The development of diabetes-related foot ulceration (DFU) is often multifactorial, and usually associated with the trilogy of peripheral neuropathy resulting in foot deformity (McMorrow et al, 2022) peripheral arterial disease and susceptibility to infection as the main predisposing factors. The dorsal and plantar aspects are usually affected due to digital deformities, such as hammer, mallet or claw toes, and account for 43%-55% of all DFUs (Calvo-Wright et al, 2023). They tend to have a higher rate of amputation compared to other areas on the foot (Pickwell et al, 2013).
Toe deformities are usually caused by peripheral neuropathy resulting in atrophy of the intrinsic muscles of the foot. When these become dysfunctional and are overpowered by the extrinsic muscles of the foot (i.e. flexor digitorum longus and extensor digitorum longus), the stabilising action is lost, resulting in the claw or hammer toes (Bus et al, 2009).
In those with diabetic neuropathy, toe deformities can increase plantar pressures during midstance and toe off, resulting in callus formation and increased pressure, particularly at the apices of the toes (La Fontaine et al, 2014).
Offloading mechanical tissue stress has been identified as one of the most important interventions needed to heal DFUs. Orthotic interventions, such as silicone toe props/protectors and footwear modifications, are standard conservative treatment options, however the evidence around this is weak (Lázaro-Martínez et al, 2014). Surgical interventions such as flexor tenotomies (FTs) can be considered when conservative non-operative treatments have been unsuccessful (Finestone et al, 2018).
IWGDF offloading guidelines
The recent 2023 International Working Group on the Diabetic Foot (IWGDF, 2023) guidelines on offloading interventions to promote healing of foot ulcers support surgical offloading treatments. The evidence for digital tenotomy of the flexor tendon is strong with the desirable effects deemed to be moderate. The IWGDF recommends performing digital flexor tenotomies in individuals with diabetes and callus, or an ulcer on the apex or distal part of a non-rigid hammer toe to prevent development of ulceration or recurrent foot ulceration (Bus et al, 2020).
This is based on one randomised controlled trial and 13 non-controlled studies, which found that digital flexor tenotomies in combination with removable ankle-high offloading devices increased healing rates, sustained healing and reduced plantar pressure at ulcer sites in comparison to offloading devices alone. The undesirable effects include small increased risk of transfer lesions in most noncontrolled studies and little to no difference in balance and amputation rates. Interestingly, they judged that any additional resources and costs required are negligible or small, as tenotomy can be performed in an outpatient clinic, so is seen as a cost-effective intervention.
Clinical case
A 68-year-old female Afro-Caribbean patient who was retired and a non-smoker. She was independently mobile but relatively inactive due to her foot pathologies, which had started in 2017.
Her medical history included:
- Type 2 diabetes mellitus diagnosed in 1999
- Peripheral neuropathy
- Retinopathy
- Hypertension
- Hypercholesterolaemia
- Transient ischaemic attack in 2009
- Body Mass Index 28.
Her medication included:
- Amlodipine 10mg od
- Aspirin 75mg od
- Atorvastatin 80mg od
- Bisoprolol 1.25mg od
- Canagliflozin 300mg od
- Humalog Mix50
- Lansoprazole 30mg od
- Liraglutide 1.2 mg od
- Metformin SR 500mg bd.
In terms of her presenting foot complaints, in July 2017, she had left third toe ulceration and infection. In November 2017, she underwent left third toe emergency amputation with debridement of extensive skin and soft tissue on dorsum of foot to remove pus and de-vascularised tendons. In addition, she underwent 5 days of larvae therapy, then negative pressure wound therapy. Also in November 2017, a left angioplasty was performed:
posterior tibial and peroneal was undertaken with 3mm balloon, TP trunk with a 4mm balloon which provided significant improvement in both posterior tibial and peroneal flow.
In March 2018, the left dorsal foot wound healed but with significant scarring.
In May 2018, there were left hallux and second progressive toe deformities.
Between 2018-2020, there was recurrent ulceration with osteomyelitis to both left apex of the second toe and left hallux ulcerated which was treated with conservative offloading and antibiotics as per local guidelines. In July 2022, due to nonhealing, the person was referred to the podiatric surgery to review for surgical offloading.
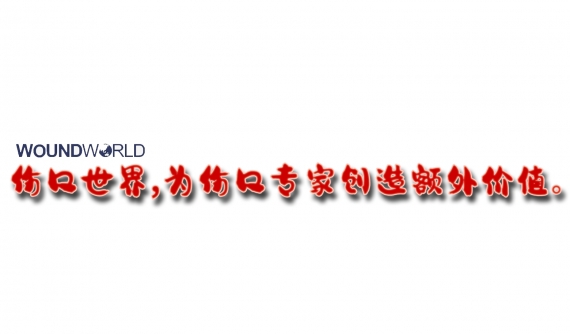
AP view and oblique view X-rays (Figures 1 and 2) show third toe amputation, second MTP degenerative joint disease and multiple toe deformities.
