Nurse practitioners play a vital role in advocating for practice change and should be involved in health policy formulation and decision making to drive the effectiveness of healthcare systems. Motivated by patient experience, informal carer experience and optimal use of their time, numerous nurses are already adopting a shared care approach when managing patients with chronic wounds. Formalising shared care in chronic wound management at the service provider level may help reduce practice variation, optimise resource allocation and simplify implementation.
While the implementation of shared care requires initial investment in training, infrastructure and education, the short and longterm benefits may outweigh the initial costs.
An estimated 2–4% of total healthcare expenditure in Europe is for wound care (Posnett et al, 2009), with wound costs outpacing increases in healthcare budgets (Milne et al, 2020; Guest, 2021). The incidence of wounds outnumbers the appointments that trained clinicians have available to care for them and the number of retiring nurses outpaces the number of newly qualified nurses (Milne, 2016; Buchan et al, 2020).
Additionally, due to resource constraints, care in hospitals is primarily focused on wound treatment as opposed to prevention. Discharge to the community is rapid, making wound management a significant part of the caseload for non-acute nursing teams and generalist nurses who are not specifically trained in wound care (Welsh, 2018; Blackburn et al, 2019).
Wound management commands over 50% of community nursing time (Lindholm and Searle, 2016), hours that are urgently needed elsewhere (Buchan et al, 2020). Furthermore, given the ageing population, earlier hospital discharges and continued threat of diabetes and obesity, the incidence and cost burden of chronic wounds will only continue to rise (Lindholm and Searle, 2016; Sen, 2021).
Against a backdrop of nursing shortages (Buchan et al, 2020), the demands on nursing time will become unmaintainable if the current trend continues; health systems must identify more efficient ways of managing the huge workload posed by chronic wounds (Lindholm and Searle, 2016).
Chronic wound care is a prime example where innovative ways of working could improve patient outcomes and satisfaction while also ensuring that healthcare resources are used in the most valuable way.
Shared wound care, an approach developed and led by a global group of nurses, encourages appropriate patients to take an active role in their ongoing wound healing (Moore et al, 2021). It has been estimated using a mathematical model that shared care practices alongside long-wear advanced foam dressings (such as ALLEVYN™ LIFE Dressing, Smith + Nephew) can release up to 3.5 billion hours globally by 2030 (Moore et al, 2022).
Behaviour change interventions, such as the scaling up of shared wound care, has the potential to improve care delivery for patients, practitioners and service providers. In addition to clinical evidence, implementation tools and best practice recommendations, behaviour change processes also require stakeholder engagement to fully realise its potential (Byrne, 2019).
It is estimated that 60% of patients with chronic wounds already have some degree of involvement in their wound care (Moore and Coggins, 2021), such as monitoring and changing dressing. Up to 26% of patients are likely to be fully self-sufficient, and 49% are in favour of 5–7 day wear-time dressings to prevent disruption to their lifestyle such as working and socialising (Moore and Coggins, 2021; Ryan and Post, 2022).
Community nurses, on the other hand, have now reached a point where they require more support from service providers in order to formally implement a shared care approach in chronic wound care, whether it be through access to long-wear advanced foam dressings, training or implementation tools or simply permission and effective reporting infrastructure (Loney and Moore, 2023).
Practitioners are key in developing a simple, formalised process for shared care, drawing insights from best practice pathways already in place for a variety of chronic illnesses. Many practitioners may underestimate the power and influence of their voices when advocating for innovation with policymakers and service providers. With real-world experience, individual practitioners can provide valuable insights on a product or care pathway to enable decision makers to make changes (Nusgart, 2021).
The aim of this article is to empower discussions between nurse practitioners and service providers as to why shared care should be implemented formally in chronic wound care and address concerns regarding its perceived complexity or cost.
Chronic wound care: the provider’s perspective
Shared wound care incorporates a range of practice interventions, from medication to nutrition advice, through to daily dressing management and method of interaction where remote communication, such as telehealth is becoming more common. Many healthcare professionals (HCPs) are keen to involve the patient as much as possible, with the main barrier being inconsistency of implementation across the care team (The Nursery, 2020).
