Introduction
Continent ileostomy (CI) is a technical refinement of the conventional ileostomy (IS) that provides voluntary control over fecal evacuation. Due to the absence of an external bag, the quality of life with CI is significantly improved [1, 2]. An intraabdominal low-pressure reservoir (the pouch) and a continence mechanism (the nipple valve (NV)) are prerequisites for proper function [3]. The method was introduced in 1969 by Prof. Nils Kock of Gothenburg [4], leading to the common designation “Kock pouch” (KP).
Apart from the fact that CI has now been replaced by ileal pouch–anal anastomosis (IPAA) as the procedure of choice for proctocolectomy [5], manifold complications also stand in the way of widespread CI use [1, 6]. However, there are numerous patients who received CI or KP decades ago. Furthermore, patients remain today who are candidates for CI but not suitable for IPAA [2]. In addition, there is an increasing number of patients who eventually experience functional failure after temporarily good IPAA function, thus representing an indication for conversion to CI [7]. All these individuals may be at risk of developing late complications of CI. This results in a need for revision surgery.
The senior author has over 3 decades of experience with CI revision and corrective surgery. Since reports on this topic are extremely sparse, an update seems appropriate. The clinical data, including the results of revision surgeries, have been reported recently [8]. Herein, it is exclusively intended to present a systematic description of the surgical techniques based on the characteristics of the respective complications.
Methods
The medical records of 77 patients who had undergone a total of 133 CI revision surgeries between 1986 and 2015 were reviewed. Revision procedures were classified according to the anatomic site of the underlying complication:
- Class 1: revision surgery of the nipple valve
- Class 2: revision surgery of the pouch
- Class 3: revision surgery of the stoma
- Class 4: revision surgery of the afferent loop
Subtypes were specified according to the clinical severity of the complication and complexity of the surgical repair:
- a: minor clinical severity/easy surgical correctability
- b–d: increasing severity/more difficult correction
The characteristic features of the complications were summarized, and schematic illustrations were prepared for the appropriate surgical procedures. A primary S-design of the pouch was taken as the basis.
Results
Nipple valve revision surgery (class 1)
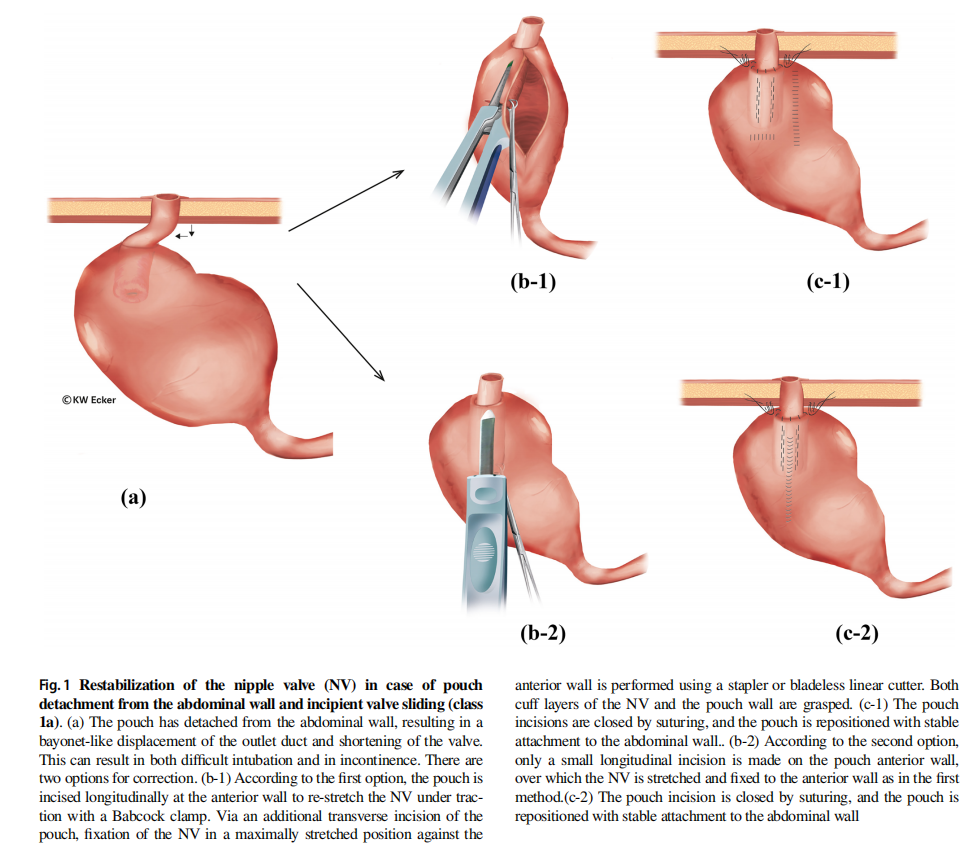
Class 1a: incipient slippage with/without detachment of the pouch from the abdominal wall
Incipient slippage is caused by traction of the mesentery on the tip of the NV leading to shortening of the nipple. It is often triggered by detachment of the pouch from the abdominal wall. This complication becomes symptomatic either because intubation is more difficult as a result of bayonetlike deformation of the outlet, or because full continence has been lost as a result of NV shortening. A revision indication is given according to the severity of the disturbance (Fig. 1).
