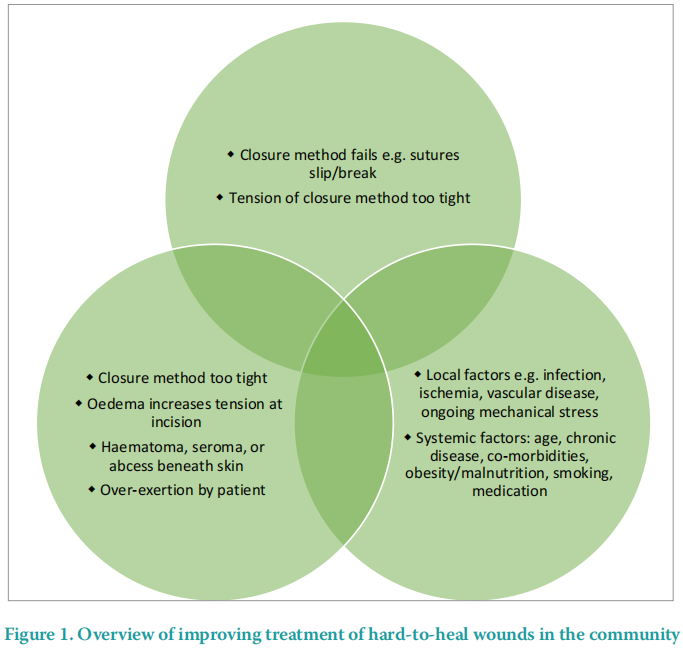
Surgical wound dehiscence (SWD) is a complication of surgery. It is the separation of the margins of a closed surgical incision that has been made in skin, with or without exposure or protrusion of underlying tissue, organs or implants. Separation may occur at single or multiple regions, or involve the full length of the incision, and may affect some or all tissue layers. A dehisced incision may, or may not, display clinical signs and symptoms of infection (World Union of Wound Healing Societies [WUWHS] 2018). SWD usually occurs five to eight days after the surgical procedure, while still in the early stages of the healing process (Rosen and Manna, 2022). SWD can occur due to technical issues with the incisional closure method used, from mechanical stresses placed on the incision site, from disruption to healing due to local or systemic factors, or a combination of all three (Figure 1).
The development of dehiscence can delay the healing process of a wound. Consequently, the wound needs to be dressed for longer, which necessitates additional nursing care, especially within the community. In the UK, 58% of dehisced wounds healing by secondary intention were reported as being cared for in the community setting (Chetter et al, 2017). This has an added financial strain, which increases the already stretched economic burden placed on the healthcare provider (WUWHS, 2018). Alongside this is the impact on the patient. Living with a wound that has dehisced can negatively impact on a patient’s mental health, their physical and social wellbeing, create financial worries due to loss of income, such as inability to work, which leads to a reduced quality of life (QoL; Correa et al, 2016).
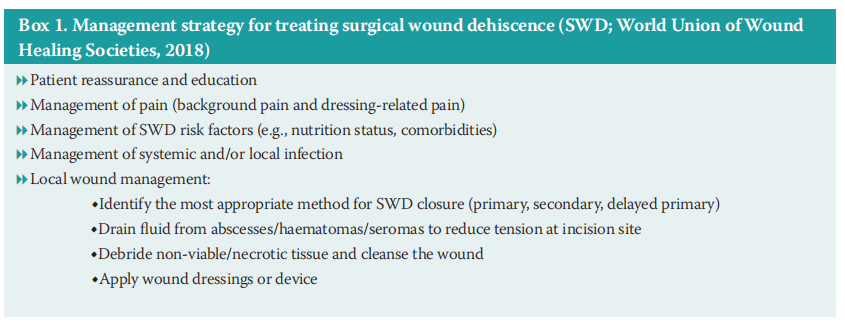
Wound closure is the fundamental goal for the management of a SWD (Box 1). An important aspect of this is the reassurance and education of the patient and their family/carers, to ensure all involved work together as a team. A strategy to manage pain, whether background or local, should be implemented and a local treatment plan for the SWD prepared and put in place. Wound dressings/ devices play an important role in this plan, as they must provide appropriate exudate management while maintaining a moist wound environment for optimal healing, ensure the elimination of dead space to help reduce the risk of infection.