Formalising a shared wound care protocol at a service provider level may mitigate concerns and deliver benefits for patients, practitioners and service providers.
The overarching benefit of formalising a shared care approach in wound care is that tools for reducing practice variation in wound assessment, management and reporting are made available (Moore et al, 2021; World Union of Wound Healing Societies, 2020). Many nurses are already implementing the approach on an individual or informal basis (Kapp and Santamaria, 2017), but establishing a standard protocol will enable the full benefits of shared care to be unlocked. This process can create cost efficiencies with advanced products and simplify implementation complexity.
Using a tool such as the Shared Wound Care Discussion Guide (SWCDG) provides the clinician with a process to follow and can help the most appropriate patients be identified for involvement in their care (Moore et al, 2021). Working alongside their healthcare provider to tailor a treatment plan can further enhance patient involvement and active engagement (Elsinga et al, 2022). Using internationally validated practice and patient training tools, practitioners will be able to communicate the shared care approach to patients more efficiently to better identify suitable and willing individuals (Moore et al, 2021). Formalising shared care in wound management could create economies of scale in relation to more appropriate use of advanced wound dressings and enable stringent processes, standards and risk assessments to be put in place.
Shared wound care: a cost-benefit discussion
The financial burden associated with chronic wounds is significant due to their prolonged existence or recurrence over several years, which may require medical interventions daily (Callaghan et al, 2012). Compared to acute wounds, chronic wounds use significantly more resources per patient; they necessitate over 2.5x as many nurse visits, twice as many prescriptions and over 2.5x as many wound care products (Guest et al, 2017).
In light of increasing demands on health systems, service providers are looking for ways to maximise efficiency and efficacy (Walters et al, 2022). This may be by reducing resource costs, costly patient complications or delayed healing, and maintaining and upskilling their workforce.
When considering efficiency improvements, service providers may first consider easy targets, such as supply budgets, which are quantifiable and provide immediate short-term savings (Lindholm and Searle, 2016). However, wound care products are not always the primary cost driver in wound management, accounting for only 6% of total annual costs (Guest et al, 2020). Instead, district/community nurse visits are the largest financial contributor, accounting for 29% of the total cost, general practitioner visits for 18%, healthcare assistant visits for 17% and practice nurse visits for 7% (Guest et al, 2020). It is crucial that healthcare providers consider the opportunity cost of resources, which is often less easy to quantify. The loss of potential benefits of resources that are allocated to a particular activity, highlights the opportunity cost (Lindholm and Searle, 2016). In this case, the question can be posed: ‘In our current way of working, what other activity or task have we given up for this nurse to undertake treatment?’.
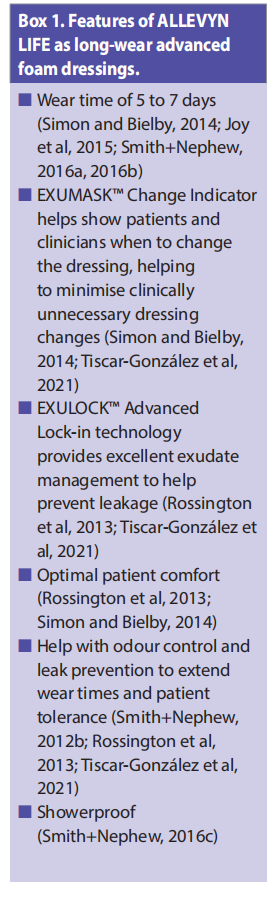
Long-wear advanced wound care dressings such as ALLEVYN LIFE Dressing are well designed to assist with the implementation of shared care due to their extended wear time, exudate management capabilities, comfort and promotion of patient independence [Box 1].
The benefits of such long-wear advanced foam dressings do come at a higher individual price point and, therefore, the opportunity for holistic cost reductions may be overlooked. For example, the time dedicated to clinically unnecessary dressing changes removes the opportunity for the practitioner to treat someone else or undertake other valuable or higher urgency activities. This time has a monetary cost that can be used to support the call for enshrining shared wound care as a standard care option. Specifically, wound care requires a significant portion of a nurse’s time. A nurse can see over three times as many patients with diabetes in a clinic setting than they can when making home visits to patients with wounds. Releasing nurse time is about maintaining care quality while increasing efficiency, which could potentially be the key to solving the problem of the growing demand for services (Lindholm and Searle, 2016).
