1. Introduction
As people’s lifestyles evolve and population aging accelerates, the prevalence of type 2 diabetes mellitus (T2DM) and obesity is on a rapid incline. The initial Diabetes Map of China, released by the Chinese Center for Disease Control and Prevention in 2022, indicates that the overall prevalence of T2DM in China surged to 14.92% between 2015 and 2019, ranking it first globally. This is in stark contrast to the 1.29% recorded from 1980 to 1984 [1]. Obesity is intricately linked with T2DM. The 2023 Obesity Map of China reveals a 36.8% prevalence of diabetes among obese/overweight individuals in China [2], with 58% of diabetes patients being overweight or obese [3]. Therefore, obesity emerges as the primary cause of T2DM.
Traditionally considered an incurable chronic progressive disease, T2DM’s best-expected outcome through conventional hypoglycemic therapy has been to manage hyperglycemia and delay inevitable complications. Unfortunately, the compliance rate for diabetes control has been historically low, leading to a worsening public health situation related to diabetes. Recent years have witnessed a shift in the traditional “hypoglycemiccentered” approach to T2DM treatment, with a growing recognition of the “patient-centered” integrated management concept. Simultaneously, the previously considered irreversible cognitive pattern of T2DM is transforming [4].
Mounting evidence suggests that diabetes can be reversed. Numerous studies confirm that managing body weight through lifestyle intervention, certain drug treatments, and metabolic weight loss surgery can enhance insulin sensitivity, improve insulin secretion, foster B cell redifferentiation, and repair and reverse pancreatic function, thereby delaying or even reversing diabetes progression. In 2016, the World Health Organization (WHO) acknowledged that diabetes could be reversed through weight loss and calorie restriction. Most experts posit that, in the absence of hypoglycemic drugs, maintaining blood glucose levels lower than diabetes diagnostic criteria for an extended period and glycosylated hemoglobin (HbA1c) below 6.5% fulfill the requirements for diabetes remission [5,6]. The concept of “reversal of diabetes” aims to prevent the progression of diabetes into a destructive cycle, repair or even reverse islet β cell function, delay or prevent disease progression, reduce or cease the use of diabetes drugs, enhance patient’s quality of life, alleviate the medical burden on patients and society, and reverse the severe health crisis of diabetes.
Over the past decade, more than one hundred experts from the Specialized Committee of Obesity Reversal of the Guangdong Provincial Geriatric Health Association and the Specialized Committee of Diabetes Management of the Guangdong Provincial Hospital Association have affirmed that T2DM patients with obesity can undergo reversal through extensive clinical practices. This draft refined through multiple revisions after extensive discussions and then consensus-seeking while acknowledging differences, serves as a clinical pathway guide for reversal therapy. It integrates the latest theories and clinical practices related to diabetes globally, offering valuable insights to domestic counterparts.
2. Significance and purpose of reversing T2DM combined with obesity
Diabetes can lead to chronic complications such as vasculopathy and neuropathy, as well as acute complications such as infection and ketoacidosis, necessitating lifelong medication treatment for patients. According to the 2017 National Medical Insurance Sampling Database, Chinese diabetic patients incur an average annual personal expenditure of 18,785 CNY (including inpatients), while the corresponding annual personal expenditure covered by medical insurance is 41,682 CNY [1]. This imposes a substantial economic burden on patients, their families, and society.
Increased body weight or waist circumference can exacerbate insulin resistance, complicating blood glucose control [7,8]. Weight loss proves effective in improving insulin resistance, managing blood glucose, reducing cardiovascular and cerebrovascular disease risk factors, and enhancing overall quality of life. Within a certain range, greater weight loss correlates with more significant health benefits [9]. Obesity heightens the risk of chronic complications in T2DM patients independently. It serves as a key risk factor for diabetic kidney disease, contributing to the progression of chronic kidney disease. Moreover, weight loss proves advantageous in reducing proteinuria in chronic kidney disease patients and slowing down the decline in renal function [10,11]. Obesity also substantially elevates the risk of cardiovascular and cerebrovascular diseases [12]. Therefore, reinforcing weight management in T2DM patients with obesity while concurrently addressing blood glucose is of paramount importance.
In 2016, the Endocrinology Branch of the Chinese Medical Association established An Expert Consensus on the Comprehensive Management of T2DM Complicated with Obesity in China [13]. In 2021, Professor Zou Dajin and Professor Ji Linong collaboratively formulated China’s inaugural Chinese Expert Consensus on Alleviating T2DM. In 2022, Professor Wu Yiming and a team of 13 experts nationwide issued the Expert Consensus on Weight Management of Patients with T2DM in China [14], guiding the systematic management of T2DM patients complicated with obesity. The economic and social value of reversing diabetes and obesity is substantial as it reduces medication dependency, alleviates complications, and diminishes personal, family, and socio-economic burdens.
The purpose of formulating a reversal therapy clinical expert consensus on T2DM complicated with obesity is to further standardize clinical management processes, improve blood glucose compliance rates and diabetes-related weight control, reduce the risk of complications, enhance patients’ overall quality of life, and alleviate personal and social economic burdens.
