It has been noted however that overuse of ineffective interventions and underuse of evidence-based treatments for wounds continues to occur in clinical practice (Gray et al, 2018). One of the reasons for this could be the plethora of dressing choices that healthcare professionals are faced with, from the ‘simplest’ to those offering more advanced treatments and everything in between, leading to confusion and difficulties with decision-making. As a result, dressing choice can be based on the perceived simplicity of use and on personal preference rather than evidence-based practice. This confusion and lack of evidence-based decision-making was highlighted by Guest et al (2020) in his work on the burden of wounds. Guest et al (2020) found that patients were prescribed a mean of eight different types of dressing, suggesting a lack of understanding about the mode of action of different dressings and how they should be used, which potentially leads to each healthcare professional choosing the most familiar dressing to them without a clear rationale.
Patients and their wounds often have multiple factors requiring consideration when choosing a wound dressing or treatment, presence of sloughy tissue, infection, exudate levels, delayed healing, size and depth of wound, atraumatic application and removal, comfort, ease of use, comorbidities and wear time. Given this, it should be of no surprise that health professionals may find it difficult to prioritise the various needs of the wound in order to choose a dressing that is going to ‘tick the most boxes’.
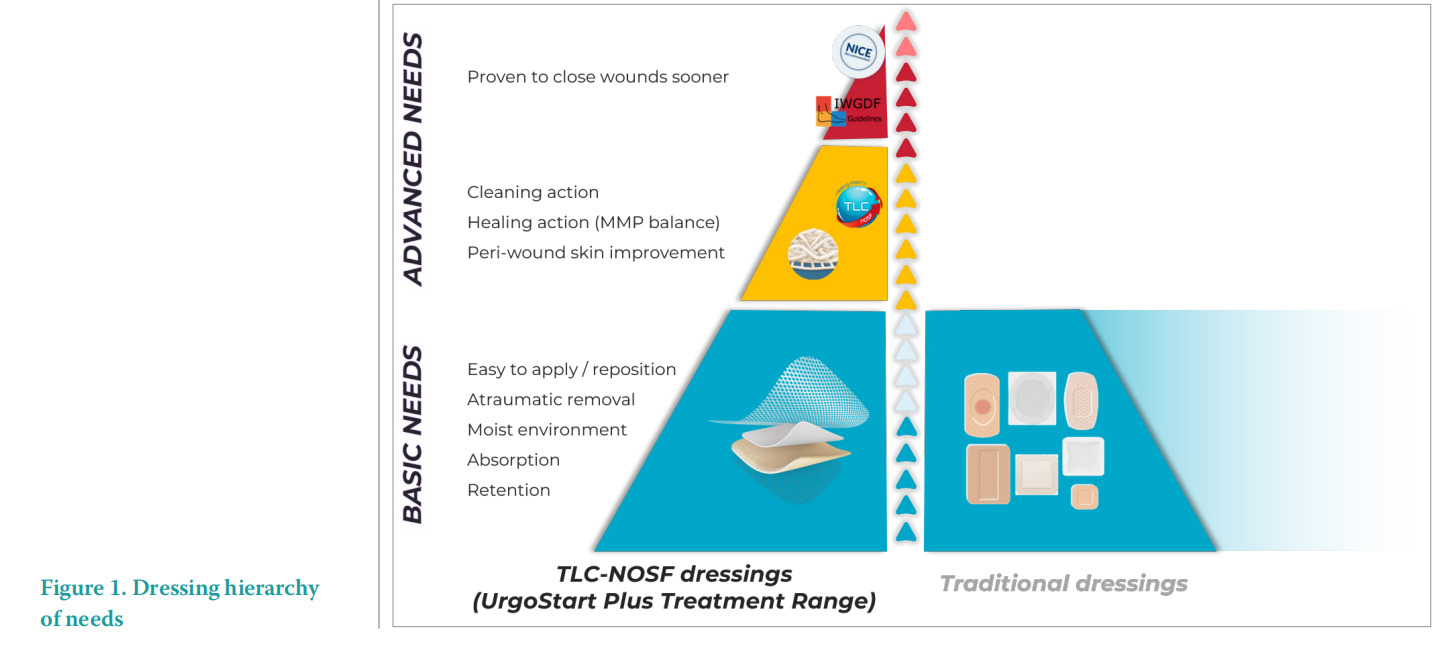
One approach for choosing wound dressings, offering structure and simplicity, could be using the same principles as the familiar Maslow’s Hierarchy of Needs, whereby society is theorised to have certain physiological and psychological needs that progress from basic to complex (Bogenhold, 2009). The discussion, originally around Maslow’s pyramid, was that each stage must be satisfied to motivate us to progress to achieving the next level i.e. the most basic needs must be met before higher-level needs can be achieved. However, there is the suggestion that the hierarchy does not need to be interpreted as rigidly as originally thought, with Maslow arguing that meeting higher needs leads to such factors as less disease, greater biological efficiency and better sleep and appetite (Bogenhold, 2009).
A similar hierarchy of needs is often applied by healthcare professionals to the patient and their wound when choosing a suitable dressing. Choice is initially guided by the basic needs relating to the symptoms of the wound and everyday needs of the patient, such as absorption, comfort, pain free application and removal and ease of use. These can generally be met by basic dressings, such as conventional foam dressings. Progression to more advanced needs would be where the wound requires debridement of sloughy and non-viable tissue supported by a suitable dressing technology, and sitting at the very top of the dressing pyramid would be products incorporating unique technologies, such as those that can rebalance the wound environment on a cellular level and promote wound closure more rapidly.
The difficulty with seeing dressing selection as a hierarchy is that the use of advanced technologies become reserved only for those patients considered to have the highest need, and reinforces the belief that unique wound treatments must be expensive, complicated, difficult to use and implement. However, while dressing selection should be based on a thorough holistic assessment of the patient and the wound, which identifies those at risk of non-healing, it doesn’t need to be a complex process. There are unique evidence-based wound treatments in existence that can meet multiple needs of patients and their wound in one simple dressing, incorporating the basic, advanced and unique features and benefits required (Figure 1). Just meeting the basic needs of the patient and the wound through automatically using the more familiar dressing such as foam or wound contact layer often means that patients are not receiving the most effective local treatment as guided by the clinical evidence. Robust clinical evidence identifies wound dressings that can actively promote faster wound healing and are particularly beneficial for those individuals at risk of delayed wound healing due to comorbidities National Institute for Health and Care Excellence (NICE, 2019).