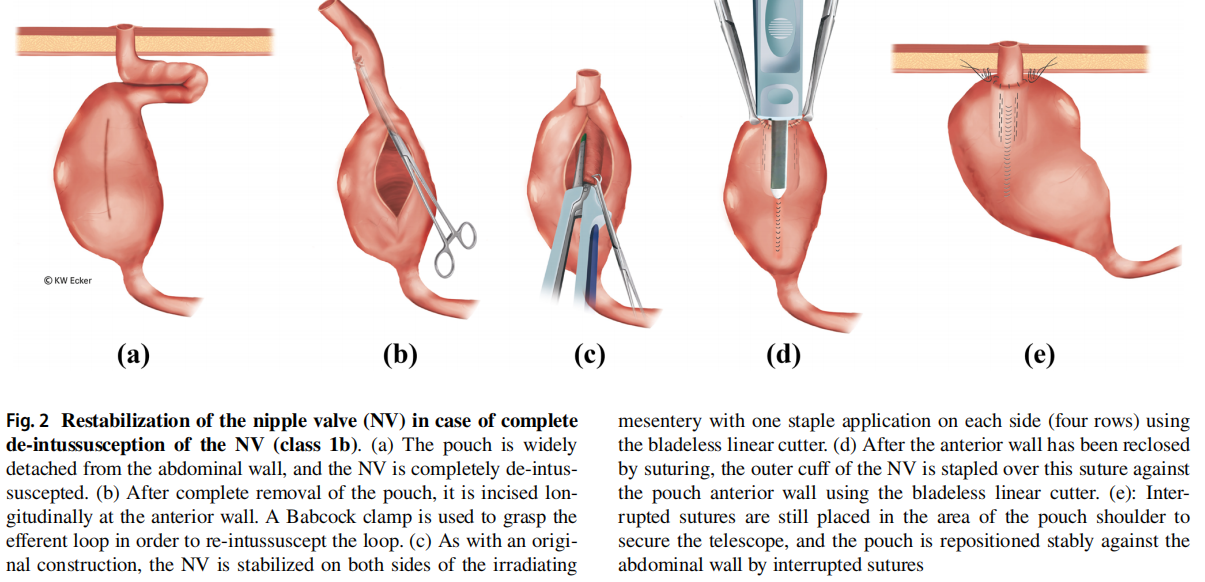
Class 1b: pronounced slippage (complete de‑intussusception) and prolapse
The end result of an unhindered sliding process is ultimately complete de-intussusception of the NV. Complete incontinence then represents an absolute indication for re-intussusception and restabilization (Fig. 2). A similar situation exists with prolapse of the valve through the stoma to the outside.