3. Diagnostic criteria for T2DM complicated with obesity
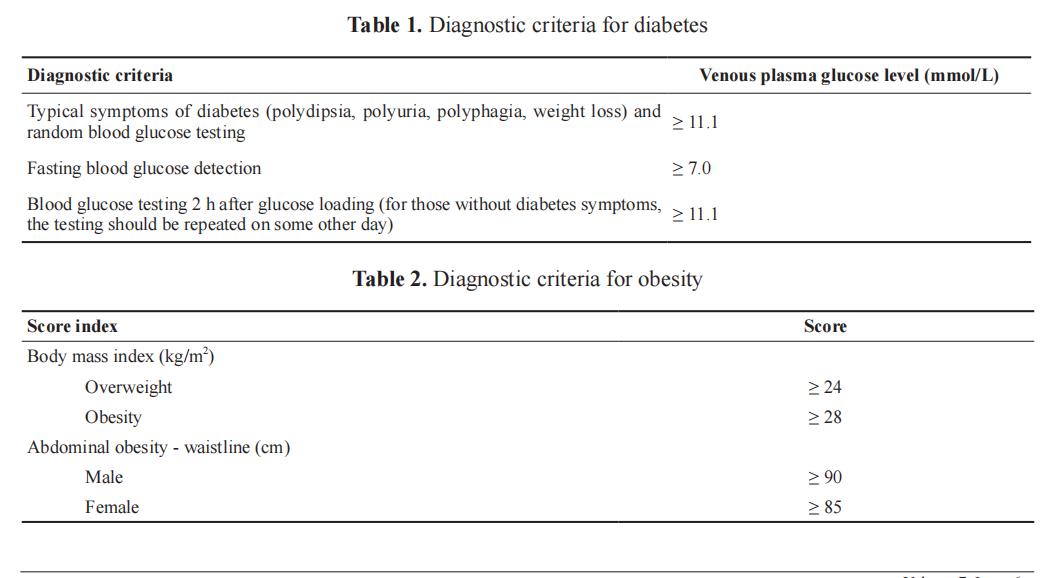
The diagnostic criteria and classification of T2DM adhere to the standards set by the WHO in 1999 [15]. The diagnostic criteria for obesity are derived from the Expert Consensus on Chinese Adult Obesity Prevention (2011 Edition) [16], and the criteria for abdominal obesity outlined in the Chinese Type 2 Diabetes Prevention Guide (2020 Edition) [17]. Patients meeting the diagnostic criteria for both conditions are managed in accordance with T2DM complicated with obesity. Tables 1 and 2 present the diagnostic criteria for diabetes and obesity, respectively
4. Definition of diabetes reversal
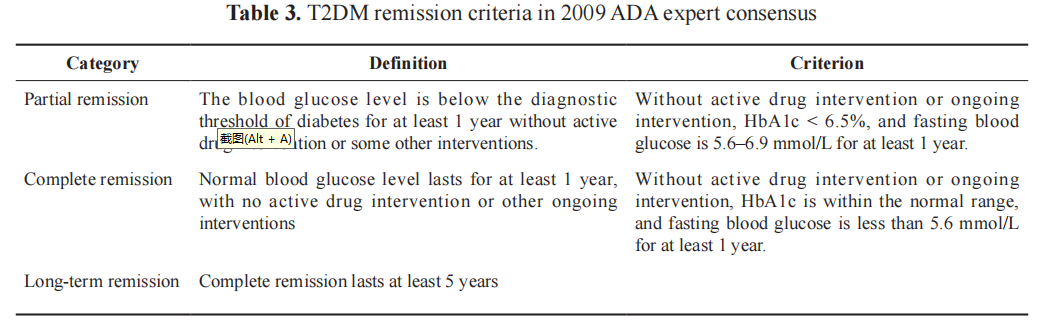
Presently, there exists no uniform standard for the definition of T2DM reversal. In 2017, the DiRECT study delineated diabetes remission as the withdrawal of anti-diabetic drugs for a minimum of 2 months and an HbA1c level below 6.5% at the one-year mark [18]. In 2009, the definition of T2DM remission within the pertinent consensus of the American Diabetes Association (ADA) categorized it into partial remission, complete remission, and long-term remission (Table 3). The 2021 Consensus Report titled “Definitions and Explanations for T2DM Remission,” drafted by the International Expert Group of the ADA, proposed the use of an HbA1c level below 6.5% after at least 3 months of discontinuation of hypoglycemic drugs as a diagnostic criterion for T2DM remission.
In China, the domestic standard for T2DM remission has incorporated the postprandial blood glucose level index, and the requirement for HbA1c levels is relatively lenient. Professor Li Guangwei and Professor Weng Jianping applied the same criteria to assess the remission of T2DM patients undergoing intensive insulin therapy [19]: in the absence of medication after intensive treatment, fasting blood glucose should be below 7.0mmol/L, and blood glucose two hours post-meal should be below 10 mmol/L, with this state maintained for over a year.