Evidence-based care considers that decisionmaking should be based on the best available clinical evidence, expertise, the patient’s wishes and values and within the context of available resources (Dawes et al, 2005), and this can be applied to delivery of effective wound management. Every patient with a wound has the right to receive evidence-based care and opportunities to improve quality of life (QoL) through faster healing should not be missed due to familiarity with a particular less effective dressing.
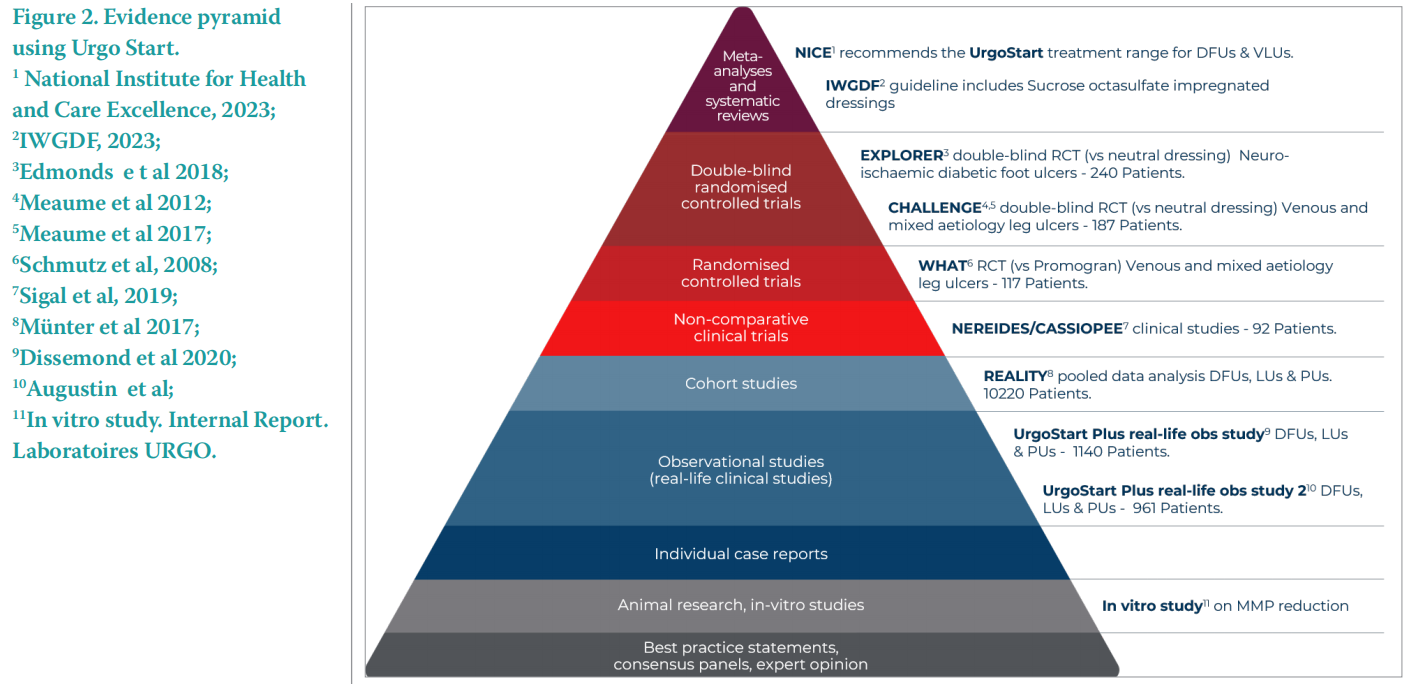
A readily available resource for healthcare professionals to use when choosing evidencebased treatments is guidance from NICE. This guidance can take several forms, one of which is the Medical Technology Guidance (MTG) whereby a ‘case for adoption’ for a specific technology is independently considered by NICE based on the strength of the available evidence and expert advice. If the technology is considered to offer advantages to patients and the NHS over current management options, then the case for adoption is supported at a national level.
The UrgoStart Plus Treatment Range is one of only a few wound management products to receive NICE MTG (NICE, 2019), and one of very few where there is a recommended case for adoption. The UrgoStart Plus Treatment Range uses a compound called Nano-Oligosaccharide Factor (NOSF), which has been shown to decrease the activity and number of matrix metalloproteinases (MMPs), enzymes that have been found to be present in too high a number in complex wounds, contributing to delayed wound healing and wound breakdown (Ren et al, 2014). In the UrgoStart Plus Treatment Range, NOSF is combined with the TLC (Technology Lipidocolloid) found within all Urgo dressings that provides a moist wound healing environment and prevents dressing adherence, promoting pain-free dressing changes. The UrgoStart Plus Pad and UrgoStart Plus Border dressings within the range, also contain polyabsorbent fibres which deslough and continuously clean the wound bed.
The strength of the evidence available for the UrgoStart Plus Treatment Range was such that NICE was able to make a recommendation for the use of the UrgoStart Plus Treatment Range to treat diabetic foot ulcers (DFU) and venous leg ulcers (VLU) within an appropriate diagnostic and treatment pathway across both acute and primary care. Alongside the considerable evidence base (Figure. 2), an independent cost analysis performed by NICE found the product to be cost-effective due to its ability to heal these wound types more quickly than conventional dressings. With faster wound healing, the UrgoStart Plus Treatment Range also improves patient outcomes and QoL (NICE, 2019). NICE independently reviewed the latest clinical evidence in April 2023 and renewed their recommendation.
The other benefit identified by NICE while collaborating with NHS staff that had experience of using the UrgoStart Plus Treatment Range to produce the MTG was around ease of use. This challenges the perception that advanced technologies and treatments are expensive, complicated, and difficult to use, and thus reserved for those patients considered to have the highest need or only for use by specialist clinicians.
While recognising that healthcare professionals will always have an individual responsibility for making appropriate treatment decisions in conjunction with the patient and/or their family or carers. Under the NHS Constitution patients have the right to clinically appropriate treatments, which NICE approves for use in the NHS. Therefore, it is expected that NICE guidance is considered and implemented appropriately with the support of local service providers and commissioners (NICE, 2019).