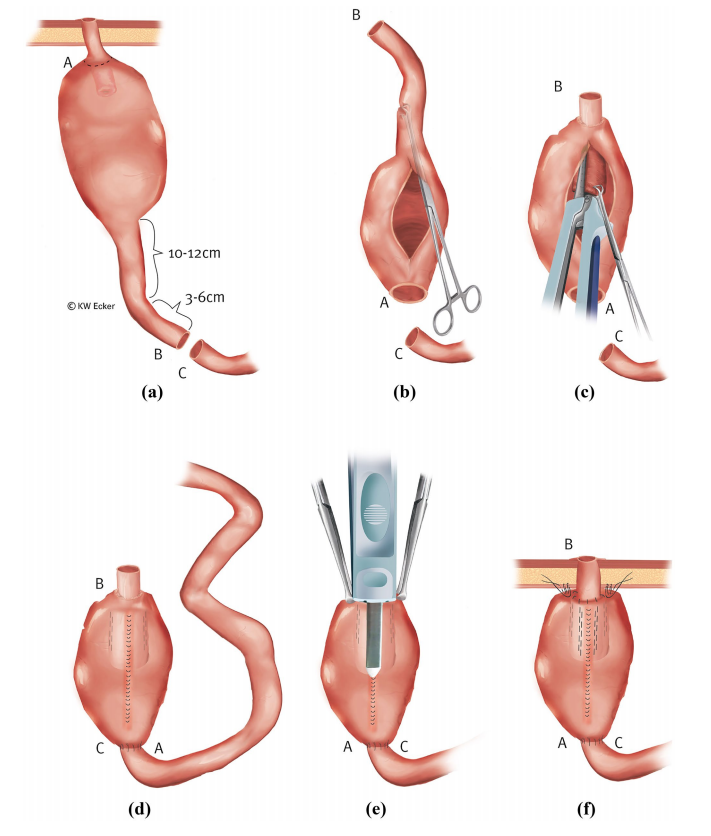
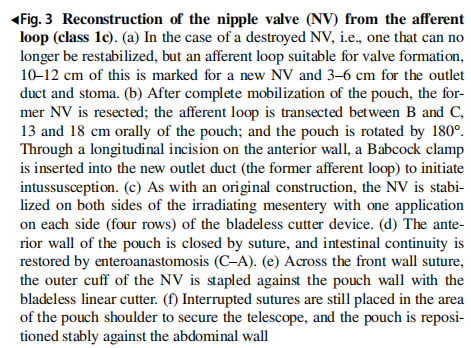
Class 1c: destruction and/or irreparability of the nipple valve
If sliding or prolapsing occurs chronically intermittently, inflammation and scarring may lead to morphologic destruction of the NV. There is an absolute indication for the reconstruction of the valve, usually from the afferent loop (Fig. 3).
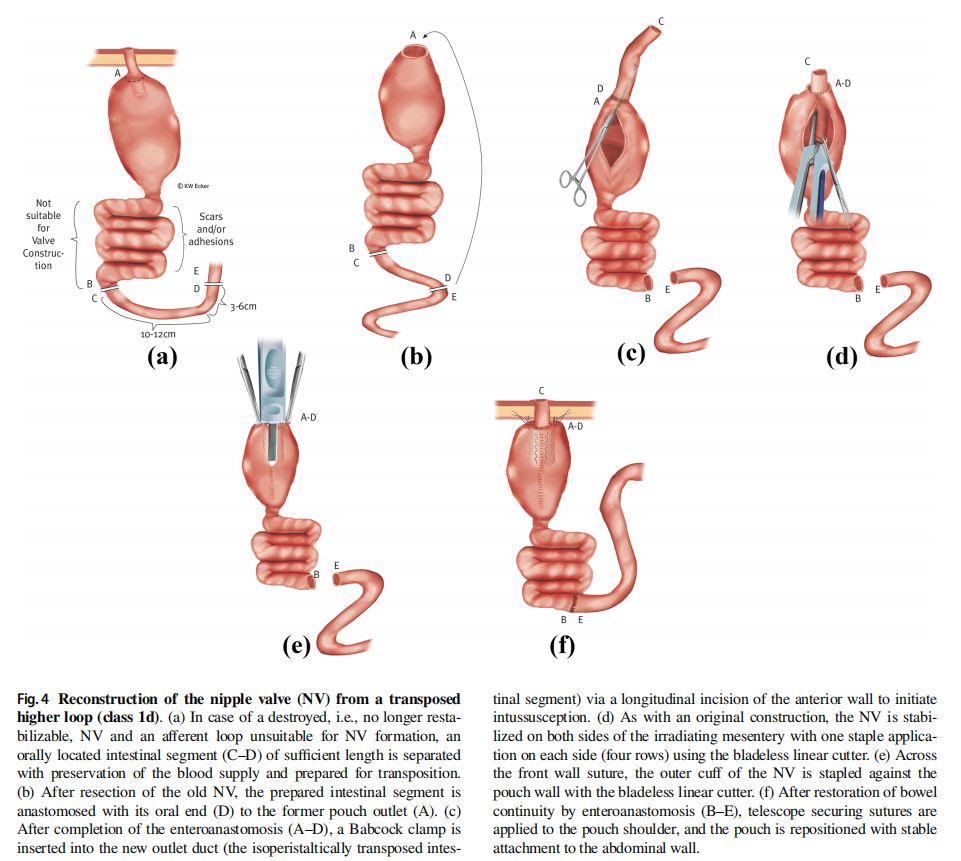
Class 1d: additional scars and thickening or dilatation of the afferent loop
In some unfavorable cases, the afferent loop is shown to be unsuitable for valve formation due to scarring and/or inflammatory changes. In cases where the loop can remain in situ with undisturbed function, it is advisable to construct a new NV from a transposed higher loop of the small intestine after resection of the old valve (Fig. 4). The same procedure is recommended if the afferent loop is considerably dilated.
