Introduction
Femoral head osteonecrosis or avascular necrosis (AVN) could be traumatic or atraumatic in nature, and the atraumatic AVN is either due to either ischaemia or idiopathic origin. Though there is certainty in the clinical manifestation of femoral head avascular necrosis there is still uncertainty in the causative aetiology and natural course of the disease development. The annual incidence of the femoral head AVN ranges from 15,000/year in the USA, 3000/year in Japan, and 14,000/year in South Korea [1].
Femoral head AVN is a multifactorial disease, caused by compromised blood supply which results in the death of the bone marrow cells and osteocytes resulting in fractures, and articular surface collapse eventually leading to arthritis [2]. The basic pathophysiology mechanisms are vascular interruption due to fracture, endoluminal obstruction, or elevated intraosseous pressure and hence the risk factors are smoking, dyslipidemia, metastasis, pancreatitis, connective tissue disorders like Systemic Lupus Erythematosus (SLE), sarcoidosis, sickle cell anaemia, barotrauma, steroid intake, prior surgery, etc [2]. Multiple classification systems have been described like Ficat and Arlet, Association Research Circulation Osseous (ARCO), Mitchell’s classification, Japanese Investigation Committee Classification, and Steinberg classification which are all based either on radiographs and Magnetic Resonance Imaging (MRI), or histology and scintigraphy. Though asymptomatic initially AVN can at times present with pain over the hip with radiation to the buttocks or knee. Multiple treatment modalities have been described including both surgical and medical. With the collapse, the symptoms worsen limiting also the treatment choices to total hip arthroplasty (THA). Other surgical treatments like core decompression and osteotomies play a role in early-stage disease. Along with surgical management, non-invasive medical treatment has been described for initial disease [1–7].
The various medical management methods are pharmacological and biophysical modalities. The pharmacological treatments are antiplatelet, anticoagulants [8], vasoactive agents [9], and statins [10] to increase the blood supply of a femoral head which is compromised [11]. The other most important pharmacological agent is bisphosphonates [2, 6, 7]. Their mechanism of action is the suppression of osteoclast activity. The most commonly used bisphosphonates are alendronate and zoledronic acid. The other conservative modalities are biophysical which are Hyper Baric Oxygen Therapy (HBOT) [1, 2], shockwave therapies like Extracorporeal Shock Wave Therapy (ESWT) [3, 4], and electrical stimulation like Pulsed Electro Magnetic Field (PEMF) [5].
Shock wave therapy can restore tissue oxygenation by reducing oedema and inducing osteogenesis as well as neovascularization [3, 4]. HBOT delivers oxygen at high concentrations and pressures greater than one atmosphere. The mechanism of action is by either increasing reactive oxygen or nitrogen radicals to modulate the inflammatory response with the help of hypoxic inducible factors leading to increased angiogenesis and vascularisation [1, 2]. Electrical stimulation uses electrical fields which have positive effects on osteocytes, osteoblasts, and bone formation [5]. The pharmacological and biophysical modalities aim at inducing new bone formation and preventing collapse to delay the collapse and avoid an arthritic joint [2, 6, 7].
Multiple studies and even systematic reviews have been described for each conservative modality. But there is no consensus on the superiority of one treatment over another in the initial stages to delay and avoid a joint failure. So in this study, we reviewed the systematic reviews of all the conservative therapies for AVN systematically to identify a single or a combination of non-surgical treatment choices in the initial stages of the disease.
Methodology
A systematic review of the literature was performed according to PRISMA [12] (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to assess the systematic reviews for conservative management for avascular necrosis of the femoral head and the study has been registered under Prospero (CRD42022306543).
Search Strategy
A comprehensive literature search was conducted by two authors independently (SKM and HG) using Pubmed, EMBASE, and Cochrane databases. The Mesh words and Keywords used were “femoral head AVN”, “Conservative management”, and “Systematic Reviews”. The final literature search was carried out on January 22, 2022.