Negative pressure wound therapy (NPWT) is a treatment that optimises wound healing through the application of sub-atmospheric pressure to help reduce wound exudate and promote the formation of granulation tissue (Zaver and Kankanalu, 2023). Historically NPWT has been used to manage open acute and chronic wounds, for example fasciotomy wounds and diabetes-related foot ulcers. More recently NPWT has been used in the management of closed wounds, for example closed surgical incisions and skin grafts, with the aim of reducing oedema and seroma formation, preventing surgical dehiscence in high-risk incision sites, and promoting granulation to encourage healing (Zaver and Kankanalu, 2023).
NPWT has mainly been used in the acute care settings, although its use in community health care is increasing, improving the QoL for the patient and reducing both the reliance on hospital-based care and wound care management costs, estimated to be £8.3 billion to the NHS in the UK (Murdoch et al, 2021). Traditionally, the use of NPWT in the community has been limited and dependent on the care provider and the resources available (Guy and Grothier, 2012; Othman, 2012). The size and weight of the pumps and canisters, and the reliance on the first generation of NPWT systems, also restricted the adoption of this intervention beyond acute care hospitals (Apelqvist et al, 2017). However, the recent introduction of portable, single-use systems has made NPWT more accessible to patients being treated in the community (Orlov and Gefen, 2021).
Intended for use on closed incisions and a variety of open wound types, Avance Solo (Molnlycke Healthcare Ltd), is a portable, battery-powered, single-use, NPWT system that features Controlled Fluid Management technology. It shares fluid management between an absorptive multilayered dressing (Avance Solo Border with Safetac adhesive to minimise trauma to the wound site and surrounding skin on removal) and a 50ml canister that can be easily replaced by carers and patients. The system delivers –125mmHg continuous, regulated pressure for up to 14 days, and features both audible and visual alarms to facilitate efficient and timely restoration of therapy.
Here we describe the use of Avance Solo selected as a therapy for both the prevention of and the treatment of SWD in a patient with complex medical and social needs.
CASE REPORT
A 25-year-old male patient with functional hemiparesis and hemianopia with visual loss (registered blind) was living with complex medical needs due to the due to autonomic failure, (a neurodegenerative disease of the autonomic nervous system), which can affect heart function, blood pressure, bladder function, and digestion. The patient suffered from paroxysmal symptomatic sinus tachycardia, postural orthostatic tachycardia syndrome, neurogenic bladder, irritable bowel syndrome, gastroesophageal reflux and oesophageal dysmotility. In addition, he had required regular dialysis over a several year period for chronic nephrotic dysfunction, had a diagnosis of loin pain haematuria syndrome, and urinary metadrenalines had been detected. The patient lived with constant pain which, when measured on a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (maximum pain), was generally rated as VAS 6. Furthermore, a constant feeling of nausea impacted on his nutritional intake, and this was confounded further by his mobility and sight issues that made food preparation difficult. He was diagnosed with multifactorial clinical depression in addition to his other comorbidities.
At the beginning of October 2021, due to episodes of dizziness and fainting linked to an erratic heart rate, an artificial cardiac pacemaker was subcutaneously implanted into the left side of the patient’s chest. Initially, the incision site was closed using sutures. After 10 days, the epidermis and upper layer of the wound had dehisced by 50%. Despite the use of a variety of conventional wound dressings, alongside antibiotics for a suspected wound infection, the wound remained unhealed. In addition, there was lymph node involvement, not due to infection but related to issues associated with his ongoing chronic autonomic failure, that caused significant pain and reduced the patient’s movement. Three weeks after implantation of the pacemaker, further revision surgery was performed to support re-closure of the wound, but this also failed, with the wound still unhealed.