Pouch revision surgery (class 2)
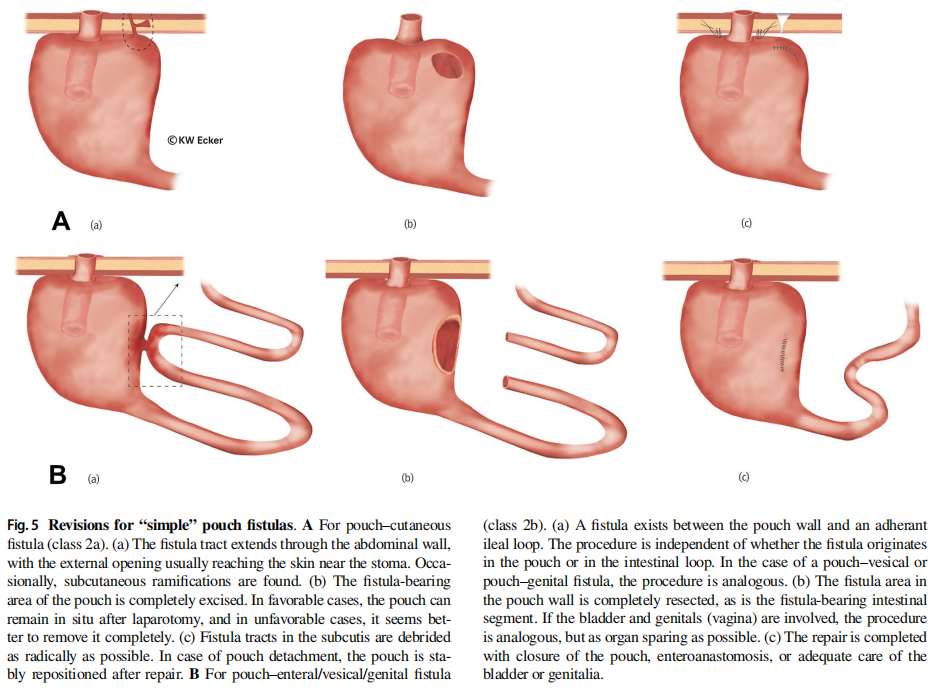
Pouch complications are mainly manifestations of the underlying disease. While adenomas in familial adenomatous polyposis (FAP) can be resected endoscopically and pouchitis in ulcerative colitis should be treated conservatively or requires sacrifice of the pouch, fistulas may represent an indication for surgical revision. Three types are to be distinguished:
Class 2a: pouch–cutaneous fistulas
Pouch–cutaneous fistulas are usually an expression of a penetrating complication of a Crohn’s manifestation. In rare cases, they may also be “suture fistulas” resulting from the attachment of the pouch to the abdominal wall. Surgical repair is indicated depending on fistula productivity (Fig. 5A).
Class 2b: pouch–enteric/vesical fistulas
These fistulas are comparable to the usual enteric Crohn’s fistulas. The indication for surgical removal depends on the potential for sepsis (Fig. 5B).