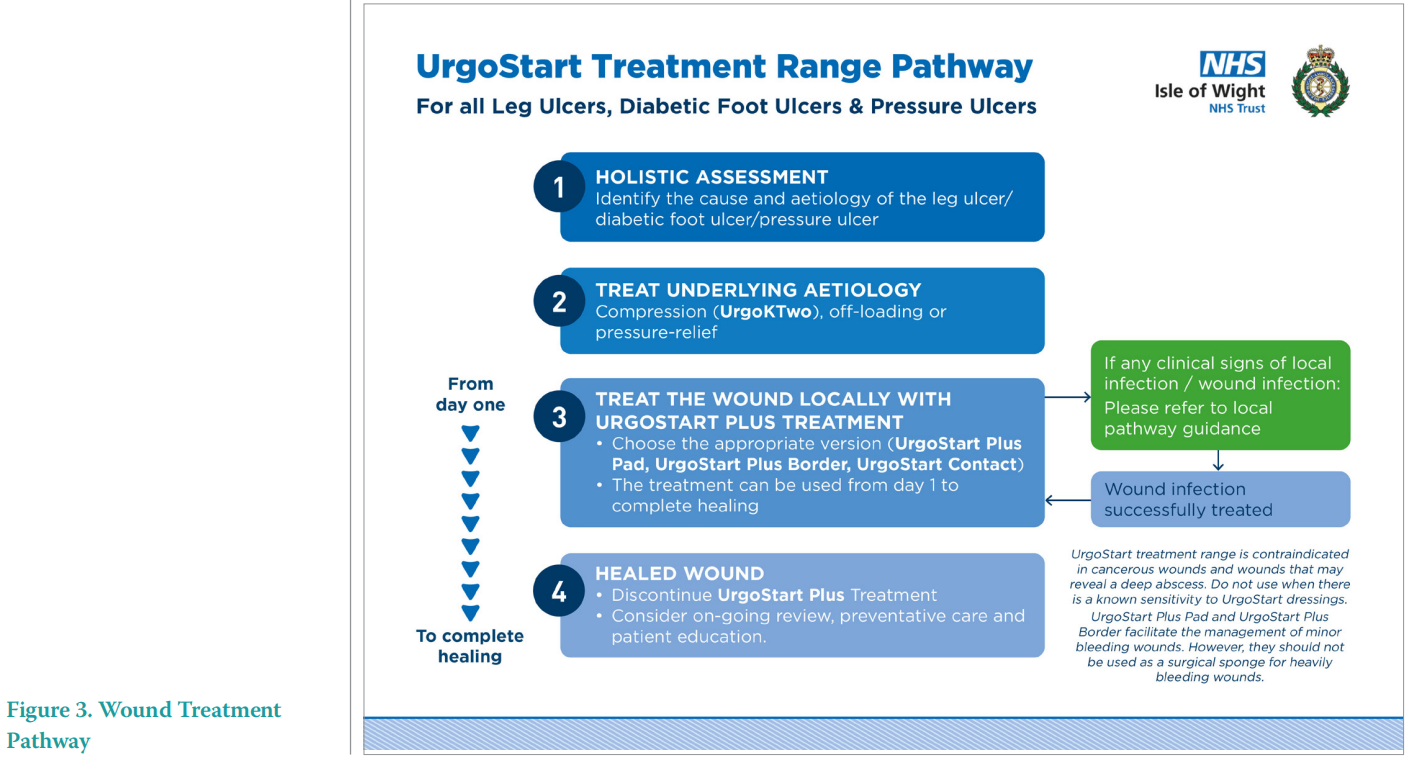
This expectation for incorporation of NICE guidance, and thus provision of access for patients to evidence-based care and treatments, was successfully recognised and demonstrated by Tickle (2021). Realworld outcomes associated with the implementation and evaluation of a standardised evidence-based treatment pathway incorporating the UrgoStart Plus Treatment Range into a new NHS wound healing clinic were published previously (Tickle, 2021). Results included improved patient outcomes in terms of timely wound healing, reduction in pain and improved QoL, and associated positive economic outcomes with reduced variation in care provision. The pathway implementation was found to be easy and usable by a range of staff supported by appropriate training, and improved knowledge and confidence around clinical decision-making.
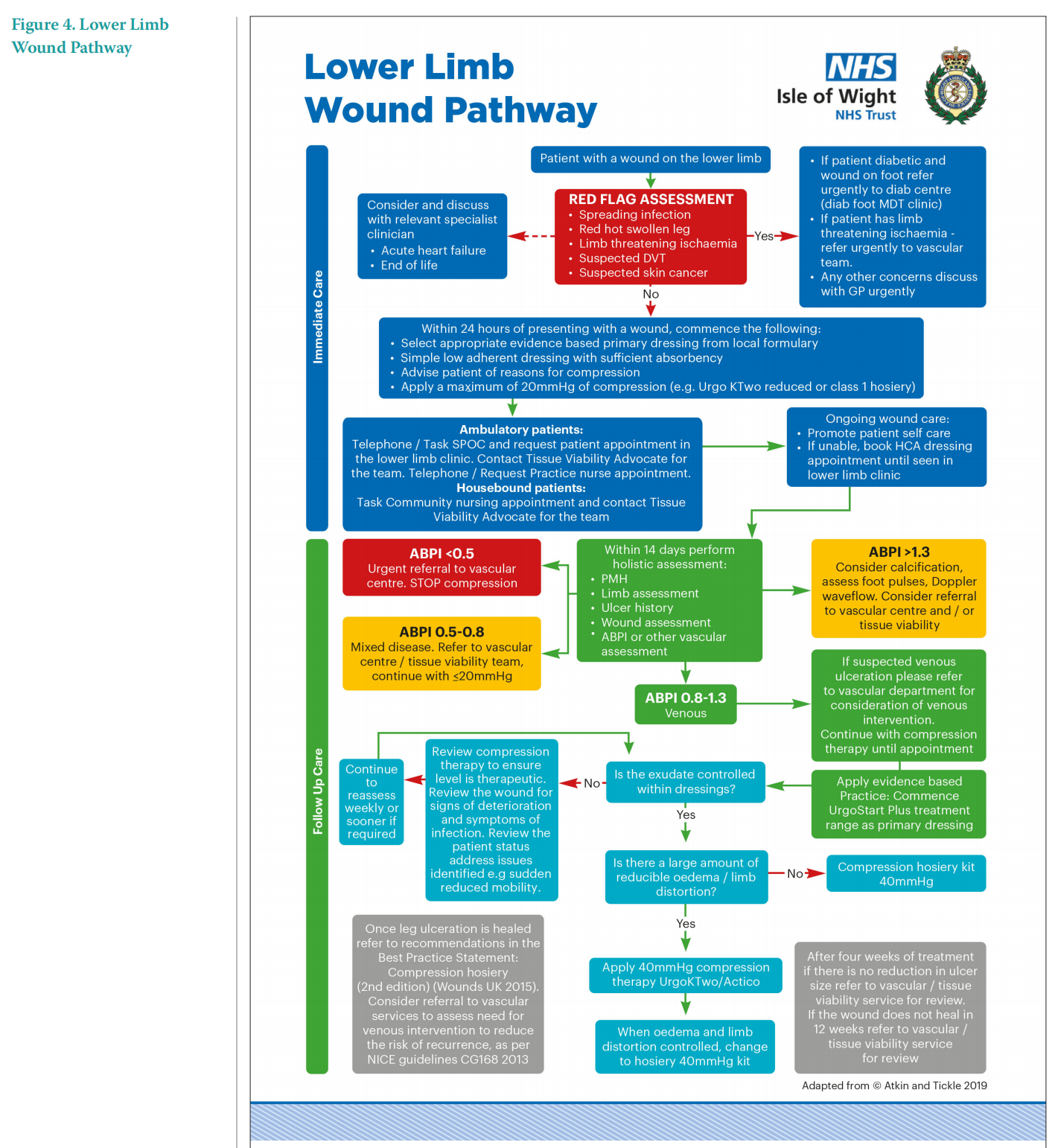
Due to the successful outcomes achieved previously with the implementation of NICE guidance and an evidence-based treatment pathway, the author chose to repeat the process when moving to a different NHS trust in another part of the UK. The simplicity of the local wound treatment pathway and lower limb wound pathway incorporating the NICE guidance for use of the UrgoStart Plus Treatment Range (Figures 3–4) meant that the implementation was easily transferable to another clinical setting and enabled the continued achievement of improved patient outcomes. Some of these outcomes are demonstrated in the following series of case studies performed while implementing the treatment pathway in the new setting. As health professionals confidence in the clinical effectiveness of the UrgoStart Plus Treatment Range