Early in December 2021, the clinicians treating the patient asked for support from a Tissue Viability Specialist (TVS) to help manage the complex requirements of the wound. As the skin of the wound and periwound was prone to skin tearing due to its fragility, together with its nonhealing nature, treatment with Avance Solo NPWT system, was recommended. Before the application of NPWT, the wound area measured 2.5cm2 with a depth of 0.2cm. After 10 days of treatment, the condition of the wound had improved; the wound area had reduced by 32% to 1.7cm2 with wound depth unchanged. However, due to ongoing significant pain and lymph swelling, in addition to a query concerning a possible allergic reaction to the pacemaker due to the autonomic disease condition, the cardiology consultant felt it was prudent to remove the pacemaker and implant a new one. Implantation was into the right side of the patient’s chest, but with a slightly deeper application into the muscle; dissolvable sutures were used. Application NPWT to each surgical site on completion of the surgical procedures was planned to support wound closure and to help reduce the risk of non-healing.
NPWT was applied to the sutured 7cm incision site on the left side 30 minutes postoperatively, but, as the sutured 6cm incision site on the right side was incredibly painful (postoperative pain severity rated as VAS 10), a decision was made to delay its application for 1 week at the request of the patient. In its place, Mepilex Border (soft silicone foam dressing) was applied, with the plan to apply Avance Solo when the patient returned for the first dressing change to the wound on the left side.
On review, postoperative day six, both wounds exhibited superficial dehiscence; the left wound dehiscence measured 2.5cm2 with a depth of 0.2cm, and the right wound dehiscence measured 1cm2 , with no depth. There was no sign of wound infection, but lymph node swelling remained. The periwound skin of each wound was healthy, and wound exudate was low, non-viscous and clear/ serous in its appearance. The patient reported the pain level as VAS 6. Both wounds were re-dressed and NPWT was re-applied. After a further 9 days (postoperative day 15; Figure 2A–B), the dehisced areas of both wounds had reduced, the left side by 60% to 1cm2 and the right by 25% to 0.75cm2 . Both wound beds were composed of granulating tissue and the periwound skin remained healthy, but lymph node swelling persisted. Wound exudation had increased to moderate in the left wound but the right wound was dry.
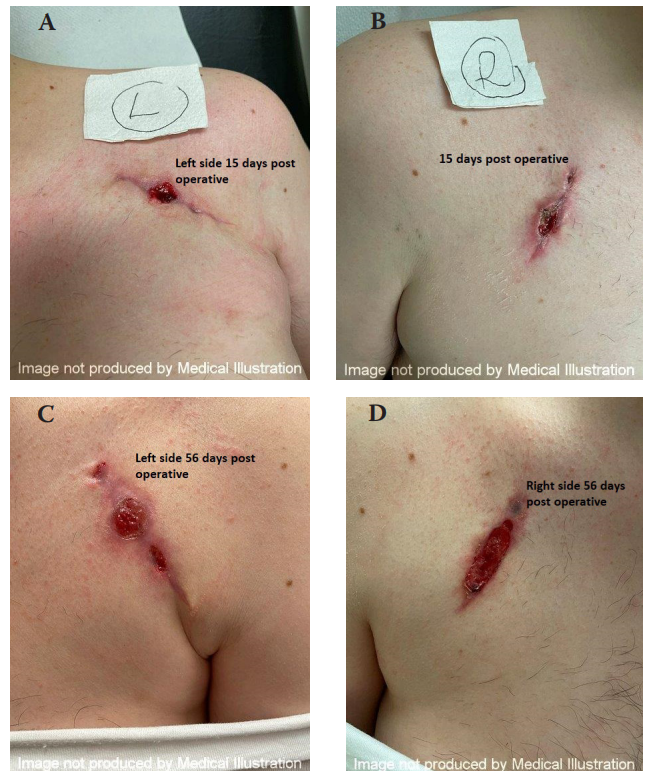
Figure 2. Postoperative day 15 A–B. Postoperative day 56 C–D
Unfortunately, at that time, there was no support available for the use of the NPWT system within the community nurse setting, necessitating the patient to attend weekly hospital appointments for dressing changes. He felt he needed a rest from having the two NPWT systems applied, and so was happy to revert to using conventional wound dressings. Flaminal Forte (antimicrobial alginate gel for high to moderate exuding wounds; primary dressing) and Mepilex Border were used to dress the left wound. The right wound was dressed using Mepilex Border. Initially the patient was self-caring with help from his husband. Dressings were changed every 3–4 days. Assessment on postoperative day 36, found the condition of both wounds had deteriorated. The left wound had increased in area to 4cm2 with a depth of 0.5cm and, although the wound exudate level remained moderate, it was serosanguinous/blood in its appearance. Pain had increased (VAS 8). The area of the right wound had increased to 2.5cm2 with a depth of 0.3cm, and it was exuding again, although it was low in volume and clear/serous in appearance. Lymph node swelling remained despite the wounds being free from infection. In contrast, granulating tissue continued to cover the wound beds and the periwounds were healthy, albeit the skin of the right wound was drier than previously observed.
