In the literature, we often encounter the term “hard-to-heal” to define a wound that does not tend to heal within the expected timeframe, despite treatment with standard of care. We prefer to define this condition as stagnant; in our opinion, both of these definitions provide us with the exact situation of lesions that, despite adequate therapy, do not progress in the healing process. These types of stagnant lesions not only show no improvement, but also make it difficult to understand the causes of the poor progression towards healing, since wound healing is a highly complex process that involves multiple cell types whose nonlinear interactions have yet to be properly understood.
The healing rate of venous ulcers, the most common aetiology of chronic wounds, is 65% in 24 weeks, and 20% of ulcers do not heal after more than 50 weeks of standard therapy (Troxler et al, 2006). Therefore, the search for new therapies capable of reactivating the healing process of silent stagnant wounds, which do not respond to standard therapies, should be a medical priority.
Methods
A class IIa medical device manufactured by Emoled Srl (Florence, Italy) was used for photobiomodulation therapy. The device uses LED sources that emit blue light in the 410– 430nm wavelength range, with a power density of 120mW/cm2 . The optical system allows for homogeneous and controlled light emission over a surface area of approximately 20 cm 2 . For larger wounds, the user will need to make several successive applications; the number of applications needed to complete the treatment of a wound is automatically calculated by the device after switching on and entering the approximate size of the wound surface.
The treatment distance must be 4cm (±1cm) from the wound and the device is only activated when placed at the correct distance. An indicator on the screen during application helps the user to identify and maintain the correct positioning. The duration of the single application (60 seconds or 120 seconds) is pre-set.
As there is a consensus in medical practice that if an ulcer does not heal sufficiently after 4weeks of standard care, the treatment schedule should be reassessed, we have decided to treat patients for 4weeks with blue light photobiomodulation in addition to standard of care to assess blue light contribution to the reactivation of healing of stagnant ulcers.
The chosen protocol was two treatments per week lasting 60 or 120 seconds, depending on the aetiology of the wound. The progression of wound healing was assessed through a reduction in wound area, the wound bed score (Falanga et al, 2006; Schultz et al, 2003) and pain reduction. Pain intensity was recorded for each patient through the use of a visual analogue scale (VAS). Data were collected on each medical check-up.
Cases
Five patients were selected, three men and two women, with an average age of 69.4 years, who had been treated for some time at the Wound Care Outpatient Clinic, Hyperbaric Medicine Service, UOC Anaesthesia and Reanimation, Misericordia Hospital Grosseto, Italy.
The patients had ulcers of various aetiologies with a mean duration of 20.8 months and significant pain symptoms. All patients had already undergone various therapies and showed no signs of improvement. The five cases were selected because they were of clinical interest for the history of the patients and the initial conditions of the lesions.
Case 1
A 51-year-old man, in good general health, presented with an osteomyelitis lesion on the anterior middle third of the leg [Figure 1]. The skin lesion developed following a minorsports injury and had a periodic pattern. The lesion had been present for 18 months and showed exposure of the tibial plateau, medium levels of exudate, firm and calloused rolled borders, perilesional skin with erythema and hemosiderin deposits. sports injury and had a periodic pattern. The lesion had been present for 18 months and showed exposure of the tibial plateau, medium levels of exudate, firm and calloused rolled borders, perilesional skin with erythema and hemosiderin deposits.

The lesion was initially treated with a cycle of hyperbaric oxygen therapy in combination with antibiotic therapy for the treatment of osteomyelitis, as well as collagen dressing twice a week combined with platelet gel application once a week. Subsequently, compression bandaging and homologous skin grafting were performed, followed by 3weeks of negative pressure therapy.
No significant signs of improvement were seen. Therefore, the patient was selected for 60 seconds of blue light therapy on the entire surface of the lesion twice a week, in combination with a collagen-based dressing.
Case 2
An 82-year-old woman with rheumatoid arthritis presented with an 8-month perimalleolar vasculitis lesion on the inside of the lower third of her leg [Figure 2]. The lesion had a nonhomogeneous appearance, fibrin, medium levels of exudate, irregular inflamed borders, and erythematous perilesional skin with areas of skin atrophy, associated with severe pain.