was already established due to previous positive experiences, this evaluation focused on use of the dressing and pathway in a wider variety of complex wound aetiologies and focusing on the impact on the patient, their individual circumstances and their QoL across social, emotional, functional and psychological domains.
CASE STUDIES
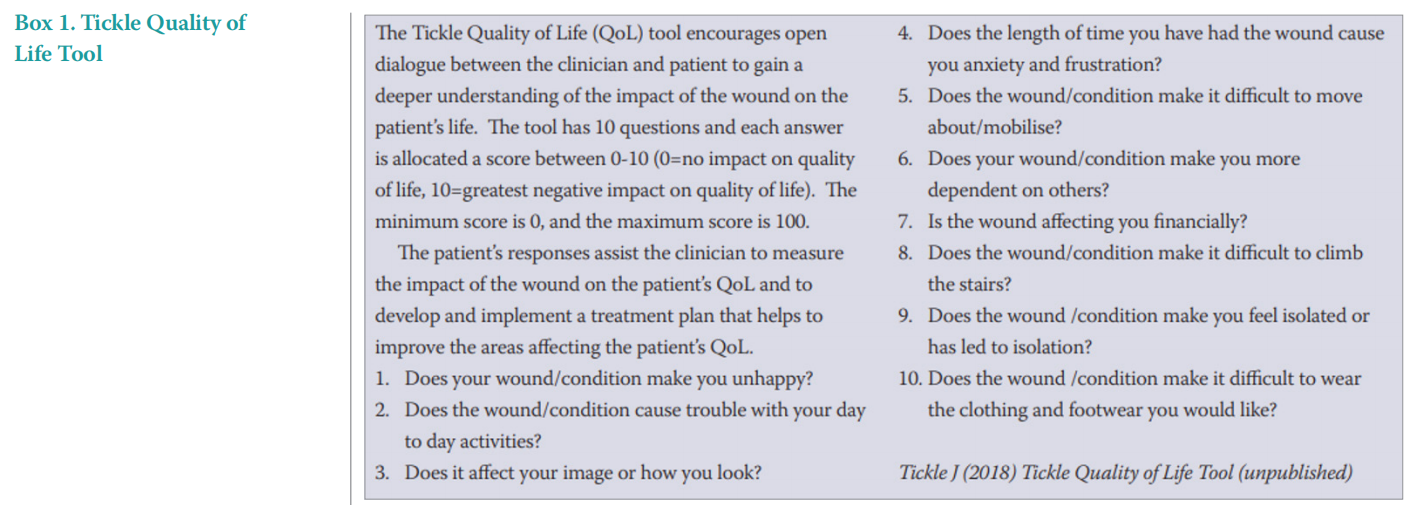
UrgoStart Plus and UrgoStart Plus Border were used as a simple primary treatment for all wounds in conjunction with appropriate standard of care, such as compression therapy, offloading and pressure relief as outlined in the evidence-based treatment pathway being used. Pain scores were measured at baseline and end of the treatment using a Visual Analogue Scale (VAS) from 0–10. QoL was measured at start and end of treatment using the Tickle Quality of Life Tool (Tickle 2021; Box 1), which is measured out of 100 and where the higher the overall score, the greater the negative impact on QoL.
Case study 1. A leg ulcer
Mrs A is a 71-year-old female with a history of rheumatoid arthritis and hyperlipidaemia being managed with non-steroidal anti-inflammatory drugs (NSAIDs) and atorvastatin.
Mrs A had a leg ulcer of four years duration measuring 9x6cm (Figure 5A), which was managed with many different types of topical treatments and had required multiple courses of oral antibiotic therapy for recurrent local wound infection. This was a cause for concern clinically with a view to antimicrobial therapy stewardship in an era of increasing antibiotic resistance. The patient had been prescribed a short stretch bandage twice before but failed to tolerate treatment and unfortunately it did not appear that any other alternative was suggested.