5. Mechanisms of diabetes reversal
Insulin resistance and islet β-cell dysfunction represent the primary pathophysiological characteristics of T2DM complicated with obesity. In skeletal muscle, lipid accumulation diminishes blood glucose utilization, concurrently escalating insulin secretion. The heightened insulin concentration in the portal vein triggers liver fat deposition, further exacerbating liver insulin resistance. Additionally, synthesized fat infiltrates pancreatic tissue, resulting in impaired pancreatic β-cell function, β-cell dedifferentiation, and a subsequent decline in insulin response to ingested glucose, thereby elevating postprandial blood glucose levels. Notably, insulin resistance impacting blood glucose control predominantly originates from the liver rather than skeletal muscle [20].
Recent studies challenge the notion that β cells in T2DM patients undergo apoptosis; instead, they lose key β-cell characteristics due to dedifferentiation. Consequently, these cells lose their normal secretory regulation function, rendering them incapable of metabolic regulation in glucose homeostasis [21].
Research indicates that lifestyle intervention and comprehensive treatments, such as hypoglycemic drug application and nutritional adjustment, stand out as primary effective measures for diabetes reversal. Lifestyle intervention not only delays the onset of T2DM but also diminishes the risk of cardiovascular and cerebrovascular adverse events, microvascular complications, and cardiovascular and all-cause mortality, thereby prolonging life expectancy [22-24]. Short-term intensive insulin therapy in the early stages of diabetes alleviates the condition and contributes to the recovery of β-cell functions [25]. GLP-1 receptor agonists (GLP- 1RAs), through multiple mechanisms, reduce insulin resistance and play a role in diabetes reversal [26]. Precise nutritional therapy, meanwhile, contributes to weight reduction and the partial restoration of insulin function [27].
6. Reversal methods and processes
6.1. Reversal mode
(1) 2+N reversal mode: “2” signifies the integration of traditional Chinese medicine and Western medicine, as well as the fusion of drug and non-drug approaches. “N” encompasses a range of comprehensive measures, including precise nutritional therapy, scientific exercise, correction of detrimental lifestyle habits, and mental conditioning.
(2) In-hospital treatment: Recommended for new-onset diabetes, patients experiencing unstable blood glucose fluctuations (fasting blood glucose > 10mmol/L, random blood glucose > 15 mmol/L), and those with severe complications.
(3) Out-of-hospital comprehensive management: Appropriate for patients with stable conditions post short-term hospitalization, individuals whose severe complications are under control, and those whose blood glucose levels meet the standard.
6.2. Reversal process – main operational steps of clinical management standard
6.2.1. Establishment and personnel allocation of multidisciplinary diagnosis and treatment team
The comprehensive management of T2DM patients with obesity/overweight necessitates a multidisciplinary diagnosis and treatment team. The team’s formation involves professionals and the acquisition of necessary hardware equipment. Led by diabetes specialists, the multidisciplinary team includes nutritionists, health managers, psychologists, weight loss surgeons, sports medicine doctors, rehabilitation physiotherapists, diabetes specialist nurses, and network managers. Hardware equipment comprises common medical tools such as a glucometer, instantaneous continuous blood glucose monitoring system, sphygmomanometer, computer, height and weight instrument, tape, nylon wire, tuning fork, human body fat composition analyzer, non-mydriatic ophthalmoscope, Doppler stethoscope, and peripheral nerve sensory threshold detector.
The medical staff at primary medical institutions, outpatient departments of hospitals at all levels, physical examination centers, weight loss centers, nutrition departments, and health care institutions should be trained to conduct diabetes screening, focusing on families with a history of diabetes.
Endocrine doctors with specialized reversal training formulate a reversal plan, oversee the entire reversal process, and guide health management institutions, nutritionists, rehabilitation physiotherapists, health managers, psychologists, and sports fitness coaches, all of whom have received professional reversal training, to jointly supervise patients in completing the reversal work.
6.2.2. Screening of high-risk population
Screening for adults (> 18 years old) with high-risk diabetes complicated with obesity includes measuring body mass index and waist circumference, blood glucose screening, glucose tolerance testing, differential diagnosis of etiology, understanding of diabetes and obesity-related complications, and testing and inquiring about related medical history.
6.2.3. Confirmation of patients
Diagnosis of T2DM patients complicated with obesity/overweight adheres to the diagnostic criteria of both T2DM and obesity/overweight. The diagnosis of abdominal obesity primarily utilizes waist circumference, with diagnostic criteria of male ≥ 90 cm and female ≥ 85 cm.
6.2.4. Improvement of auxiliary examination and establishment of files for reversed patients
The perfect auxiliary examination involves filing and measuring height, weight, waist circumference, hip circumference, body fat content, and body mass index, as well as taking photos. Biochemical tests include blood lipids, blood glucose, HbA1c, insulin and C-peptide levels, urinary microalbumin, thyroid function, adrenocortical hormone, and sex hormones. Peripheral nerve electrophysiological examination, fundus examination, electrocardiogram, abdominal ultrasound, chest X-ray, and body fat composition analysis should be performed.
Filing involves the collection of patients’ basic information, evaluation of islet β-cell function and complications, and establishment of personal medical records through hospitals, community health service centers, or health management institutions.