Study Selection
Studies were considered eligible for inclusion in this review if they matched the following inclusion criteria.
1. Patients with avascular necrosis of the femoral head due to any pathology including idiopathic and secondary
2. Such patients with AVN are managed with conservative therapies like bisphosphonates, Hyper Baric Oxygen Therapy (HBOT), Shock wave therapies like Extracorporeal Shock Wave Therapy (ESWT), or electrical therapy like Pulsed Electro Magnetic Field (PEMF).
3. Systematic reviews only
Analysis
The data from the final included studies were extracted and recorded in a Microsoft Excel spreadsheet by two authors independently (SK and RG). The data included the level of evidence of various included studies, patient size, mean follow-up period, inclusion and exclusion criteria, modality of treatment and its duration and dosage, functional outcomes, and failures. The outcomes of all the studies were assessed. The outcomes included progression of AVN and conversion to Total Hip Arthroplasty (THA), clinical and functional improvement, and scores like the Visual Analogue Scale (VAS) and Harris Hip Score (HHS).
The outcome measures were not pooled because of the heterogeneity of the various systematic reviews. So they are presented in a narrative summary fashion.
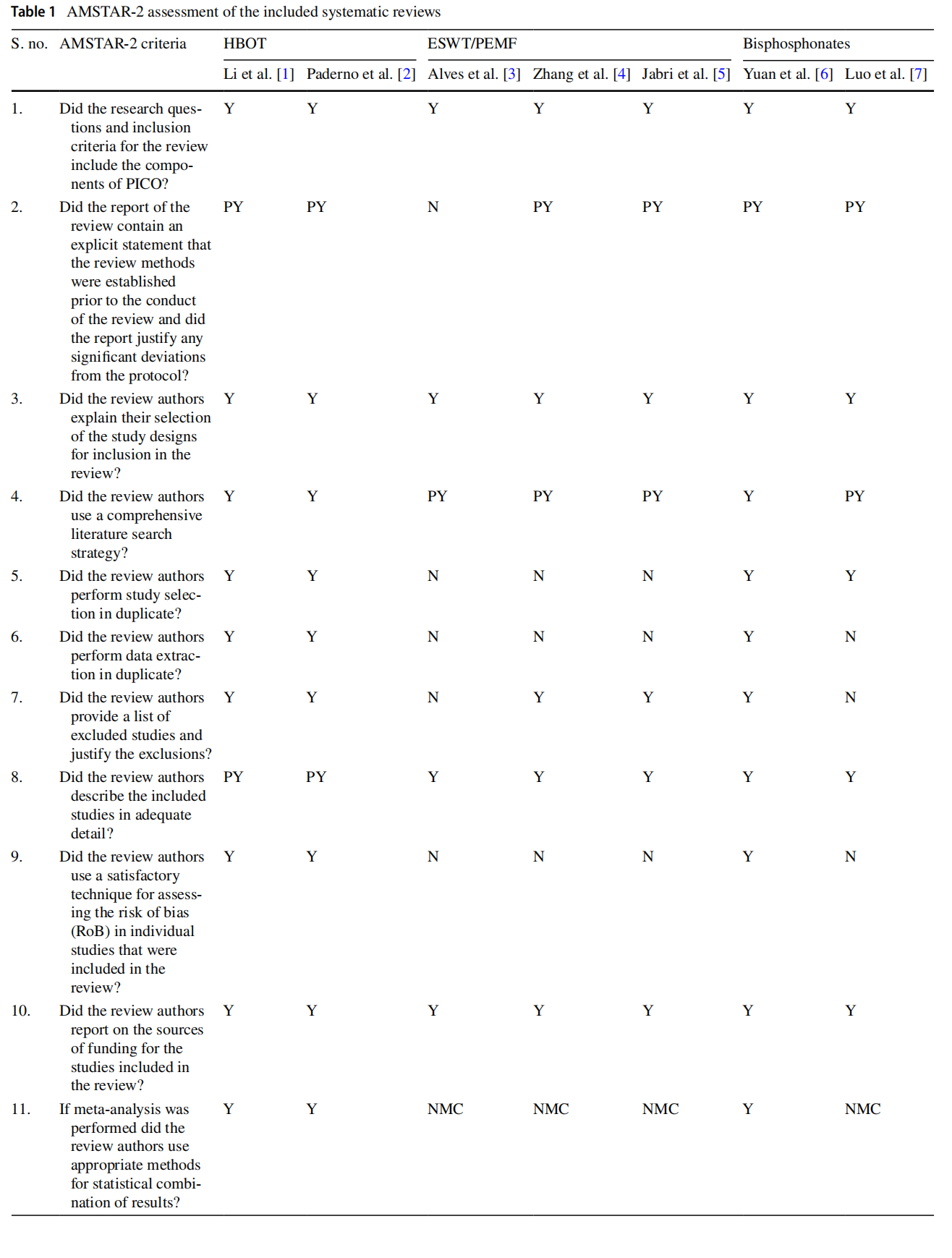
Quality Assessment of the Included Systematic Reviews (Table 1)
The quality of the included systematic reviews was assessed using AMSTAR-2 criteria [13]. The AMSTAR-2 criteria don’t generate an overall score. It contains sixteen domains which were marked either as yes [Y], partially yes [PY], no [N] and no meta-analysis conducted [NMC]. Some domains are grouped as critical domains (domains 2, 4, 7, 9, 11, 13, 15). Based on the weakness in the critical and non-critical domains an overall rating was generated as high, moderate, low, and critically low [13].

Results
PRISMA Flow Chart
The initial search of the databases based on the Mesh and Keywords yielded 364 results. Among the 364 search results, filters were applied to include systematic reviews and exclude editorials, conference abstracts, and book chapters as a part of step one (identification) before proceeding to step two (screening). This yielded 72 studies for screening. By applying the inclusion criteria for the 72 studies, the initial screening was done using titles and abstracts in Pubmed, Cochrane, and EMBASE which yielded 15 studies. For all 15 studies, full texts were retrieved to assess their inclusion in our review, and 8 were excluded (supplementary file). At the end of the scrutinization of the literature search, a total of 7 systematic reviews were considered for this study.