Vascular assessment left foot:
There was a history of angioplasty to the left limb, and the following features were non postangioplasty: pulses were non-palpable, with doppler signals for both dorsals pedis, and Posterior tibial monophaisic, and Anterior tibial multiphaisic (Biphasic). It was technically difficult to perform toe pressure due to alignment and poor apical tissue quality; however, it was not impossible. Left systolic toe pressure = 64mmHg.
Using the WIfI tool, the score was 1-0-1:
- Ulcer = 1 — small/shallow ulcer on distal leg or foot
- Gangrene = 0 — no gangrene
- Toe pressure = 64mmHg
- Foot Infection = 1 — local infection involving only skin and subcutaneous tissue
- WIfI Stage = 1
- Risk of amputation = Low risk
- Benefits of performing revascularisation = Low benefit.
Interestingly, if osteomyelitis recurred, the WIfI stage rises to stage 3, indicating a moderate risk of amputation.
Clinical assessment and treatment plan
The individual had experienced recurrent ulcerations despite conservative offloading and multiple courses of antibiotics over the preceding 5 years. Diabetes was poorly controlled with a HbA1c of 97mmol/ mol. At the time of the treatment, she presented with a left apical hallux ulcer with negative probe to bone test, pressure lesion to the hallux dorsomedial interphalangeal joint and second toe apical callus with remission of the ulcer (Figures 3 and 4). On clinical assessment of the toe deformities, there remained some flexibility despite the second metatarso-phalangeal joint being affected by degenerative joint disease. Claw toe deformities were noted to the fourth and fifth digits but there was no history of callus or ulceration.

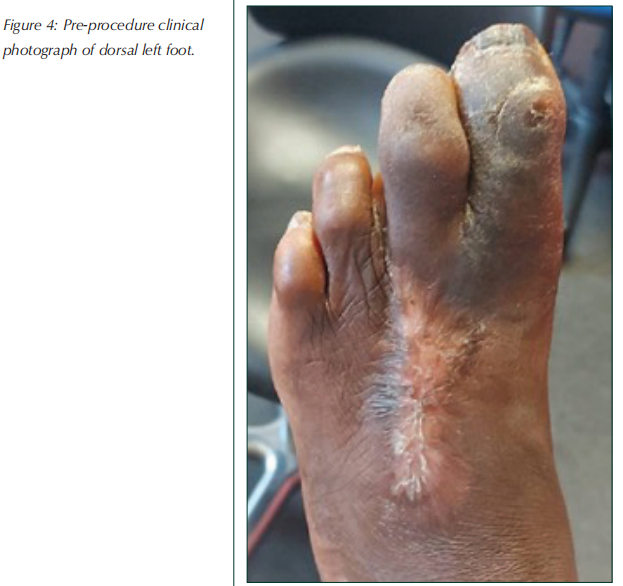
Surgical options were discussed including flexor tenotomies, digital arthroplasties and partial toe amputations. In view of the suboptimal diabetes control, history of revascularisation and previous scarring, it was decided to proceed with flexor tenotomies as the option carrying least risk, with the potential to proceed to formal surgery if this failed. The individual consented to the following risks: swelling, bleeding, infection, toe instability, transfer pressure lesions/ulcers, failure to heal the ulcer, need for further surgery, including amputation and reduced flexion/motion of the toes.
Left hallux and second toe flexor tenotomies were performed under local anaesthesia using an 18-gauge needle as an outpatient procedure. The needle was inserted at the bases of each toe, lateral to the flexor tendons. While applying tension to the tendon and using the sharp, bevelled edge of the needle, a sweeping motion back and forth was carried out to transect the longitudinal fibres of the tendons. Post-procedure, the toes were splinted in rectus alignment with appropriate dressings applied, and she was able to fully mobilise in a flat
Treatment timeline
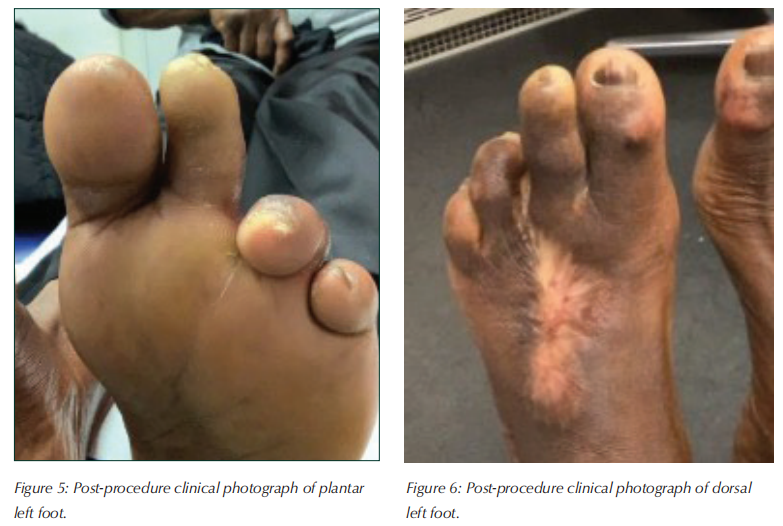
In August 2022, left hallux and second toe flexor tenotomies were performed. A month later, left hallux and second toe ulcers healed at 2 weeks post-procedure and the individual was back in her own footwear. In November 2022, no complications were reported, and ulcers remained healed. In June 2023, the individual’s digits remain healed with no transfer pressure lesions reported.