6.2.5. Evaluation and grading of patients
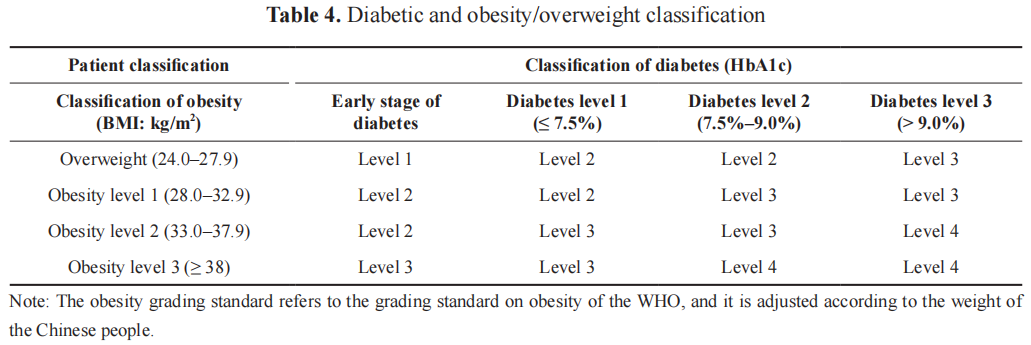
Assessment and grading include disease assessment, lifestyle assessment, and psychological assessment. Disease assessment can be summarized as ABCD, where A represents Age and HbA1c; B represents BMI and blood pressure; C represents Cholesterol and Cigarettes; D represents Diet and Duration. Patient condition is divided into 4 grades based on weight and blood glucose control level (see Table 4), where a higher grade indicates a more severe disease.
Lifestyle assessment encompasses various aspects such as diet, exercise habits, exercise willingness, exercise feasibility, and smoking and drinking habits. Sports feasibility includes physical function feasibility and environmental feasibility. Psychologists should also evaluate patients based on quality of life, sleep status, and anxiety status.
6.2.6. Formulation of intervention schemes
An individualized reversal intervention plan should be formulated based on the evaluation of the patient’s condition. The plan sets control objectives such as ideal weight, blood glucose, and complications. Lifestyle, drug intervention, and bariatric surgery schemes are then developed. Diabetes reversal treatment sets goals according to different stages of the disease (see Table 5).
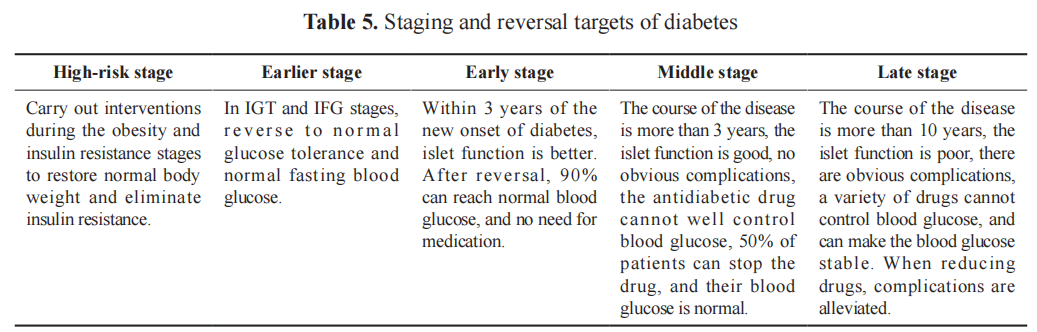
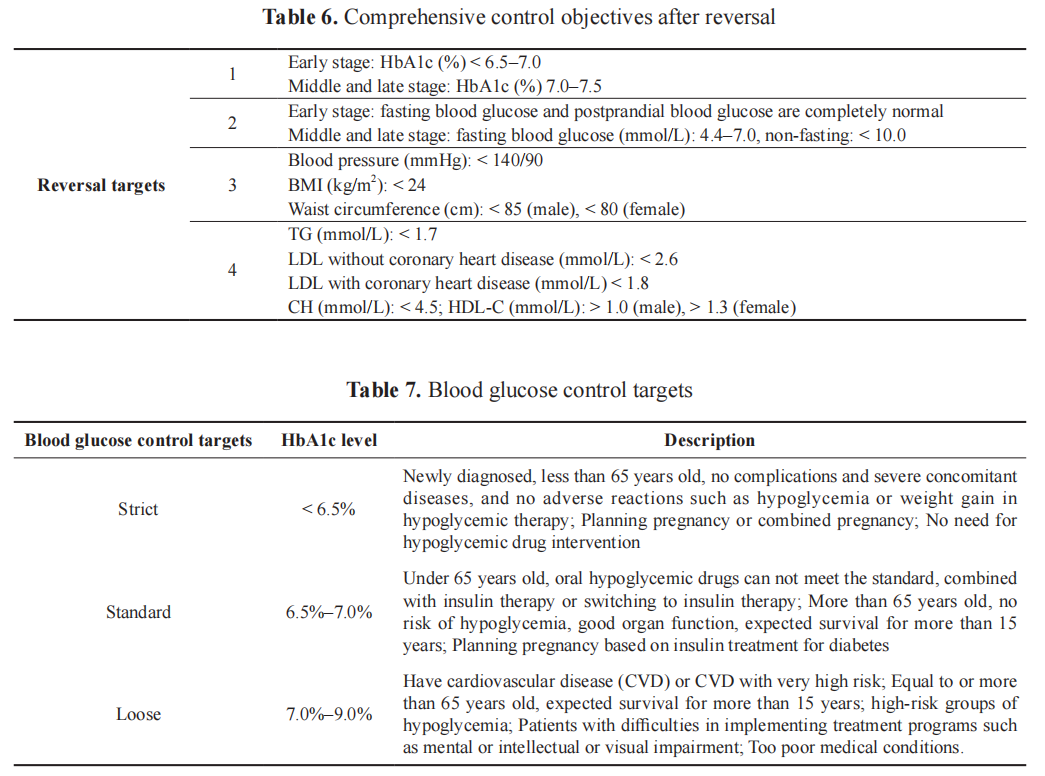
The ideal control targets for blood glucose, blood pressure, and blood lipid should be determined according to different stages. In the middle and late stages of diabetes, blood glucose control is relatively loose (refer to Tables 6 and 7 for specific control targets).