The wound was causing severe pain, rated as 8/10 VAS. The recorded QoL score was 45/100 and this was due to multiple factors where the wound was impacting on QoL. The patient was experiencing significant stress and anxiety, leading to sleep deprivation and loss of appetite, all of which can potentially adversely affect wound healing (Gouin and Kiecolt-Glaser, 2012). While Mrs A was now retired, she had previously been working while living with the leg ulcer and was still mindful of the impact the wound had had on this part of her life. She expressed feelings of embarrassment when she’d been at work and at home due to recurrent infections, malodour and leakage from the wound, this was affecting her relationship with her husband and had also impacted previously on her work and financial status due to having to take time off for appointments and associated reduction in salary. All this had left the patient feeling a loss of importance as a person and unable to enjoy a social life and go on holidays with her family. She expressed:
'I just want to be a wife and a mother, I want to be normal'
Following tissue viability review, Mrs A was commenced on UrgoStart Plus Pad to restart the wound healing process and ultimately improve QoL UrgoStart Plus Pad was used in conjunction with standard of care, including regular cleansing, debridement and compression therapy with UrgoKTwo Reduced (20mmHg; Urgo Medical) compression bandaging. Reduced compression was discussed with the patient and selected due to the patient’s rheumatoid arthritis and previous difficulty with tolerating compression due to pain.
After 16 weeks of optimising both the local treatment along with compression therapy with UrgoStart Plus Pad and UrgoKTwo Reduced bandage system oedema reduced to the lower limb and exudate levels were decreased and limb shape improved, allowing for a change of compression therapy to Class 1 hosiery to support self-care (Figure 5B).
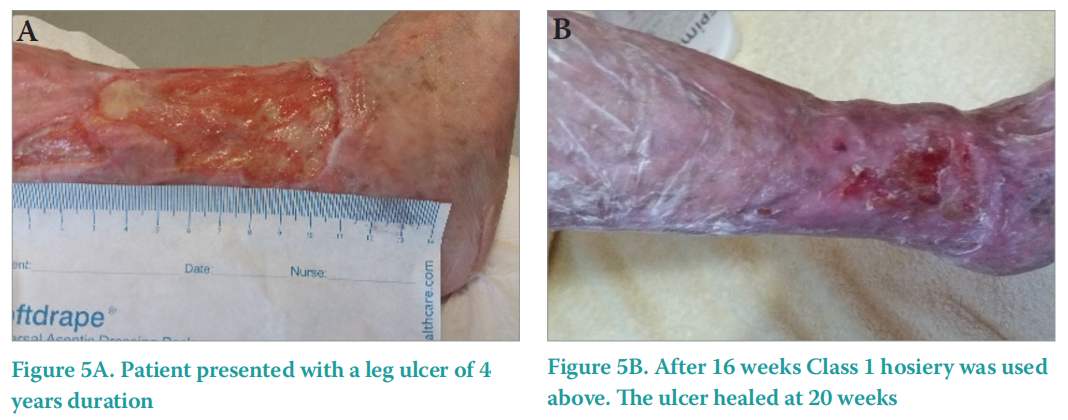
The wound was completely healed after 20 weeks, with no reported pain and a QoL score of 0.
Case study 2. A diabetic foot ulcer
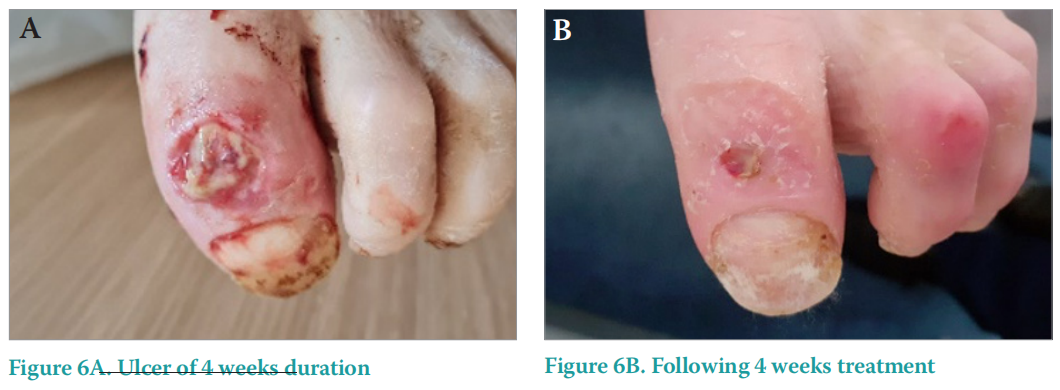
Mr B is a 93-year-old man with a past medical history of diabetes, vitamin B12 deficiency anaemia, rectal cancer and diverticulitis, he was living in a residential care home. His medical conditions were being treated with various medications. He presented to the tissue viability service with a DFU to his toe of 4 weeks duration measuring 3x2cm (Figure 6A). It had been managed with multiple antimicrobial dressings and courses of antibiotics, which had impacted on his health further, causing nausea and diarrhoea. He was wearing an offloading boot, but despite this standard of care being in place and the ulcer being small in size, it was deemed at high risk of nonhealing due to Mr B’s age, comorbidities and effects of polypharmacy.
The wound was also negatively impacting his QoL across multiple domains, recording a QoL score of 20/100. He was experiencing fear and anxiety over the potential loss of his toe or even limb, and the malodor from the wound was making him uncomfortable when being visited by family and friends, and while around his fellow residents. Pain was recorded as 4/10 and was affecting his sleep due to discomfort at night from the weight of bedclothes on his foot and when repositioning in bed. Mr B was finding it increasingly difficult to attend his DFU clinic appointments and was also feeling a financial impact due to requiring costly taxis to the specialist clinic.
The decision was made to treat the wound with UrgoStart Plus Pad as recommended by NICE (2019) as a primary dressing to promote healing of this high risk DFU, alongside continuation of standard of care with regular cleansing, debridement and offloading.