An exudate-transfer foam primary dressing and a hydrofibre secondary dressing were used on the patient. Moderate compression bandaging and 120 seconds of blue light treatment were applied over the entire wound surface three times a week for the first 2weeks, and twice a week for the second 2weeks of treatment.
Case 3
A 73-year-old woman presented with a 4-year infected lesion on the posterior middle and lower third of the leg[Figure 3]. Following critical ischaemia of the lower limb, she had undergone vascularisation surgery in 2018, resulting in necrotic skin lesions of the heel and the posterior lower and middle third of the leg. The now necrotic Achilles tendon was removed following an attempted surgical restoration (ulcerectomy) and an unsuccessful autologous surgical graft. Since the surgery, the skin lesion had remained open with an exposed calcaneal spine.
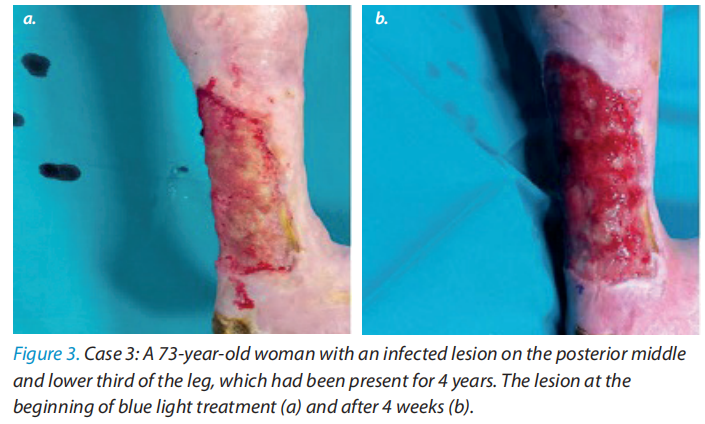
Upon examination, the lesion appeared clear, however, biofilm, medium levels of exudate, firm and calloused borders around skin were observed. The superficial swab tested positive for multidrug-resistant Pseudomonas aeruginosa and extended-spectrum betalactamase Escherichia coli. An X-ray of the foot revealed no evidence of osteomyelitis. Arterial Doppler ultrasound was valid in the right the periphery and erythematous perilesional popliteal artery, in the anterior tibial artery and in the dorsal artery of the foot. An antibacterial primary dressing and a secondary dressing with hydrofibre were used on the patient, alongside moderate compression bandaging and 60 seconds of treatment with blue light over the entire wound surface twice a week.
Case 4
An 89-year-old man with Horton’s arteritis and diverticulitis presented with a skin lesion on the trochanter [Figure 4] of about a year’s duration. There was a small papule with aggravating evolution and an appearance similar to pyoderma gangrenosum.
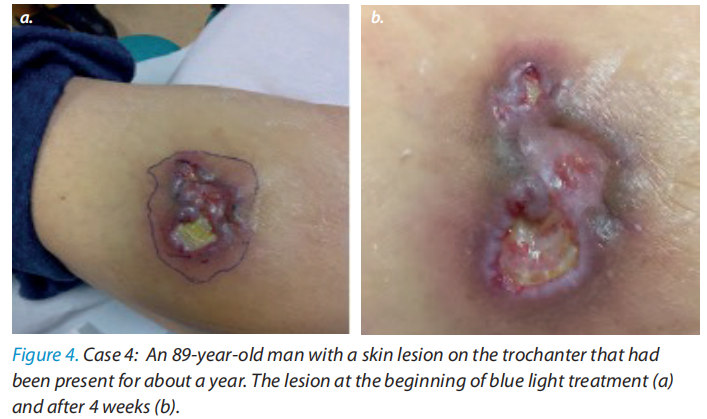
The base of the lesion appeared nonhomogeneous with slough. High levels of exudate, rolled and raised inflamed borders and purple perilesional collar with adjacent erythema were also observed on examination.
A primary exudate-transfer dressing and a secondary dressing with hydrofibre were used on the patient, as well as blue light treatment for 120 seconds on the entire wound surface twice a week.