Systematic Reviews with Included Studies, Level of Evidence, Aetiology, and Grades of AVN and Date and Databases Searched (Table 2)
There were 2 systematic reviews for HBOT [1, 2], 2 for shock wave therapy (ESWT) [3, 4], 1 for electrical stimulation (PEMF) [5], and 2 for bisphosphonates [6, 7]. In each of the included systematic reviews, the studies ranged from 5 to 17 with overlap among the reviews. The level of evidence of one systematic review [6] was level 1 which included only Randomized Control Trials (RCT) as inclusion criteria [6] and the rest of the reviews [1–5, 7] level of evidence was level 3 due to the heterogeneous nature of the included studies. The AMSTAR-2 [13] analysis was done for all the reviews included (Table 1). Based on the weakness in critical and non-critical domains, three systematic reviews had no flaws in their criteria and the overall confidence in their results were considered as high [1, 2, 6]. The other four studies had more than one flaw in the critical and non-critical domains and hence their overall confidence was considered critically low [3–5, 7].

In 2 studies [1, 2] only idiopathic AVN cases were included, in one [5] both idiopathic and secondary causes were taken as criteria, in the rest [3, 4, 6, 7] there was no clear consensus on the inclusion criteria based on the aetiology. The grades of AVN in 2 of the systematic reviews [1,2] included Ficat 1–4, in 3 systematic reviews [4, 5, 7] Ficat 1–3 and ARCO 1–3 were included and in 2 reviews [3, 6] no data was available.
Inclusion and Exclusion Criteria of the Systematic Reviews Along with Treatment Protocol, Dosages, Duration, and Follow‑Up (Table 3)
There were no specific inclusion criteria other than those of the treatment modality and in one study [6] only RCT was included. The exclusion criteria for two studies where HBOT [1, 2] was the treatment modality were secondary AVN and bone marrow oedema. The follow-up of the patients in the included systematic reviews varied from 6 weeks to 10 years. Almost all of the studies had control groups and there was variation in either dosage or duration of the treatment across the included reviews.