6.2.7 Implementation of intervention measures
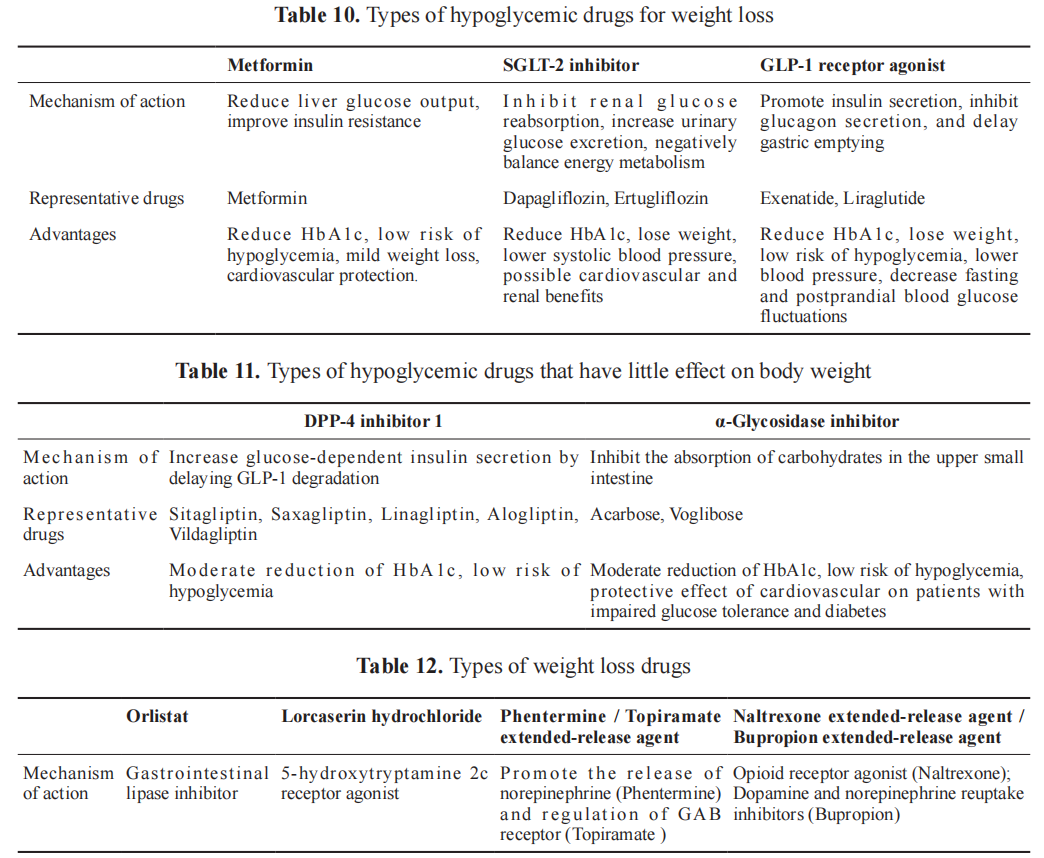
When implementing intervention treatment schemes for diabetic patients, individualized choices are made according to different conditions. Drug intervention scheme choices consider improving insulin resistance and protecting β-cell function, prioritizing drugs with comprehensive metabolic benefits. Hypoglycemic drugs with significant weight loss effects are preferred, followed by those with minimal impact on body weight. Drugs that increase body weight should be used sparingly, with weight loss drugs and surgery considered if necessary.
Several key intervention treatment issues:
(1) Lifestyle intervention: Lifestyle intervention, a pivotal part of the reversal process, includes dietary adjustments, exercise routines, habit corrections, and psychological therapy. Successful intervention requires collaborative efforts from Western medicine practitioners, Chinese medicine practitioners, and healthcare managers. The integration of Internet+ is instrumental in achieving optimal results. The 5+2 reversal treatment model, combining the traditional “five carriages” with co-management and Internet+, proves effective where traditional methods fall short.
(2) Weight management: Effective weight management is crucial for diabetic patients with obesity. Early weight loss goals range from 5% to 10%, with the ultimate target being a BMI < 24 kg/m2 .