Following four weeks of treatment, a clear improvement was seen in the wound size and condition (Figure 6B) and QoL and pain scores had both reduced to 0. This progress was hugely reassuring to the patient, carers and clinicians. Regular DFU clinic appointments were no longer required as the district nursing team were more confident to undertake shared care. Furthermore, Mr B was experiencing improved sleep quality due to pain reduction, and overall anxiety levels were significantly better. UrgoStart Plus Pad was continued through to complete healing.
Case study 3. A postoperatively abdominal wound
Mrs C is a 58-year-old female with a past medical history of hypertension and diverticulitis that was managed with Bisoprolol, Spironolactone and protein supplements. She had been admitted to hospital with a bowel obstruction that had required surgical intervention. Abdominal wound dehiscence was reported due to a surgical site infection (SSI), five days after surgery. It was treated with appropriate antibiotics. Postoperatively dressings were causing pain and discomfort on removal.
A referral was made to the Tissue Viability Service 10 days postoperatively (Figure 7A) as the wound was failing to reduce in size and there was continued risk of infection due to the type of surgery and that she was nutritionally compromised. Discharge was also being delayed due to the wound dehiscence and subsequent complications. On review the wound measured 6x4cm, the wound bed was sloughy, and there were moderate levels of haemopurulent exudate. The periwound skin was dry and irritated causing some discomfort. Pain was recorded as 6/10 overall, but this increased to 8/10 at dressing change. Mrs C worked as a healthcare assistant in a Nursing Home, and the delayed discharge and wound concerns were causing her increased anxiety about loss of income, and that she was also unable to perform her normal supportive role for her daughter providing care for her two grandchildren. Her QoL score was recorded as 25.
Due to the risks associated with prolonged healing and infection and the pain being experienced, Mrs C was started on UrgoStart Plus Border dressings to reduce MMPs, absorb exudate and promote wound healing as quickly as possible and thus improve QoL. Following 10 days of treatment with UrgoStart Plus Border the wound bed was clean of any slough, granulating and exudate was minimal (Figure 7B). Furthermore her pain score had reduced to 2/10. Due to the simplicity and ease of use of the dressings with atraumatic dressing changes, Mrs C was able to be seamlessly discharged at this point to continue the same treatment regimen at home (Figure 7C). The improvement in the wound and wound pain was significantly reducing the stress and anxiety experienced by the patient, reflected in an improved QoL score of 10.
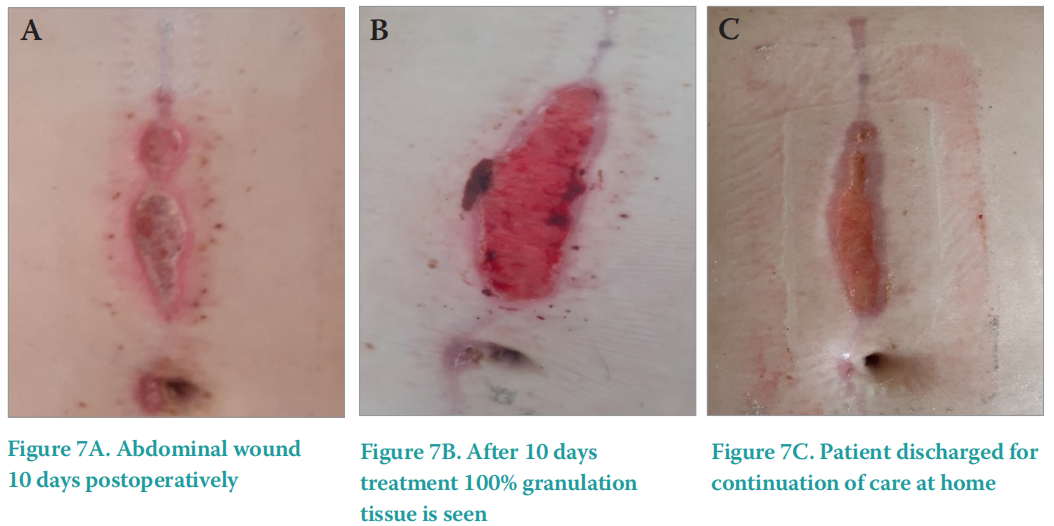
Complete wound healing was achieved after 3 weeks of treatment with UrgoStart Plus Border much to Mrs C’s delight as she was able to plan her return to work and resume her important family role.
Case study 4. A pressure ulcer
Mrs D is a 78-year-old female with a past medical history of rheumatoid arthritis, iron deficiency anaemia, depression and peripheral vascular disease. Concomitant medications for these conditions included buprenorphine patches, methylprednisolone injections and venlafaxine. Mrs D was referred to the Tissue Viability Service by the district nursing team with a non-healing pressure ulcer (PU) to the malleolus of 10 weeks duration and measuring 4x4cm (Figure 8A). The PU was caused by pressure from footwear. Previous wound dressings included silver and honey-based antimicrobial dressings and hydrocolloid dressings.
Risks of continued non-healing and potential infection were identified due to the patient having rheumatoid arthritis and being on steroid treatment, and also due to peripheral vascular disease that was unsuitable for revascularisation. The wound was causing significant pain, with a recorded pain score of 8/10. The impact on QoL across various domains was also recorded.The delayed healing was exacerbating her levels of anxiety as Mrs D was concerned that due to her poor arterial blood supply, the wound would deteriorate and lead to her losing her limb. The location of the PU was also causing difficulty with wearing of her specialist orthotic footwear, contributing to increased pain and impacting on her ability to mobilise fully. This led to an increased reliance on her husband and carers to assist with activities of daily living, causing feelings of a loss of independence and an overall negative impact upon her QoL. She was increasingly frustrated with the length of time she was having to live with the wound and was experiencing loss of sleep as she did not find the pressure-relieving mattress on her bed very comfortable. Mrs D also expressed anxiety with waiting for the district nurse as the time of their visits varied and she was reluctant to invite friends or family to her home on these days due to embarrassment of the wound. The reported QoL score was 50.
On examination of the wound bed consisted of 100% sloughy tissue, with low exudate levels and fragile but intact surrounding skin. UrgoStart Plus Pad was started as the primary dressing treatment to clean the sloughy tissue and stimulate the wound healing process by reducing the level of MMP’s in a complex and chronic wound. This was used in conjunction with the existing pressure relieving devices as established standard of care.