Case 5
A 52-year-old man in good general health presented with a pressure lesion of 1 year’s duration on the stump of the right leg due to contact with his prosthetic silicone sleeve [Figure 5]. The lesion was classified as a grade 3 pressure ulcer by the European Pressure Ulcer Advisory Panel Pressure Ulcer Classification Tool, with a superficial cleansed base but with biofilm, abundant exudation, firm borders and perilesional skin with signs of maceration.
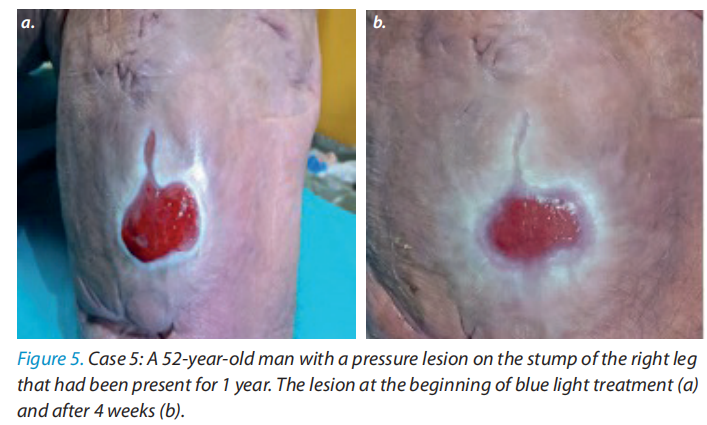
The lesion was treated with negative pressure therapy for 3weeks, however, no significant signs of improvement were seen, thus, the patient was selected for 60 seconds of blue light treatment over the entire surface of the wound twice a week, in conjunction with a polyurethane foam dressing.
Results
At the end of 4weeks, all five patients experienced a significant reduction in lesion area (57.63% on average). At the time of enrolment, wound bed score ranged between 4 and 7 (mean 5.4), and at the end of therapy it ranged between 10 and 16 (mean 13.2), showing an important improvement [Table 1].
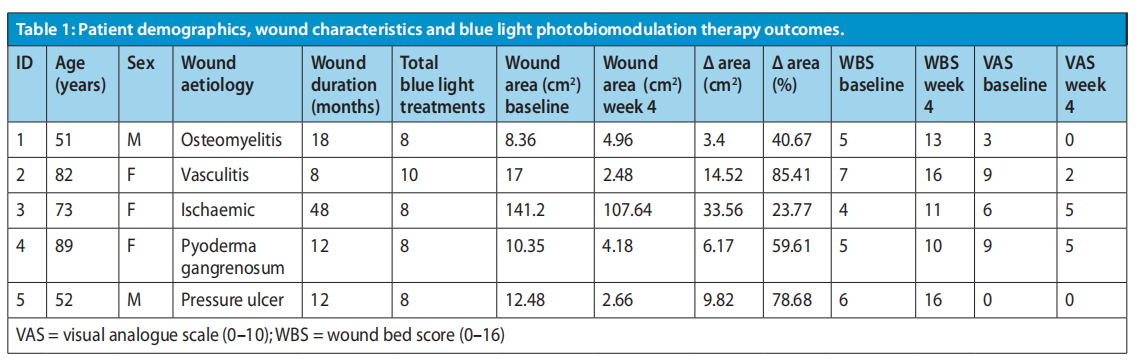
The trend in pain relief confirms the positive impact of treatment, varying between 0 and 9 (mean 5.4) at the time of enrolment and between 0 and 5 (mean 2.4) at the end of therapy. The results obtained from each patient are reported in Table 1 and shown in Figures 1–5.
Discussion
The inflammatory process is an integral part of wound healing and disruption of this process is recognised as one of the primary causes of impaired wound healing.
Blue light acts on inflammation by stimulating a faster transition; this effect has been demonstrated in preclinical studies where the early arrival of inflammatory infiltrate cells in the wound bed and an acceleration of the phenotypic switch of M1 to M2 macrophages marking the transition to the proliferative phase were observed in treated wounds (Cicchi et al, 2016; Magni et al, 2022).