(3) Precise nutrition: A scientifically sound diet forms the foundation of diabetes reversal therapies. Patients with T2DM and obesity require precise, personalized, and systematic nutrition therapy. The selection of nutritional interventions should align with metabolic indicators such as obesity degree, blood glucose, blood pressure, blood lipid, and uric acid. Recommended dietary modes include the ketogenic diet, low-carbohydrate diet, Mediterranean diet, and Paleo diet, flexibly adapted to the patient’s condition. Diet therapy principles include:
(a) Determine total calorie intake based on body mass index and weight loss goals;
(b) Adjust the proportion of carbohydrate intake according to blood glucose control, choose foods with a low glycemic index (GI) and/or low glycemic load (GL) such as coarse grains and vegetables, and avoid the intake of refined rice and flour foods and refined sugars;
(c) Appropriately adjust the total amount of protein intake and avoid a long-term high-protein diet;
(d) Avoid the intake of trans-fatty acids, and appropriately intake high-quality fat;
(e) Increase dietary fiber intake;
(f) Appropriately select types and quantities of fruits according to the control of blood glucose;
(g) Ensure the intake of rich vitamins, minerals, and antioxidants;
(h) Reasonably allocate dieting time to reduce the stimulation of the pancreas;
(i) Chewing slowly is conducive to digesting food;
(j) Pay attention to intestinal health and appropriately supplement probiotics and/or prebiotics.
(4) Scientific exercise therapy: Exercise enhances insulin sensitivity, improves skeletal muscle function,
and positively impacts metabolic disorders. Principles of exercise therapy for T2DM with obesity
include:
(a) Medical evaluation before exercise therapy and strict control of indications and contraindications;
(b) Individualized exercise prescriptions according to the patient’s course of disease, degree of illness, severity of complications, etc., by considering a variety of factors such as age, family status, exercise habits, and cultural background; the exercise prescription should include five elements: exercise frequency, exercise intensity, exercise duration, exercise type, and amount of exercise;
(c) Focusing on moderate intensity and aerobic exercises, at least 3 times a week, not less than 20 minutes each time. Aerobic exercise and resistance exercise should be carried out alternately, integrating outdoor and indoor activities. They should exercise at any time and anywhere according to their specific living and working environment. Meanwhile, they should integrate the concept of exercise into life and work, persist in a personalized, continuous, and systematic exercise mode, and walk at least 5,000–10,000 steps every day (depending on the patient’s physical condition);
(d) They should follow the principles of from light to heavy, from less to more, from slow to fast, and from sparse to dense to adjust their own sports scheme;
(e) They should adjust the exercise scheme in time according to blood glucose monitoring and weight loss.
(5) Mental intervention: Obesity and diabetes increase the psychological burden on patients. Strengthening psychological intervention, guided by professional psychologists or diabetes specialists, helps patients adjust their mentality, improve their life attitude, and boost their confidence. Weight loss not only overcomes psychological barriers but also fosters self-confidence, contributing to enhanced life
(6) Developing good living habits: A poor lifestyle is a significant factor leading to diabetes and obesity. A good lifestyle is essential for reversing diabetes complicated with obesity. Doctors play a crucial role in helping patients identify existing problems, providing corrective training, and ensuring patients form and maintain good living habits.
(7) Chinese medicine acupuncture and rehabilitation therapy: Traditional Chinese medicine offers advantages in regulating metabolic disorders caused by diabetes and treating diabetic complications. “Obesity or overweight - spleen-warm syndrome - Xiaoke - Xiaoke complications” is the natural development process of obese diabetes. The effect of the “Kaiyu Qingre method” is significant in the treatment of early and middle diabetes [28]. Compound preparations such as Dahuang Huanglian Xiexin Decoction, Gegen Qinlian Decoction, and Dachaihu Decoction can appropriately reduce blood glucose and reduce risk factors for complications [29]. Therefore, Chinese medicine conditioning, tailored to blood glucose, constitution, and Chinese medicine dialectical methods, significantly improves physical condition, stabilizes blood glucose, and enhances the reversal effect of diabetes.
By stimulating the corresponding acupoints, acupuncture plays a role in dredging the channel, balancing yin and yang, regulating Zang and Fu, and running qi and blood, and ultimately achieves the purpose of weight loss and blood glucose regulation [30]. Acupuncture can also inhibit the occurrence of hunger and reduce food intake by adjusting the activity of neurotransmitters. Meanwhile, it can promote the adrenal medulla to secrete adrenaline, enhance fat mobilization and decomposition, and reduce the content of growth hormone and insulin, thereby reducing weight, lowering blood glucose, and reversing diabetes.
Major acupoints of acupuncture therapy included Yishu, Pishu, and Sanyinjiao. Matching acupoints for patients with damp-heat retention in the spleen may include Quchi and Neiting. Functional acupuncture, moxibustion, and ultrasonic energy meter can dredge the channel, relieve diabetic complications, and activate stem cells to repair islet function [31-33]. Therefore, it has a very important adjuvant therapeutic effect on the reversal of T2DM patients complicated with obesity.