After three weeks treatment with UrgoStart Plus Pad, the slough had been completely debrided and the wound consisted of mostly epithelial and some granulation tissue with an associated decrease in wound size (Figure 8B). The recorded pain score had reduced to 2/10 and QoL score improved to 10 due to the reassuring visible progress of the wound, which was reducing associated stress and anxiety.
The wound healed completely after four weeks with the UrgoStart Plus Pad used through to complete re-epithelialisation. Mrs D was extremely pleased with the excellent and timely improvement and with the noticeable reduction in the discomfort experienced both when the dressing was in place and during dressing changes. She stated:
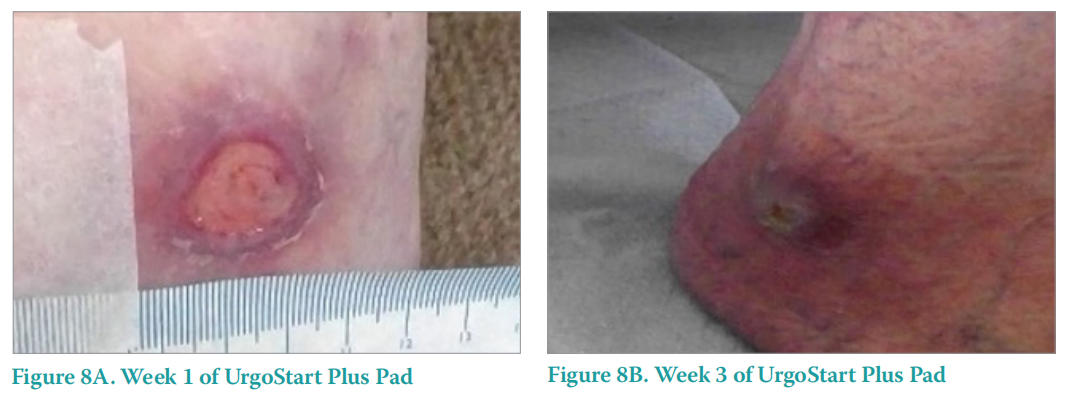
'I am so pleased that the wound has healed and that I no longer need the input of the district nurses. They are a lovely team, but it is good to get my life back to normal’
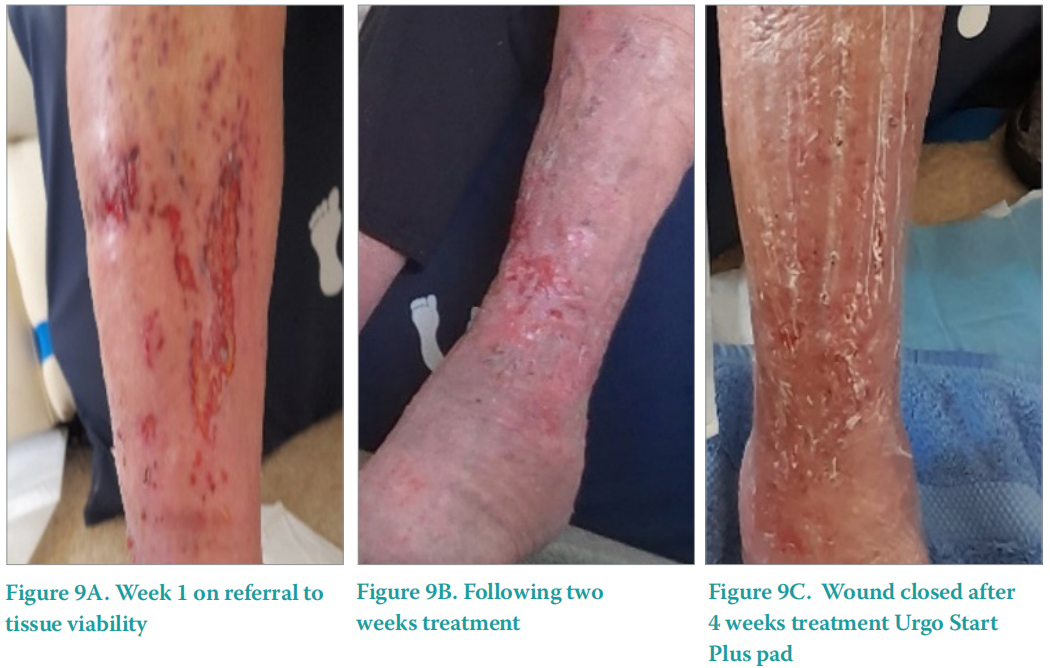
Case study 5. A traumatic lower limb wound
Mrs E is a 72-year-old female with a past medical history of a cerebral vascular accident and hyperlipidaemia being treated with simvastatin. She experienced a traumatic injury to her lower limb while gardening (Figure 9A), which had been managed with twice weekly dressing changes by the Practice Nurse for six weeks. Following holistic assessment Mrs E had been started on UrgoKTwo reduced (20mmHg) compression bandaging to manage any underlying venous insufficiency and oedema that may have been contributing to the delayed healing. Previous dressings used included alginate dressings, hydrogel and iodine-based dressings, but due to no visible improvement she was referred to the Tissue Viability Service.
On review, the wound bed consisted of 70% granulation tissue and 30% slough but was static and failing to reduce in size despite the presence of granulating tissue. Exudate levels were moderate with irritable and dry surrounding skin, and pain was an issue, with a recorded pain score of 7/10. Mrs E was normally a very independent lady who enjoyed dancing and gardening, and she was now extremely distressed with having a non-healing wound. She was unable to attend her dance classes or spend time in her garden, which was leaving her feeling frustrated and socially isolated. She was also having to rely on her husband to drive her to her twice weekly clinic appointments, which was making them both irritable. QoL score on initial assessment was 40.
UrgoStart Plus Pad was started as the primary dressing as it was suspected there were elevated levels of MMP’s due to the length of time the wound was present despite optimising standard care with compression therapy and the presence of underlying comorbidities. Normal saline was used for cleansing the wound and an emollient used to treat the surrounding skin, with continuation of the UrgoKTwo reduced compression bandaging.
After three weeks of twice weekly dressing changes with UrgoStart Plus Pad, the wound was considerably improved (Figure 9B) and reduced in size, providing reassurance to Mrs E and reducing her feelings of stress and anxiety. Complete wound closure was achieved after four weeks (Figure 9C), with both pain and QoL scores being recorded as 0. She was able to resume her independent lifestyle, restarting her gardening and dancing activities, and also freeing up her husband’s time too which restored the normal balance in their relationship.
