dressing and applied directly to the wound allowing them to debride the non-viable tissue only Ratcliffe et al, 2014). This is selective debridement as healthy tissue is not affected and is based on three therapeutic actions; debridement, disinfection and skin growth promotion. To our knowledge, following a literature review, only one study reports the positive use of maggot debridement therapy in recalcitrant pyoderma gangrenosum (Din et al, 2018).
HBOT is a process of supplying tissue with oxygen to promote healing. Wounds, such as in pyoderma gangrenosum, are starved of oxygen and therefore healing is diminished (Katz et al, 2021). HBOT results in tissue hyperoxia leading to angiogenesis and reduction in inflammation and pain (Katz et al 2021). The physician-prescribed process involves the patient entering a special chamber to breathe in pure oxygen at higher than average air pressure levels (Katz et al, 2021). The patient sits or lies within the chamber for a predetermined length of time, such as 45 minutes, as in the case of our patient. Repeated sessions are required and typically involve a number of sessions per week. As in this case, objective measures are used for monitoring improvement, including clinical photography and the use of pain scales such as VAS. HBOT is typically used for nonhealing wounds associated with conditions such as vascular insufficiency and diabetes and in the case of compromised skin grafts or flaps (Katz et al 2021). The positive effects of HBOT in refractory pyoderma gangrenosum have been described (Katz et al, 2021; de Sousa Magalhães et al, 2021; Maronese et al, 2022).
CONCLUSION
Our case highlights how significant improvements in wound healing and pain reduction can be achieved by considering non-traditional treatment approaches in patients with refractory pyoderma gangrenosum. Immunosuppressive therapy is ongoing to ensure ulcer healing and clearance. Nonetheless, this report shows that maggot debridement therapy and HBOT may be considered in similar cases in the future.
DECLARATION OF INTEREST
No conflicts of interest to declare. No competing interests or funding to declare. The data that support the findings of this study are available from the corresponding author, DL, upon reasonable request.
REFERENCES
1. Alonso‐León T, Hernández‐Ramírez H, Fonte‐Avalos V et al (2020)The great imitator with no diagnostic test: pyoderma gangrenosum. Int Wound J 17(6):1774–82. https://doi.org/10.1111%2Fiwj.13466
2. Ashchyan H, Butler D, Nelson C et al (2018) The association of age with clinical presentation and comorbidities of pyoderma gangrenosum. JAMA Dermatol 154(4):409. https://doi.org/10.1001/jamadermatol.2017.5978
3. de Sousa Magalhães R, Moreira MJ, Rosa B, Cotter J (2021) Hyperbaric oxygen therapy for refractory pyoderma gangrenosum: a salvage treatment. BMJ Case Rep 14:e238638. https://doi.org/10.1136/bcr- 2020-238638
4. Din R, Tsiaras W, Mostaghimi A (2018) Two cases of maggot debridement therapy in pyoderma gangrenosum. JAAD Case Rep 4(10):1027–9. https://doi.org/10.1016%2Fj.jdcr.2018.07.016
5. González-Moreno J, Ruíz-Ruigomez M, Callejas Rubio J et al (2014) Pyoderma gangrenosum and systemic lupus erythematosus: a report of five cases and review of the literature. Lupus 24(2):130–7. https://doi. org/10.1177/0961203314550227
6. Katz AA, Thomson K, Amin U (2021) Hyperbaric oxygen therapy as an adjunctive treatment for pyoderma gangrenosum: a case report. Intl J Res Dermatol 27;7(6):863
7. Maronese CA, Pimentel MA, Li MM et al (2022) Pyoderma gangrenosum: an updated literature review on established and emerging pharmacological treatments. Am J Clin Dermatol 23(5):615–34. https://doi.org/10.1007/s40257-022-00699-8
8. Ratcliffe N, Azambuja P, Mello CB (2014) Recent advances in developing insect natural products as potential modern day medicines. Evid Based Complement Alternat Med 2014:904958. https://doi. org/10.1155/2014/904958
9. Skopis M, Ayse Bag-Ozbek A (2021) Pyoderma gangrenosum: a review of updates in diagnosis, pathophysiology and management J 4(3):367–5. https://doi.org/10.3390/j4030028
This article is excerpted from the Wounds UK | Vol 19 | No 4 | 2023 by Wound World.