(8) Rational use of drug therapy: In the early stage of diabetes reversal, drugs should be applied rationally based on blood glucose and complications. Tables 10 to 12 show the characteristics and types of related drugs. However, in the late reversal, medication should be minimized to prevent hypoglycemia.
(9) Surgical treatment: Metabolic surgery can be considered for T2DM patients with obesity/overweight if blood glucose control or weight loss is unsatisfactory after comprehensive reversal therapy. Surgical methods and types are individually selected based on the patient’s condition and willingness, following corresponding guidelines.
(10) Control of multiple risk factors: Assessment of risk factors for cardio-cerebro-renal vascular disease (such as carotid ultrasound, peripheral nerve sensory threshold, fundus, urinary microprotein, liver and kidney function) should be conducted annually. Treatment plans should be adjusted based on examination results.
(11) Monitoring and follow-up:
(a) Monitoring: FPG and PG 2 hours after the meal should be detected at each follow-up, and HbA1C, blood lipids, body weight, and other risk factors of cardiovascular, cerebrovascular, and renal vascular diseases should be monitored regularly. OGTT and islet function tests should be performed at least once a year.
(b) Follow-up: Face-to-face or telephone follow-up should be carried out at least once a week to understand the patient’s diet and exercise situation, complications, blood glucose control, symptom improvement, etc. The physical examination should be recorded to conduct a dynamic comparison and formulate a diagnosis and treatment plan.
(c) Efficacy evaluation after reversal: 3–6 months after reversal, the blood glucose stability of patients should be evaluated. All indicators before reversal should be re-examined to compare the differences before and after treatment and evaluate the therapeutic effect. Meanwhile, patient satisfaction, medical expenses, and medical insurance payments should be evaluated.
Disclosure statement
The authors declare no conflict of interest.
References
[1] Wu J, Guo L, 2022, The Map of Diabetes in China. People’s Health Publishing House, Beijing.
[2] Chen K, Shen Z, Gu W, et al., 2023, Prevalence of Obesity and Associated Complications in China: A Cross-Sectional, Real-World Study in 15.8 Million Adults. Diabetes Obes Metab, 25(11): 3390–3399. https://doi.org/10.1111/dom.15238.
[3] Wang Y, Liang X, Zhou Z, et al., 2022, Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study. Int J Environ Res Public Health, 19(5): 2989. https://doi.org/10.3390/ijerph19052989
[4] McCombie L, Leslie W, Taylor R, et al., 2017, Beating Type 2 Diabetes into Remission. BMJ, 358: j4030. https://doi. org/10.1136/bmj.j4030
[5] Ramos-Levi AM, Cabrerizo L, Matia P, et al., 2013, Which Criteria Should be Used to Define Type 2 Diabetes Remission After Bariatric Surgery? BMC Surg, 13: 8. https://doi.org/10.1186/1471-2482-13-8
[6] Klein S, Sheard NF, Pi-Sunyer X, et al., 2004, Weight Management Through Lifestyle Modification for the Prevention and Management of Type 2 Diabetes: Rationale and Strategies. A Statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Am J Clin Nutr, 80(2): 257–263. https://doi.org/10.1093/ajcn/80.2.257
[7] The Diabetes Prevention Program Research Group, 2006, Relationship of Body Size and Shape to the Development of Diabetes in the Diabetes Prevention Program. Obesity (Silver Spring), 14(11): 2107–2117. https://doi.org/10.1038/ oby.2006.246
[8] Lake S, Krook A, Zierath JR, 2003, Analysis of Insulin Signaling Pathways Through Comparative Genomics. Mapping Mechanisms for Insulin Resistance in Type 2 (Non-Insulin-Dependent) Diabetes Mellitus. Exp Clin Endocrinol Diabetes, 111(4): 191–197. https://doi.org/10.1055/s-2003-40462
[9] Jensen MD, Ryan DH, Apovian CM, et al., 2014, 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation, 129(25 Suppl 2): S102–138. https://doi. org/10.1161/01.cir.0000437739.71477.ee
[10] Lastra G, Manrique C, Sowers JR, 2006, Obesity, Cardiometabolic Syndrome, and Chronic Kidney Disease: The Weight of the Evidence. Adv Chronic Kidney Dis, 13(4): 365–373. https://doi.org/10.1053/j,ackd,2006.07.011
[11] Navaneethan SD, Yehnert H, Moustarah F, et al., 2009, Weight Loss Interventions in Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Clin J Am Soc Nephrol, 4(10): 1565–1574. https://doi.org/10.2215/CJN.02250409
[12] Indulekha K, Anjana RM, Surendar J, et al., 2011, Association of Visceral and Subcutaneous Fat with Glucose Intolerance, Insulin Resistance, Adipocytokines and Inflammatory Markers in Asian Indians (CURES-113). Clin Biochem, 44(4): 281–287. https://doi.org/10.1016/j.clinbiochem.2010.12.015
[13] Endocrinology Branch of the Chinese Medical Association, 2016, Expert Consensus on Integrating Obesity Management with T2DM in China. Chinese Journal of Diabetes, 8(11): 662–666.