CONCLUSION
These real-life case studies demonstrate that including UrgoStart Plus Treatment Range within easy to use evidence-based clinical pathways can support patients with multiple comorbidities to heal sooner. Complete healing was achieved for all the patients within these case studies by optimising the local wound conditions and reducing MMP’s. All patients had a positive experience with associated improvements in wound pain and overall quality of life, using just one type of dressing from the start to the end of the healing process.
For all of the patients presented, many different dressings had been tried unsuccessfully with limited rationale for dressing choice before the patient began the treatment pathway, leading to longer wound durations, increased complexity and a growing negative impact on QoL.
Starting the patient, following the first assessment, on an appropriate and standardised pathway using an effective evidence-based but simple dressing regimen, ensures the multiple needs of the patient can be met. These include factors that may concern the patient for example containment of exudate, pain free dressing changes and comfort when wearing the dressing. In addition, patients reported a reduced impact on their daily lives and improved physical, psychological and emotional wellbeing due to healing at the earliest opportunity.
The rigour of NICE guidance development supports lead clinicians in reviewing the available clinical evidence regarding the UrgoStart treatment range and helps them to build confidence in the recommendations, supporting implementation locally. Robust clinical evidence can be easily translated into local pathways of care and clinical practice without the need for extensive literature review by individual clinicians. Healthcare professionals of all skills and abilities are able to ensure safe and effective care as well as reducing healing time which benefits the patient’s QoL and is cost effective for the organisation.
REFERENCES
1. Augustin M, Keuthage W, Lobmann R et al (2021) Clinical evaluation of UrgoStart Plus dressings in real-life conditions: results of a prospective multicentre study on 961 patients. J Wound Care 30(12):966–78. https://doi.org/10.12968/jowc.2021.30.12.966
2. Bogenhold D (2009) Maslow’s Hierarchy of Needs. Chapter: The Encyclopedia of Business in Today's World. Sage
3. Dawes M, Summerskill W, Glasziou P et al (2005) Sicily statement on evidence-based practice. BMC Med Educ 5(1):1–7. https://doi. org/10.1186/1472-6920-5-1
4. Dowsett C, Hall Y (2019) T.I.M.E to improve patient outcomes: optimising wound care through a clinical decision support tool Br J Nurs 28 (6): S17–21. https://doi.org/10.12968/bjon.2019.28.6.s17
5. Dissemond J, Lützkendorf S, Dietlein M et al (2020) Clinical evaluation of polyabsorbent TLC-NOSF dressings on chronic wounds: a prospective, observational, multicentre study of 1140 patients. J Wound Care 29(6):350–61. https://doi.org/10.12968/ jowc.2020.29.6.350. PMID: 32530781.
6. Edmonds M, Lázaro-Martínez JL, Alfayate-García JM et al (2018) Sucrose octasulfate dressing versus control dressing in patients with neuroischaemic diabetic foot ulcers (Explorer): an international, multicentre, double-blind, randomised, controlled trial. Lancet Diabetes Endocrinol 6(3):186–96. https://doi.org/10.1016/s2213- 8587(17)30438-2
7. Gouin J-P, Kiecolt-Glaser JK (2012) The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am 31(1):81–93. https://doi.org/10.1016%2Fj.iac.2010.09.010
8. Gray TA, Rhodes S Atkinson RA et al (2018) Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 8(3):e019440. https://doi.org/10.1136/bmjopen-2017-019440.
9. Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 10(12):e045253. https://doi. org/10.1136/bmjopen-2020-045253
10. IWGDF (2023)Guidelines on the prevention and management of diabetic foot disease – 2023. https://iwgdfguidelines.org/guidelines-2023/ (accessed 10 June 2023)
11. Meaume S, Truchetet F, Cambazard F et al (2012) A randomized, controlled, double-blind prospective trial with a Lipido-Colloid Technology-Nano-OligoSaccharide Factor wound dressing in the local management of venous leg ulcers. Wound Repair Regen 20(4):500–11. https://doi.org/10.1111/j.1524-475x.2012.00797.x
12. Meaume S, Dompmartin A, Lazareth I et al (2017) Quality of life in patients with leg ulcers: results from CHALLENGE, a double-blind randomized controlled trial. J Wound Care 26 (7): 368–79. https://doi. org/10.12968/jowc.2017.26.7.368
13. Münter KC, Meaume S, Augustin M et al (2017) The reality of routine practice: a pooled data analysis on chronic wounds treated with TLCNOSF wound dressings. J Wound Care 26 (Sup2): S4–15. https://doi. org/10.12968/jowc.2017.26.sup2.s4 .Erratum in: J Wound Care (2017) 26(3):153
14. National Institute for Health and Care Excellence (NICE; 2019) UrgoStart for treating diabetic foot ulcers and leg ulcers MTG 42 https://tinyurl.com/pfy9skw4 (accessed 23 May 2023)
15. Ren Y, Gu G, Yao M, Driver VR (2014) Role of matrix metalloproteinases in chronic wound healing: diagnostic and therapeutic implications. Chin Med J (Engl) 127(8):1572–81
16. Schmutz JL, Meaume S, Fays Set al (2008) Evaluation of the nanooligosaccharide factor lipido-colloid matrix in the local management of venous leg ulcers : results of a randomised, controlled trial. Int Wound J 5:172–82. https://doi.org/10.1111/j.1742-481x.2008.00453.x
17. Sigal ML, Addala A, Maillard H et al (2019)Clinical evaluation of a new TLC-NOSF dressing with poly-absorbent fibers for the local management of exuding leg ulcers, at the different stages of the healing process: Results from two multicentric, single-arm, prospective, open-label clinical trials. J Wound Care 28(3):164–75. https://doi. org/10.12968/jowc.2019.28.3.164
18. Tickle J (2021) NICE guidance in real life: Implementation of an evidencebased care pathway within a new wound healing clinic. Wounds UK 17(3): 72–9. https://tinyurl.com/5dt737kv
This article is excerpted from the Wounds UK | Vol 19 | No 2 | 2023 by Wound World.