Focusing discussions on direct dressing costs associated with more expensive long-wear foam dressings may initially make shared wound care approaches seem prohibitively expensive. Instead, conversations should focus on the potential efficiency gains which relate to three cost drivers: dressing change frequency, time to heal a wound and incidence of complications (Lindholm and Searle, 2016).
Cost drivers in shared wound care Frequency of dressing changes
When looking at resource allocation in wound management, practitioner time is the biggest contributor to the financial burden of wound care, especially in community services (Guest et al, 2020). In the UK, approximately 60% of community nurses’ time is spent changing wound dressings (Lindholm and Searle, 2016), which is why service providers must consider the frequency of dressing changes as a significant driver of cost.
Using long-wear advanced dressings, that have an evidenced wear time of 5–7 days can reduce dressing changes by 50% (Joy et al, 2015). Using such dressings where appropriate in combination with a shared care practice approach could result in major efficiency savings, not only by reducing frequency of dressing changes but also releasing HCPs’ time to other duties (Moore et al, 2022).
Individuals with more complex wounds who are at greater risk of complications require more regular assessment, so wound dressings will need to be changed more frequently. Tools such as, M.O.I.S.T. (Moisture balance, Oxygen balance, Infection control, Supporting strategies, Tissue management), SWCDG, T.I.M.E. CDST (Tissue, Infection and inflammation, Moisture balance, Edge of the wound clinical decision support tool), can be used to help identify these patients and mark them as potentially unsuitable for shared wound care until wound healing has progressed (Moore et al, 2019; 2022).
Incidence of complications
Clinically unnecessary dressing changes driven by rigid schedules can lead to various wound healing complications. This includes mechanical disturbance to the healing process, loss of temperature (affecting the cellular healing process) and providing an entry portal for harmful bacteria at the exposed wound site (Blackburn et al, 2018). Consequently, it increases the risk of wound contamination, disrupts the healing process and delays wound closure (Sen, 2019).
The annual expenditure for a patient with an unhealed wound can be up to £7,886, with demands expected to increase due to an ageing population and comorbidities (Lindholm and Searle, 2016; Guest, 2020). Instances of unanticipated dressing failures arise from poor performance, such as dressing leakage due to lifting borders, weak adherence to the skin and excessive visible dressing strikethrough.
Long-wear advanced foam dressings can be left in situ for 5–7 days thereby reducing the frequency of wound exposure (Joy et al, 2015). Undisturbed wound healing can be optimised by using long-wear advanced foam dressings such as ALLEVYN LIFE Dressing, which minimises trauma to the wound bed upon removal, improving healing outcomes (Hurd et al, 2009; Vowden et al, 2011).
Time to heal a wound
Shared wound care‘s main clinical benefit is undisturbed healing, where it is commonly agreed by clinicians that it is best practice to leave a dressing in situ rather than to engage in clinically unnecessary dressing changes dictated by nursing schedules. Long-wear advanced foam dressings facilitate undisturbed healing, making them an ideal complement to a shared care approach (Stephen-Haynes, 2015).
Using long-wear advanced foam dressings as part of a shared wound care approach has the potential to release more than 10%, or approximately 400 million hours of nursing time spent on dressing changes in the community* (Rossington et al, 2013; Simon and Bielby, 2014; Joy et al, 2015; Tiscar-González et al, 2021; Moore et al, 2022). Releasing this time has the potential to improve patient quality of life and allow nurses to spend more time avoiding complications in higher risk patients. Complications can lead to complex wound management and extend healing time, increasing workload on an already overstretched nursing population.
Patients who are involved in their dressing changes are also trained to monitor and identify the early signs of potential complications and notify their practitioner as part of the shared wound care approach (Elsinga et al, 2022).