[14] Ji Q, Wu Y, et al., 2022, Expert Consensus on Weight Management for Patients with Type 2 Diabetes. International Journal of Endocrinology and Metabolism, 9: 78–86.
[15] Alberti KG, Zimmet PZ, 1998, Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus Provisional Report of a WHO Consultation. Diabet Med, 15(7): 539–553. https://doi.org/10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
[16] Obesity Group, Endocrinology Branch, Chinese Medical Association, 2011, Consensus of Experts on the Prevention and Treatment of Adult Obesity in China. Chinese Journal of Endocrinology and Metabolism, 27(9): 711–717.
[17] Chinese Diabetes Society, 2021, Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes (2020 Edition). Chinese Journal of Diabetes, 13(4): 317–411.
[18] Knowler WC, Barrett-Connor E, Fowler SE, et al., 2002, Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N Engl J Med, 346(6): 393–403. https://doi.org/10.1056/NEJMoa012512
[19] Weng J, 2017, Short‐Term Intensive Insulin Therapy Could be the Preferred Option for New Onset Type 2 Diabetes Mellitus Patients with HbA1c > 9. J Diabetes, 9(10): 890–893. https://doi.org/10.1111/1753-0407.12581
[20] Al-Mrabeh A, Zhyzhneuskaya SV, Peters C, et al., 2020, Hepatic Lipoprotein Export and Remission of Human Type 2 Diabetes after Weight Loss. Cell Metab, 31(2): 233–249.e4. https://doi.org/10.1016/j.cmet.2019.11.018
[21] Accili D, Talchai SC, Kim-Muller JY, et al., 2016, When β-cells Fail: Lessons from Dedifferentiation. Diabetes Obes Metab, 18 Suppl 1(S1): 117–122. https://doi.org/10.1111/dom.12723
[22] Li G, Zhang P, Wang J, et al., 2008, The Long-Term Effect of Lifestyle Interventions to Prevent Diabetes in the China Da Qing Diabetes Prevention Study: A 20-Year Follow-Up Study. Lancet, 371(9626): 1783–1789. https://doi. org/10.1016/S0140-6737(08)60766-7
[23] Gong Q, Gregg EW, Wang J, et al., 2011, Long-Term Effects of a Randomised Trial of a 6-Year Lifestyle Intervention in Impaired Glucose Tolerance on Diabetes-Related Microvascular Complications: The China Da Qing Diabetes Prevention Outcome Study. Diabetologia, 54(2): 300–307.
[24] Li G, Zhang P, Wang J, et al., 2014, Cardiovascular Mortality, All-Cause Mortality, and Diabetes Incidence After Lifestyle Intervention for People with Impaired Glucose Tolerance in the Da Qing Diabetes Prevention Study: A 23-Year Follow-Up Study. Lancet Diabetes Endocrinol, 2(6): 474–480. https://doi.org/10.1016/S2213-8587(14)70057-9
[25] Kramer CK, Zinman B, Retnakaran R, 2013, Short-Term Intensive Insulin Therapy in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis.Lancet Diabetes Endocrinol, 1(1): 28–34. https://doi.org/10.1016/S2213- 8587(13)70006-8
[26] Nadkarni P, Chepurny OG, Holz GG, 2014, Regulation of Glucose Homeostasis by GLP-1. Prog Mol Biol Transl Sci, 121: 23–65. https://doi.org/10.1016/B978-0-12-800101-1.00002-8
[27] Bauman WA, Schwartz E, Rose HG, et al., 1988, Early and Long-Term Effects of Acute Caloric Deprivation in Obese Diabetic Subjects. Am J Med, 85(1): 38–46. https://doi.org/10.1016/0002-9343(88)90500-1
[28] Guo J, Chen H, Song J, et al., 2014, Syndrome Differentiation of Diabetes by the Traditional Chinese Medicine According to Evidence-Based Medicine and Expert Consensus Opinion. Evid Based Complement Alternat Med, 2014: 492193. https://doi.org/10.1155/2014/492193
[29] Pang B, Guo J, Zhao L, et al., 2016, Retrospective Study of Traditional Chinese Medicine Treatment of Type 2 Diabetes Mellitus. J Tradit Chin Med, 36(3): 307–313. https://doi.org/10.1016/s0254-6272(16)30042-5
[30] Lv Renhe, Zhao Jinxi, 2009, Diagnosis and Treatment of Diabetes and Its Complications, People’s Medical Publishing House, 209–214.
[31] Case Introduction and Discussion on the Treatment of Extraspinal Soft Tissue Damage Caused by Male Sexual Dysfunction in the Lower Back, Buttocks, Waist and Buttocks or Combined With Soft Tissue Release Surgery at the Base of the Thigh, n.d., Soft Tissue Surgery, 2009, 1141–1149.
[32] Yuan L, 2011, Research Prospects of Fasciology, Tsinghua University Press, 160–174.
[33] Feng R, Wang Z, 2020, Clinical Application of Ultrasound Therapy, Practical Ultrasound Therapy, 59–82.
Publisher’s note
Bio-Byword Scientific Publishing remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is excerpted from the Proceedings of Anticancer Research, 2023, Volume 7, Issue 6 by Wound World.