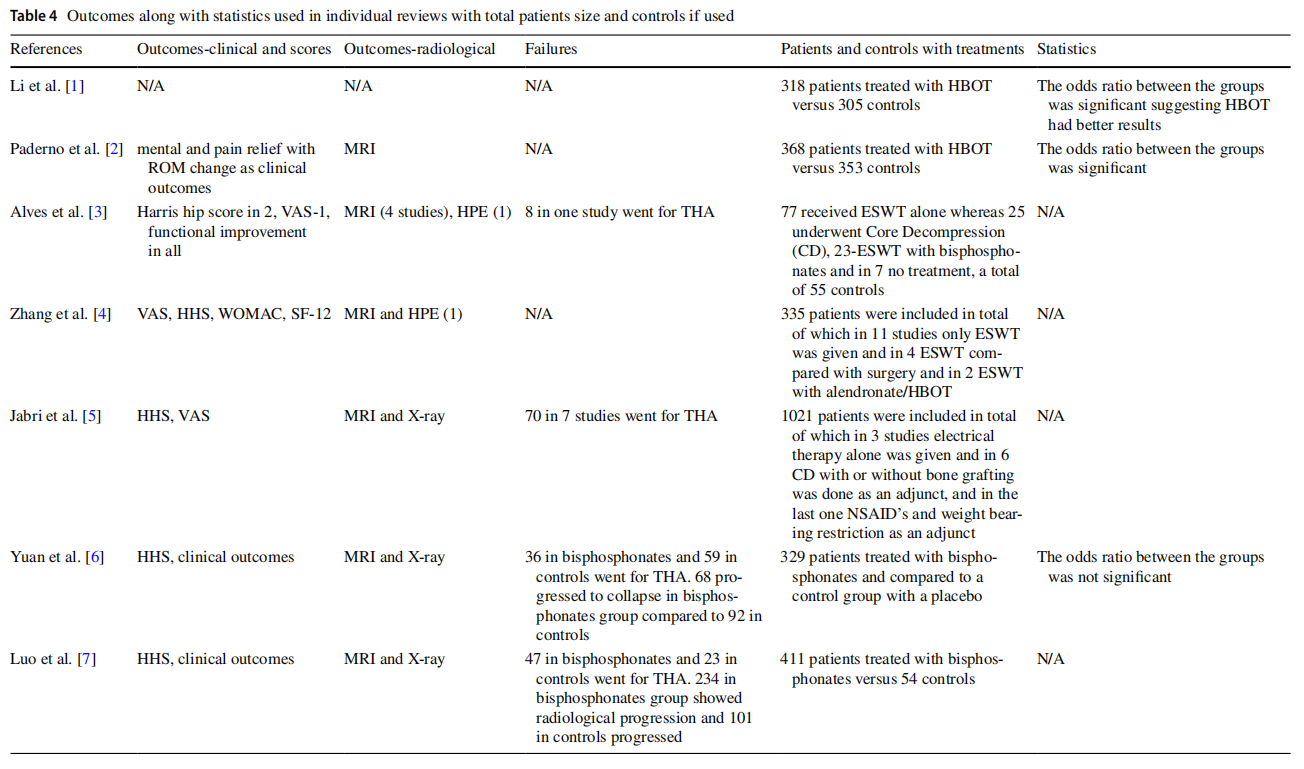
Outcomes Along with Statistics Used in Individual Reviews with Total Patients Size and Controls (Table 4)
In almost all of the studies the outcomes were measured, wherein they used both clinical criteria, scoring systems, and radiological criteria. The failures or disease progression was not described across all of the reviews but they were mentioned in some articles of some reviews leaving the data inhomogeneous. The total number of patients varied from 77 to over 1000 across the systematic reviews. Almost all of the studies included a control group that either received the intended treatment with adjuncts or did not receive any treatment at all. Because of the heterogeneous nature of included articles in the systematic reviews meta-analysis was performed [1, 2, 6] in only 3 of the included systematic reviews.