Following the tenotomies, the ulcer and callus resolved rapidly and had completely healed after 2 weeks demonstrating how powerful these procedures are in managing toe deformities and apical DFUs. The hallux dorso-medial interphalangeal joint lesion also resolved (Figures 5 and 6). postoperative shoe.
Discussion
Digital flexor tenotomy can be a successful intervention for people with toes deformities and recalcitrant lesser digital ulcers that fail conservative treatment. The presence of ischaemia or osteomyelitis should not be considered a contraindication for these procedures, however, there may be longer healing times and a higher risk of complications during follow up.
The cost of flexor tenotomies is relatively low when compared to the cost of ongoing dressing care, multiple antibiotics, and the potential for hospital admission for infection management. There is also the socio-economic cost to the individual to consider from lifestyle, employment and cardiovascular risk factor perspectives.
Conclusion
The flexor tenotomy is an effective, safe and minimally invasive procedure for the treatment and prevention of apical ulcers in individuals with toe deformity. With the 2023 IWGDF offloading guidelines advocating this valuable treatment option, we must consider how we can incorporate it into our treatment pathways to optimise patient care.
Reflective points and future research considerations
Could tenotomies be done prophylactically after digital amputation to prevent adjacent digital toe deformity and ulceration? Consideration should be given to this for each on a case-by-case basis. Should we be offering tenotomies to a broader range of patients with apical pressure lesions, recurrent ulcerations and those with apical osteomyelitis where the tenotomy can be performed with debridement of the osteomyelitis? Further research is needed to include those patients with non diabetes-related apical ulceration.
Should we consider tenotomising all digits to reduce the risk of transfer lesions? In this case, the fourth and fifth digits were clawed so appear vulnerable, but they did not proceed to develop callus/ulceration.
References
1. Bus SA, Maas M, Michels RP, Levi M (2009) Role of Intrinsic Muscle Atrophy in the Etiology of Claw Toe Deformity in Diabetic Neuropathy May Not Be as Straightforward as Widely Believed. Diabetes Care 32(6): 1063–7. doi: 10.2337/ dc08-2174
2. Bus SA, Lavery LA, Monteiro-Soares M et al, on behalf of the International Working Group on the Diabetic Foot (2020) Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update) Diabetes Metab Res Rev 36: e3269. doi: 10.1002/dmrr.3269
3. Calvo-Wright MM, López-Moral M, García-Álvarez Y et al (2023) Effectiveness of percutaneous flexor tenotomies for the prevention and management of toe-related diabetic foot ulcers: a systematic review. J Clin Med 12(8): 2835. doi: 10.3390/jcm12082835. PMID: 37109172; PMCID: PMC10142834
4. Finestone AS, Tamir E, Ron G et al (2018) Surgical offloading procedures for diabetic foot ulcers compared to best nonsurgical treatment: A study protocol for a randomized controlled trial. J Foot Ankle Res 11: 6. doi: 10.1186/s13047- 018-0248-3
5. International Working Group on the Diabetic Foot (2023) Guidelines of offloading foot ulcers In persons with diabetes IWGDF Update. Available at: https://iwgdfguidelines.org/ wp-content/uploads/2023/05/IWGDF-2023-06-Offloading Guideline.pdf (accessed 19.06.2023)
6. La Fontaine J, Lavery LA, Hunt NA, Murdoch DP (2014) The Role of Surgical Off-Loading to Prevent Recurrent Ulcerations. Int J Low Extrem Wounds 13(4): 320–34. doi: 10.1177/153473461455002
7. Lázaro-Martínez JL, Aragón-Sánchez J, Afonso FJA et al (2014) The Best Way to Reduce Reulcerations. Int J Low Extrem Wounds 13(4): 294–319. doi: 10.1177/1534734614549417
8. McMorrow R, Nube VL, Manski-Nankervis JA (2022) Preventing diabetes-related foot ulcers through early detection of peripheral neuropathy. Aust J Gen Pract 51(11): 833–8
9. Pickwell KM, Siersma VD, Kars M et al, on behalf of the Eurodiale consortium (2013) Diabetic foot disease: Impact of ulcer location on ulcer healing. Diabetes Metab Res Rev 29(5): 377–83. doi: 10.1002/dmrr.2400.
This article is excerpted from the 《The Diabetic Foot Journal Vol 26 No 1 2023》by Wound World.