At this point, the patient’s personal circumstances changed significantly, placing him under immense stress. This resulted in a loss of support with his personal care, and an inability to prepare food, which resulted in a nutritional deficit and considerable weight loss, which impacted on his healing. Consequently, the patient needed to be re-homed and a new care plan implemented to provide help with his ongoing social and wound care difficulties. He agreed to the continued use of conventional dressings, rather than resume treatment with Avance Solo, as he was worried about the care he would receive, as he had a different carer each day and he felt there was a lack of consistency in approaches to his care. Treatment was continued with no change to the regime, with the exception of emollients which were applied to the dry periwound skin of the right wound. The dressings were changed every four days.
After postoperative day 56, the original dehisced wound on the left incision was stable at 4cm2 but two new smaller areas had opened, measuring 0.5cm2 and 0.25cm2 , both with a depth of 0.2cm (Figure 2C–D). As the patient had more mobility in his left arm, he believed the increased ‘reaching and stretching’ required due to increased self-care led to the recently healed sections of the incision site to 'tear open'. However, there was a reduction in wound exudation, which was clear/serous in appearance, and the periwound edges were dry. Pain was rated between VAS 6 and 8. The dehisced wound on the right was, once again, superficial (no depth) and the wound area had reduced slightly by 16% to 2.1cm2 . Wound exudation was unchanged and the periwound remained dry. Wound pain was no greater than the patient’s normal baseline level of VAS 6. As the patient was happy with the healing progress of the wounds, believing it to be 'quicker than usual', the treatment regime was continued, with the exception of Flaminal Hydro (antimicrobial alginate gel for moderate-to-low wound exudate) being applied to the dehisced wound on the left side, and emollient applied to the periwound skin of both wounds.
The patient continued to self-care, with help from a social carer and daily carers from a home care service. However, the patient was concerned that the carers, who were not nurses or trained in healthcare, kept “ripping off ” the wound dressings each day, which removed the scab and resulted in the re-opening of the wounds. This daily re-dressing of the wounds was not written into the patient’s care plan and went against both the patient’s wishes and the advice from the TVS. However, following a discussion between the TVS and carers, this practice was stopped and, eventually, 74 days after the surgical procedure to remove and re-implant the pacemaker, all the dehisced areas of the wounds had re-epithelialised. Scabbing of the left wound remained, and a VAS of 8 was recorded still for the wound. However, lymph node swelling had finally resolved. The application of emollient to both of the healed wound areas was continued to aid strengthening of the periwound skin, as well as to help reduce possible ‘tearing’ issues of the new skin, and to soften the scabbed areas still present on the left wound. In addition, Cosmopore (self-adhesive island wound dressing) was applied over the healed wounds to protect the new epithelial tissue.
After postoperative day 98, the patient was discharged from the care of the TVS, with advice on how to support ongoing skin maturation and to ensure he protected the area from the sun.
Learnings
This case study highlights the impact that underlying complex health conditions can have on a patient’s ability to self-heal, as well as the requirement for support from a multidisciplinary care team to achieve a successful outcome. Unfortunately, healthcare systems and processes do not easily navigate the boundaries between health care and social care, which can lead to misunderstandings, delays and missed opportunities for support, with the consequences ultimately impacting on the patient, both physically and psychologically.
In complex medical cases, a complete treatment plan will generally not fall within the remit of just a single healthcare professional. Unfortunately, professionals can be inclined to work in a silo, with each individual/team working on the same objective but with no communication. Therefore, to ensure the needs of the patient are met, it is imperative that one professional involved in the patient’s care takes the lead and coordinates the management of the healthcare plan.