Discussion
AVN of the femoral head, a multifactorial disease, is the result of compromised blood supply which leads to the collapse of the articular surface eventually leading to arthritis and requiring total hip arthroplasty. With its increasing prevalence in the younger age group worldwide, the need to delay the inevitable end-stage arthritis is necessary to avoid an early THA. Multiple medical and surgical treatments have been described in the early stages which delay the disease progression. Multiple studies, trials, reviews, and systematic reviews exist for the various treatments described and their outcomes but with no consensus over which is superior. In this study, we reviewed the systematic reviews wherein conservative medical management has been used as a treatment of choice for AVN. In this review article, we studied a total of 7 systematic reviews, in 2 studies HBOT [1, 2] was the treatment used, shock wave therapy modalities in 2 more [3, 4], electrical therapy in one [5], and the last two bisphosphonates [6, 7] were used. The included systematic reviews though exhibited heterogeneity in their inclusion and exclusion criteria, including studies and patient size, follow-up period, and treatment modality, almost all of them had a control group for comparing the outcomes of the management [1–7].
Li et al. [1] in their systematic review included studies where patients with all the stages of femoral head osteonecrosis are included and subjected to HBOT. The study concluded that when compared to controls the patients who received HBOT achieved significant clinical improvement. The rationale being HBOT can improve the tissue oxygen partial pressures and enhance the activities of osteoblasts, osteoclasts, fibroblasts, and bone morphogenic proteins, which leads to neo-vasculogenesis, osteogenesis, reduce local inflammation, inflammatory markers (TNF, IL-6) and oedema and also increases the bone formation markers. Similarly, Paderno et al. [2] in their systematic review also included studies where patients who are treated with HBOT are compared with controls with statistically significant improvement in function. The treatment protocol proposed was 60–90 episodes of HBOT with one episode per day at 2–2.5 atmospheres for one hour. But the said treatment is costly ranging from 6000 US dollars to 9000 US dollars for all the episodes and requires the equipment for the therapy [2]. HBOT has been recommended as a treatment for various conditions like carbon monoxide poisoning, radio necrosis, gas embolism, decompression sickness, burns, etc., and its usage is extended to the treatment for femoral head osteonecrosis also but as an adjunct according to the tenth European consensus conference for hyperbaric medicine [14].
Alves et al. [3], and Zhang et al. [4] used shock wave therapy as a modality of choice for the treatment of AVN femoral head. The rationale is that shock waves are acoustic waves at high pressure and velocity which are used to stimulate osteogenesis and neovascularization. In his systematic review, Alves et al. [3] included 5 studies that used a single treatment by a shock wave, in one study they were compared with core decompression; in one more with alendronate, and both the studies the shock wave group had better functional and radiological outcomes. In the rest of the studies, the controls did not receive any additional treatment and the patients who received shock waves had favourable outcomes at 2–3 years of follow-up. Zhang et al. [4] included 17 studies in their systematic review which compared the effect of ESWT alone, and ESWT with surgical options like core decompression, and multiple drilling with or without bone grafting. They concluded that shock wave therapy has more benefits than core decompression and grafting and it can be supplemented with a pharmacological modality for better efficacy.
Jabri et al. [5] in their systematic review included 10 studies that used electrical stimulation like pulsed electromagnetic field (PEMF), direct current stimulation (DC), and capacitive coupling (CC) as a modality of treatment. In six studies PEMF was used and compared to a surgical treatment like core decompression, and multiple drilling. In the rest 4 studies, DC/CC was used to compare with surgical treatment. Their study concluded that PEMF had better outcomes both clinical and radiological when compared to surgical outcomes, but the same is not true for DC/CC.