Controlling complexity: implementation costs of shared care
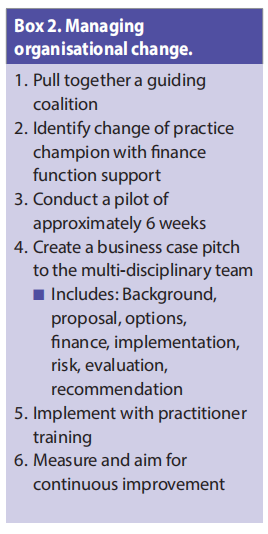
Implementing shared care alongside long-wear advanced foam dressings would not require extensive investment to pilot initially to understand the potential gains. There is no significant initial cost outlay for service providers; they do not need to invest in expensive equipment, commit to a lengthy industry contract or hire new staff. Additional documentation and auditing are not necessarily complex either, they need detailed patient records and notes, as well as a way to calculate time/cost savings (Loney and Moore, 2023).
The financial opportunities created by shared care are more obtainable to some healthcare systems within some countries than others; depending on the healthcare infrastructures in place. While introducing shared care approaches requires time investment from the outset, there are both short- and long-term benefits (Moore et al, 2022). In the short term, implementing new training and new approaches to clinical practice has been shown to increase staff motivation. Pilot shared care programmes can be designed and implemented in as little as 8 weeks, allowing patients, practitioners and providers to see clinical, quality of life and productivity benefits and make adjustments for wider roll out (Scalise et al, 2023).
Long-wear advanced foam wound dressings have a comparatively higher price than standard wound dressings. However, especially when implemented alongside shared care, they could substantially reduce main cost drivers in wound care. By fostering a collaboration between budget managers and those who prescribe, a cost-benefit case can be constructed (Moore et al, 2022). Aside from the cost of long-wear advanced foam dressings, other initial costs to implement shared care would include telehealth infrastructure, patient and carer education (with associated materials), as well as multidisciplinary meetings with nurses, surgeons and primary care providers, many of which are already in place or available with the support of industry partners (Loney and Moore, 2023).
Tools have been created to assist clinicians in assessing a wound (T.I.M.E. CDST), assessing a patient’s behavioural suitability for shared care (SWCDG), applying best practice (Case Series: Shared wound care discussion guide) and applying step-by-step implementation: (Shared wound care: Made Easy) (Moore et al, 2019, 2021, Elsinga et al, 2022; Loney and Moore, 2023). All of these tools contribute in some way to standardise the implementation of shared wound care at an individual practitioner level.
Conclusion
The World Health Organization (WHO) predicts that the world will require an extra nine million nurses and midwives by 2030 to meet the United Nations Sustainable Development Goal 3, that focuses on health and wellbeing (WHO, 2022). Evidence suggests that up to half of chronic wound dressing changes may be clinically unnecessary (Joy et al, 2015). It is important for healthcare providers and nurses to consistently question if they can use community nursing time to deliver more timely care and accommodate a greater number of patients in need (Lindholm and Searle, 2016). With that question in mind, shared care is an approach that service providers should consider formalising for chronic wound management.
The WHO State of the World’s Nursing 2020 report urged governments and all key stakeholders to strengthen nurse leadership in order for nurses to have an influential role in health policy formulation and decision making, as well as contribute to the effectiveness of health and social care systems (WHO, 2020). Practitioners have a vital role to play and are ready to start advocating for a shift in practice change when they see fit.
These discussions not only advocate for change in attitude to shared care, but attitude towards chronic wounds in general. It must be taken into consideration that chronic wound management is a particularly challenging field. Firstly, chronic wounds are often considered secondary to the main disease, as opposed to being classified as a disease themselves. Secondly, as chronic wounds are often the result of a wider systemic disease, wound care is interdisciplinary with many different people and services involved in the patient treatment journey, increasing the risk of miscommunication or treatment failure (Lindsay et al, 2017).
A widely accepted shared wound care approach will make steps to address these challenges. There is a need for decision makers and legislators to recognise chronic wounds as a disease that does not exist in isolation. This requires a dedicated strategic plan for ongoing management, similar to what has been done for other conditions that impose a significant burden on healthcare systems, such as cancer, cardiovascular diseases and neurodegenerative diseases (Mahmoudi and Gould, 2020).