Furthermore, blue light has the ability to modulate the oxidative state of cytochrome c and thus influence the process of cellular respiration, which is more important than ever in cells involved in tissue repair (Magni et al, 2020; Rossi et al, 2021). Previous clinical trials have demonstrated that blue light effectively promoted wound healing and reduced pain in patients with venous ulcers, vasculitis and traumatic wounds that did not respond to standard treatments (Marchelli et al, 2019; Dini et al, 2021; Fraccalvieri et al, 2022).
The therapies commonly used for wound care are advanced dressings – a wide range of topical solutions whose function is to maintain or restore the tissue microenvironment, so that the main cells involved in the reparative process can carry out their functions and the physiological healing process is not altered. When the inflammatory process stalls, it alters this favourable environmental condition, the repair process is interrupted and the lesion tends to become stagnant. Therefore, it is necessary to proceed with therapeutic approaches that go beyond the optimisation of the tissue microenvironment, capable of stimulating the overcoming of the inflammatory stall.
Blue light photobiomodulation therapy can play a key role in this context, as shown in these cases by the reduction of wound area and wound bed score at week 4 in the five patients. In these patients, the reduction/resolution of the inflammatory phase was manifested by the progression of the wound borders, the reduction of perilesional hyperaemia and the reduction of pain. Despite having different underlying pathophysiologies, all five ulcers responded to the blue light therapy, demonstrating that all ulcers have a final common pathway, which results in behaviours that are similar.
Conclusion
According to our observation, blue light therapy can represent a new frontier of tissue repair, reducing wound size and pain and improving wound bed score in patients affected by stagnant wounds. Our preliminary data has led us to undertake an observation on a larger sample, randomising the patients who come to our outpatient clinic to verify our preliminary observations, with the aim of giving a further contribution to the search for therapeutic solutions that will improve the lives of our patients.
References
1. Cicchi R, Rossi F, Alfieri D et al (2016) Observation of an improved healing process in superficial skin wounds after irradiation with a blue-LED haemostatic device. J Biophotonics 9(6): 645–55
2. Dini V, Romanelli M, Oranges T et al (2021) Blue light emission in the management of hard-to-heal wounds. Ital J Dermatol Venerol 156(6): 709713
3. Falanga V, Saap LJ, Ozonoff A (2006) Wound bed score and its correlation with healing of chronic wounds. Dermatol Ther 19(6): 383–90
4. Fraccalvieri M, Amadeo G, Bortolotti P et al (2022) Effectiveness of blue light photobiomodulation therapy in the treatment of chronic wounds. Results of the Blue Light for Ulcer Reduction (B.L.U.R.) Study. Ital J Dermatol Venerol 157(2): 187-194
5.Magni G, Banchelli M, Cherchi F et al (2020) Experimental study on blue light interaction with human keloid-derived fibroblasts. Biomedicines 8(12): 573
6. Magni G, Tatini F, Siena G et al (2022) Blue-LED-light photobiomodulation of inflammatory responses and new tissue formation in mouse-skin wounds. Life (Basel) 12(10): 1564
7. Marchelli M, Perniciaro G, Granara D et al (2019) Photobiomodulation with blue light in non-healing wounds: case series evaluation. Wounds International 10(3): 63–7
8. Rossi F, Magni G, Tatini F et al (2021) Photobiomodulation of human fibroblasts and keratinocytes with blue light: implications in wound healing. Biomedicine 9(1): 41
9. Schultz GS, Sibbald RG, Falanga V et al (2003) Wound bed preparation: a systematic approach to wound management. Wound Repair Regen 11(Suppl 1): S1–28
10. Troxler M, Vowden K, Vowden P (2006) Integrating adjunctive therapy into practice: the importance of recognising ‘hard-to-heal’ wounds. World Wide Wounds. Available from: http://www. worldwidewounds.com/2006/december/Troxler/ Integrating-Adjunctive-Therapy-Into-Practice.html (accessed 12.04.23)
This article is excerpted from the Wounds International 2023 | Vol 14 Issue 2 by wound world。