Yuan et al. [6] and Luo et al. [7] compared the effect of bisphosphonates in the management of femoral head osteonecrosis in their systematic reviews. The mechanism of action of bisphosphonates is by inhibiting the activity of osteoclasts which delays any articular collapse and gives time for bone regeneration to occur. Yuan et al. [6] included 5 RCTs in their systematic review, of which in one study there was a significant difference between the cases and controls. But in the other four studies the difference was not significant between the groups, the reasons attributed were low sample size, supplementary treatment like ESWT, drilling, and calcium/vitamin D3 in both the groups which could have biased the outcomes. In the systematic review by Luo et al. [7], 8 studies were included, both in short term and long term the bisphosphonates-treated group showed favourable outcomes both clinically and radiologically when compared to controls or untreated AVN historical data. The longest follow-up period was for 10 years and the patients received alendronate 10 mg daily or a 70 mg weekly basis for 3 years. In the short-term period during the treatment, there was a clinical and radiological improvement and during the longterm follow-up of 10 years, though there was a decline in function once the treatment was stopped after 3 years, the radiological and clinical decline was lower compared to the untreated AVN historical data at 10 years suggesting a short term as well as long term favourable results for patients with AVN treated with bisphosphonates.
Li et al. [1] and Paderno et al. [2] in their systematic review concluded that patients with AVN treated with HBOT had better clinical outcomes than controls. Both the systematic reviews on HBOT [1, 2] had higher overall confidence scores in AMSTAR-2 [13] as there were no flaws in the critical domains (Table 1). The tenth European consensus conference for hyperbaric medicine [14] also recommended the usage of HBOT for AVN, but as an adjunct. The systematic reviews on ESWT [3, 4], and PEMF [5] as a treatment for AVN yielded better results. The overall score based on AMSTAR-2 [13] (Table 1) is considered critically low, as there were flaws in both critical and non-critical domains. The results which were summarised in all three reviews [3–5] had better results in patients who underwent ESWT [3, 4] or PEMF [5] for AVN. In a few individual studies included in the reviews, the results are even better than core decompression [3–5]. The systematic reviews which compared bisphosphonates as a treatment for AVN yielded better results both at a short-term period of 3 years and a long-term period of 10 years. In one review [6] the overall score based on AMSTAR-2 [13] is high, as there were no flaws in the critical domains.
Our review concentrated on conservative management for the AVN. There are multiple individual articles as well as systematic reviews for each modality of conservative treatment of AVN. Each article on this topic concentrates mainly on one or two modalities of management. Hence the efficacy of different modalities of conservative management is difficult to formulate. Our study bridges this missing link in the literature. This we consider the biggest strength of our study.
Our limitations were, because of the heterogeneous nature of the individual studies in all of the included systematic reviews, and the heterogeneity of the systematic reviews themselves, a meta-analysis was not done and the data was summarized narratively. We have not discussed the surgical management for avascular necrosis, as our review article is on conservative modalities.
Conclusion
Of all the modalities of treatment described, bisphosphonates are easily available and cost-effective and don’t require any hospital resources/machinery for delivering the treatment. So they can be used as an initial line of treatment for patients with early stages of AVN (Ficat and Arlet 1–3) and based on the hospital availability of resources could be supplemented with any of the biophysical modalities (ESWT/PEMF/HBOT) for maximum efficacy to delay the disease progression.
Supplementary Information
The online version contains supplementary material available at https:// doi.org/10.1007/s43465-023-00818-5.
Author Contributions Dr. SK and Dr. VKD were involved in the conception of the idea for the study. Dr. SK and Dr. HS were involved in the literature search based on the Prisma guidelines and identifying the final studies to be included in the review. Dr. RK and Dr. SK were involved were involved in interpreting the involved studies, data extraction and analysis. Dr. SK and Dr. VKD were involved in writing the manuscript post analysis. Dr. RM was involved in overseeing and proof reading the manuscript. All the authors read the final manuscript and gave consent for publication.
Funding This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Data Availability The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest The authors of this paper have no conflict of interest to declare in the preparation and submission of this manuscript.