This case study demonstrates how such a collaboration of multidiscipline professionals was able to work together with a common goal to achieve a successful outcome for the patient. As well as requiring wound care for a closed incision wound following a pacemaker implantation, the patient needed additional support with his social, psychological and physical wellbeing. These needs were met by the successful interaction of the lead healthcare professional who coordinated and built links with the community nursing team, the patient’s general practitioner, a nutritionist, as well as social services who provided the patient with social care and daily carers. As a result, a positive patient outcome was achieved that encompassed all the patient’s needs, rather than wound care alone. Such collaborations help to build links and develop closer multidisciplinary working relationships that allow for the sharing of knowledge, both clinical and procedural, but simultaneously foster a key therapeutic relationship with the patient.
With this in mind, this article successfully illustrates how a multidisciplinary team can achieve a positive outcome of a hard-to-heal incision wound while ensuring the patient’s social care and wellbeing.
REFERENCES
1. Apelqvist J, Willy C, Fagerdahl A-M et al (2017) Negative pressure wound therapy – overview, challenges and perspectives. J Wound Care 26(Supplement 3):S1–113. https://doi.org/10.12968/jowc.2017.26.sup3.s1
2. Chetter IC, Oswald AV, Fletcher M, et al (2017) A survey of patients with surgical wounds healing by secondary intention; an assessment of prevalence, aetiology, duration and management. J Tissue Viability 26(2):103–7. https://doi.org/10.1016/j.jtv.2016.12.004
3. Correa NFM, de Brito MJA, de Carvalho Resende MM et al (2016) Impact of surgical wound dehiscence on health-related quality of life and mental health. J Wound Care 25(10):561–70. https://doi.org/10.12968/ jowc.2016.25.10.561
4. Davies P (2022) Closed incision negative pressure wound therapy: a literature review and an introduction to Avance Solo. Wounds International. https://tinyurl.com/29b9bvwa (accessed 3 September 2023)
5. Guy H, Grothier L (2012) Using negative pressure therapy in wound healing. Nursing Times 108(36):16–20
6. Murdoch J, Robinson M, Rossato M et al (2021) Use of NPWT as part of a Hospital@Nurse wound management service. Journal of Community Nursing 35(4):50–7
7. Orlov A, Gefen A (2022) The potential of a canister-based single-use negative pressure wound therapy system delivering a greater and continuous absolute pressure level lto facilitate better surgical wound care. IntWound J19(6):1471–93. https://doi.org/10.1111/iwj.13744
8. Othman D (2012) Negative pressure wound therapy literature review of efficacy, cost effectiveness, and impact on patients’ quality of life in chronic wound management and its implementation in the United Kingdom. Plast Surg Int 2012:374398. https://doi.org/10.1155%2F2012%2F374398
9. Rosen RD, Manna B. Wound Dehiscence. StatPearls Publishing
10. Sandy-Hodgetts K, Leslie GD, Parsons R (2017) Prevention of postsurgical wound dehiscence after abdominal surgery with NPWT: a multicentre randomised controlled trial protocol. JWound Care 26(2): S23–6. https:// doi.org/10.12968/jowc.2017.26.sup2.s23 Rosen RD, Manna B. Wound Dehiscence. StatPearls Publishing
11. World Union of Wound Healing Societies (WUWHS) Consensus Document. Surgical wound dehiscence: improving prevention and outcomes. Wounds International. https://tinyurl.com/mry8ae6t (accessed 3 September 2023)
12. Sandy-Hodgetts K, Leslie GD, Parsons R (2017) Prevention of postsurgical wound dehiscence after abdominal surgery with NPWT: a multicentre randomised controlled trial protocol. JWound Care 26(2): S23–6. https:// doi.org/10.12968/jowc.2017.26.sup2.s23
13. World Union of Wound Healing Societies (WUWHS) Consensus Document. Surgical wound dehiscence: improving prevention and outcomes. Wounds International. https://tinyurl.com/mry8ae6t (accessed 3 September 2023)
14. Zaver V, Kankanalu P (2023) Negative Pressure Wound Therapy. StatPearls Publishing
This article is excerpted from the Wounds UK | Vol 19 | No 3 | 2023 by Wound World.