It would be highly beneficial for practitioners and service providers to work together to take the lead in standardising protocols across the continuum of care, to reflect the changes in practice, like shared wound care. Recognition that chronic wounds are a disease entity is a primary goal that will unify the field of wound healing, promote education for future generations and facilitate the development of new products, which will all continue to bring innovation and quality of life improvements to patients. See Box 2 for a plan on managing organisational change.
In order to effectively implement and integrate this practice shift within healthcare systems, healthcare practitioners and patients require access to long-lasting advanced foam dressings, tools to access patient eligibility for shared wound care, and educational resources led by nurses and other healthcare providers.
References
1. Blackburn J, Stephenson J, Atkin L et al (2018) Exploring and understanding challenges in clinical practice: appropriate dressing wear time. Wounds UK 14(5): 56–64
2. Blackburn J, Ousey K, Stephenson J (2019) Nurses’ Education, Confidence, and Competence in Appropriate Dressing Choice. Adv Skin Wound Care 32(10): 470–476
3. Buchan J, Catton H, Shaffer FA (2020) Ageing well: Policies to support older nurses at work. International Centre on Nurse Migration Available at: https://www.icn.ch/ sites/default/files/inline-files/Ageing%20ICNM%20 Report%20December%209%202020.pdf
4. Byrne M (2019) Increasing the impact of behavior change intervention research: Is there a role for stakeholder engagement? Health Psychology 38(4): 290–296
5. Callaghan R, Chadwick P, Mahoney K, Stephen-Haynes J (2012) Case series evaluation: The use of Allevyn gentle border multisite on chronic wounds. Wounds UK 8: 110–118
6. Elsinga B, Loney A, Post H et al (2022) Case series: Shared wound care discussion guide. Wounds International Available from: www. woundsinternational.com
7. Guest JF, Vowden K, Vowden P (2017) The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care 26: 292–03
8. Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 10: e045253
9. Guest JF (2021) Burden of wounds to the NHS: what has changed since 2012/13? Wounds UK 17(1): 10–15
10. Hurd T, Gregory L, Jones A, Brown S (2009) A multi-centre in-market evaluation of ALLEVYN◊ Gentle Border. Wounds UK 5(3): 32-44
11. Joy H, Bielby A, Searle R (2015) A collaborative project to enhance efficiency through dressing change practice. J Wound Care 24: 312–317
12. Kapp S, Santamaria N (2017) How and why patients selftreat chronic wounds. Int Wound J 14: 1269–127
13. Lindholm C, Searle R (2016) Wound management for the 21st century: combining effectiveness and efficiency. Int Wound J 13: 5–15
14. Loney A, Moore Z (2023) Shared wound care discussion guide: Made Easy. Wounds International Available from: www. woundsinternational.com
15. Mahmoudi M, Gould L (2020) Opportunities and Challenges of the Management of Chronic Wounds: A Multidisciplinary Viewpoint. Chronic Wound Care Management and Research 7: 27–36
16. Milne J (2016) The challenge of providing cost-effective wound care. Wounds UK 12(1): 52–57
17. Milne J, Searle R, Styche T (2020) The characteristics and impact of hard-to-heal wounds: results of a standardised survey. J Wound Care 29(5): 282–288
18. Moore Z, Dowsett C, Smith G et al (2019) TIME CDST: An updated tool to address the current challenges in wound care. J Wound Care 28: 154–161
19. Moore Z, Coggins T (2021) Clinician attitudes to sharedcare and perceptions on the current extent of patient engagement in wound care: Results of a clinician surer. Wounds International 12(1): 48–53
20. Moore Z, Kapp S, Loney A et al (2021) A tool to promote patient and informal carer involvement for shared wound care. Wounds International 12: 86–92
21. Moore Z, Loney A, Probst S et al (2022) 3.5 billion hours of nurse time released by 2030: Potential efficiency gains from shared care and long-wear advanced foam dressings. Wounds International 13(2): 32-38
22. Nusgart M (2021) Wound Clinics and Wound Care Advocacy: Advocating for Evidence-Based Coverage and Reimbursement. Wound Care Learning Network Available at: https://www.hmpgloballearningnetwork. com/site/twc/wound-clinics-and-wound-careadvocacy-advocating-evidence-based-coverage-andreimbursement.