Ethical Standard Statement This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent For this type of study informed consent is not required.
References
1. Li, W., Ye, Z., Wang, W., Wang, K., Li, L., & Zhao, D. (2017). Clinical effect of hyperbaric oxygen therapy in the treatment of femoral head necrosis: A systematic review and meta-analysis. Klinische Wirksamkeit der hyperbaren Sauerstoftherapie bei Femurkopfnekrose: Systematische Übersicht und Metaanalyse. Der Orthopäde, 46(5), 440–446. https://doi.org/10.1007/ s00132-016-3360-8
2. Paderno, E., Zanon, V., Vezzani, G., et al. (2021). Evidencesupported HBO therapy in femoral head necrosis: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 18(6), 2888. https://doi.org/10.3390/ ijerph18062888
3. Alves, E. M., Angrisani, A. T., & Santiago, M. B. (2009). The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: A systematic review. Clinical Rheumatology, 28(11), 1247–1251. https://doi.org/10.1007/s10067-009-1231-y
4. Zhang, Q., Liu, L., Sun, W., Gao, F., Cheng, L., & Li, Z. (2017). Extracorporeal shockwave therapy in osteonecrosis of femoral head: A systematic review of now available clinical evidences. Medicine (Baltimore), 96(4), e5897. https://doi.org/10.1097/MD. 0000000000005897
5. Al-Jabri, T., Tan, J. Y. Q., Tong, G. Y., et al. (2017). The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: A systematic review. BMC Musculoskeletal Disorders, 18(1), 319. https://doi.org/10.1186/ s12891-017-1663-5
6. Yuan, H. F., Guo, C. A., & Yan, Z. Q. (2016). The use of bisphosphonate in the treatment of osteonecrosis of the femoral head: A meta-analysis of randomized control trials. Osteoporosis International, 27(1), 295–299. https://doi.org/10.1007/ s00198-015-3317-5
7. Luo, R. B., Lin, T., Zhong, H. M., Yan, S. G., & Wang, J. A. (2014). Evidence for using alendronate to treat adult avascular necrosis of the femoral head: A systematic review. Medical Science Monitor, 20, 2439–2447. https://doi.org/10.12659/MSM. 891123
8. Glueck, C. J., Freiberg, R. A., Wissman, R., & Wang, P. (2015). Long term anticoagulation (4–16 years) stops progression of idiopathic hip osteonecrosis associated with familial thrombophilia. Advances in Orthopedics, 2015, 138382. https://doi.org/10.1155/ 2015/138382
9. Claßen, T., Becker, A., Landgraeber, S., et al. (2016). Long-term clinical results after iloprost treatment for bone marrow edema and avascular necrosis. Orthopedic Reviews (Pavia), 8(1), 6150. https://doi.org/10.4081/or.2016.6150
10. Pritchett, J. W. (2001). Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clinical Orthopaedics and Related Research, 386, 173–178. https://doi.org/10.1097/ 00003086-200105000-00022
11. Fessel, J. (2013). There are many potential medical therapies for atraumatic osteonecrosis. Rheumatology (Oxford), 52(2), 235–241. https://doi.org/10.1093/rheumatology/kes241
12. Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., & Stewart, L. A. (2015). PRISMA-P Group. Preferred reporting items for systematic review and metaanalysis protocols (PRISMA-P) statement. Systematic Reviews, 4(1), 1.
13. Shea, B. J., Reeves, B. C., Wells, G., et al. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ, 358, j4008. https://doi.org/10.1136/bmj.j4008
14. Mathieu, D., Marroni, A., & Kot, J. (2017). Tenth European Consensus Conference on Hyperbaric Medicine: Recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment [published correction appears in Diving and Hyperbaric Medicine 2017 Jun;47(2):131–132]. Divng and Hyperbaric Medicine, 47(1), 24–32.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
This article is excerpted from the Indian Journal of Orthopaedics (2023) 57:410–420 by Wound World.