23. Posnett J, Gottrup F, Lundgren H, Saal G (2009) The resource impact of wounds on health-care providers in Europe. J Wound Care 18: 154–161
24. Rossington A, Drysdale K, Winter R (2013) Clinical performance and positive impact on patient wellbeing of ALLEVYN Life. Wounds UK 9: 91–95
25. Ryan H and Post H (2022) Shared wound care continuum: Factors that influence a patient’s preference and suitability for shared wound care. Wounds International 13(4): 54–60
26. Scalise A, Arizmendi M, Vicente H et al (2023) Evaluation of a five-layer hydrocellular polyurethane foam dressing across wound care settings in southern Europe. Journal of Wound care 32(2): 62-128
27. Sen CK (2019) Human Wounds and Its Burden: An Updated Compendium of Estimates. Adv Wound Care 8(2): 39-48
28. Sen CK (2021) Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv Wound Care 10: 281–292
29. Simon D, Bielby A (2014) A structured collaborative approach to appraise the clinical performance of a new product. Wounds UK 10: 80–87
30. Smith+Nephew (2012a) Odour reducing properties of ALLEVYN Life. Internal Report DS/12/127/DOF
31. Smith+Nephew (2016a) Wound Model Testing of New ALLEVYN Life Gen2 wcl Dressing using Horse Serum at a Flow Rate Modelling that of a Moderately Exuding Wound. DS/14/303/R
32. Smith+Nephew (2016b) A Randomised Cross-Over Clinical Evaluation to Compare Performance of ALLEVYN Life and Mepilex® Border Dressings on Patient WellbeingRelated Endpoints. Internal Report. CE/047/ALF
33. Smith+Nephew (2016c) Product Performance of Next Generation ALLEVYN Life Internal Report. (HVT080) GMCA-DOF/08
34. Stephen-Haynes J, Bielby A, Searle R (2013) The clinical performance of a silicone foam in an NHS community trust. Journal of Community Nursing 27: 50–59
35. Stephen-Haynes J (2015) The benefits of undisturbed healing using ALLEVYN Life™. Wounds International 6(4): 18-21
36. The Nursery (2020) Community nursing data table. Selfcare approaches to patient wound care and the impact of Covid-19. Available at: https://www.nursingtimes.net/ news/community-news/nurses-report-negative-impact of-pandemic-on-wound-care-patients-05-05-2022/
37. Tiscar-González V, Menor-Rodríguez M, Rabadán-Sainz C (2021) Clinical and Economic Impact of Wound Care Using a Polyurethane Foam Multilayer Dressing. Adv Skin Wound Care 34: 23–30
38. Vowden K, Moiemen N, Drysdale K, Mistry C (2011) An open, prospective randomised, multi-centre clinical evaluation of a hydrocellular silicone foam dressing* in the management of exuding chronic and acute wounds. Paper presented at: EWMA, Brussels
39. Walters JK, Sharma A, Malica E, Harrison R (2022) Supporting efficiency improvement in public health systems: a rapid evidence synthesis. BMC Health Serv Res 22: 293
40. Welsh L (2018) Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. Int Wound J 15: 53–61
41. World Health Organization (2020) State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership. Geneva: WHO. Available at: https://www.who.int/ publications/i/item/9789240003279 (accessed 26.09.2023)
42. World Health Organization (2022) Nursing and Midwifery. Geneva: WHO. Available at: https://www.who.int/ news-room/fact-sheets/detail/nursing-and-midwifery (accessed 26.09.2023)
43. World Union of Wound Healing Societies (2020) Strategies to reduce practice variation in wound assessment and management: The T.I.M.E. Clinical Decision Support Tool.
Declaration
This article is sponsored by Smith+Nephew via an educational grant; the content has been independently produced and reviewed and does not necessarily reflect the views of Smith+Nephew.
This article is excerpted from the Wounds International 2023 | Vol 14 Issue 3 by Wound World.