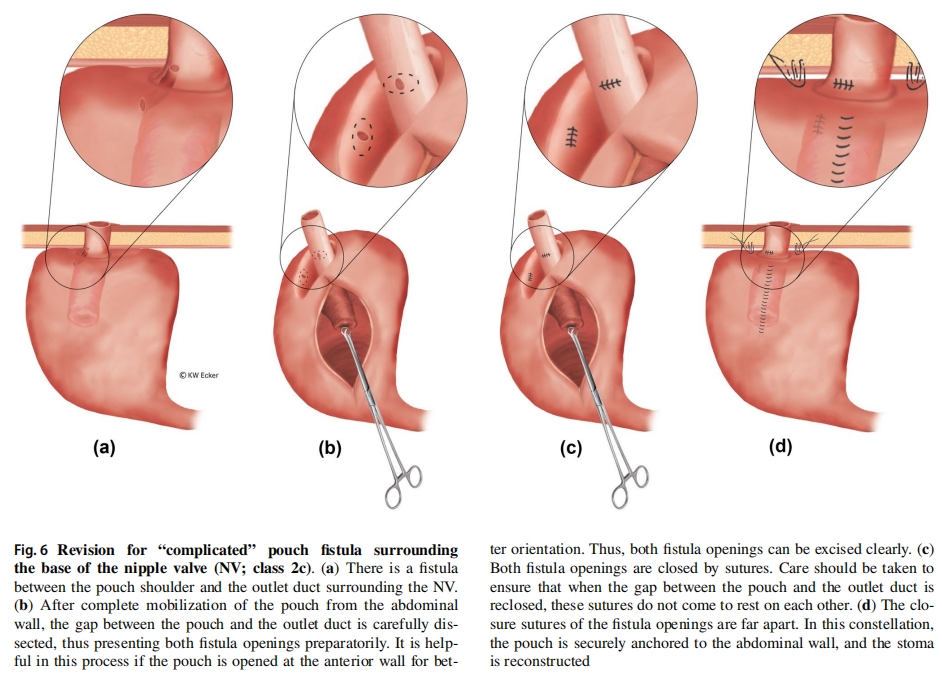
Class 2c: fistulas surrounding the valve at the base
These are the most difficult fistulas of all. Since they become symptomatic by partial or total incontinence, they counteract the objective of CI/KP and always represent an indication for treatment. Only if the pathogenesis is seen in Crohn’s disease can treatment with biologics be tried. However, subtle surgical closure is usually necessary (Fig. 6).
Stoma revision surgery (class 3)
Special stoma complications in CI are related to the specific nature of the actual planar design at the skin level.
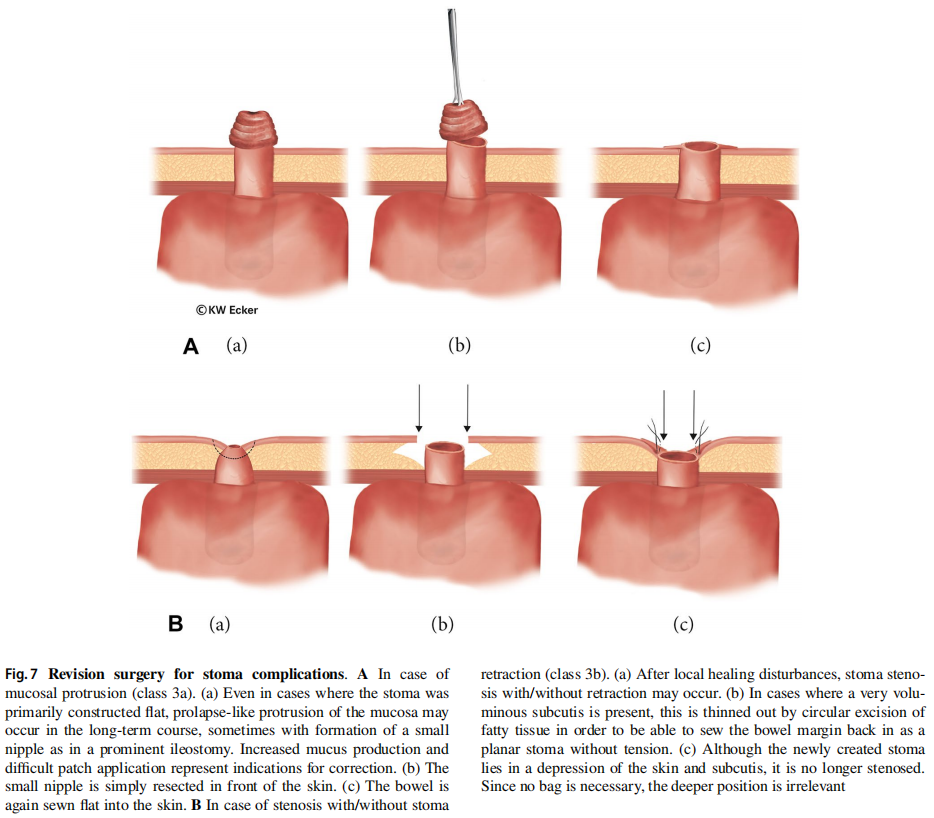
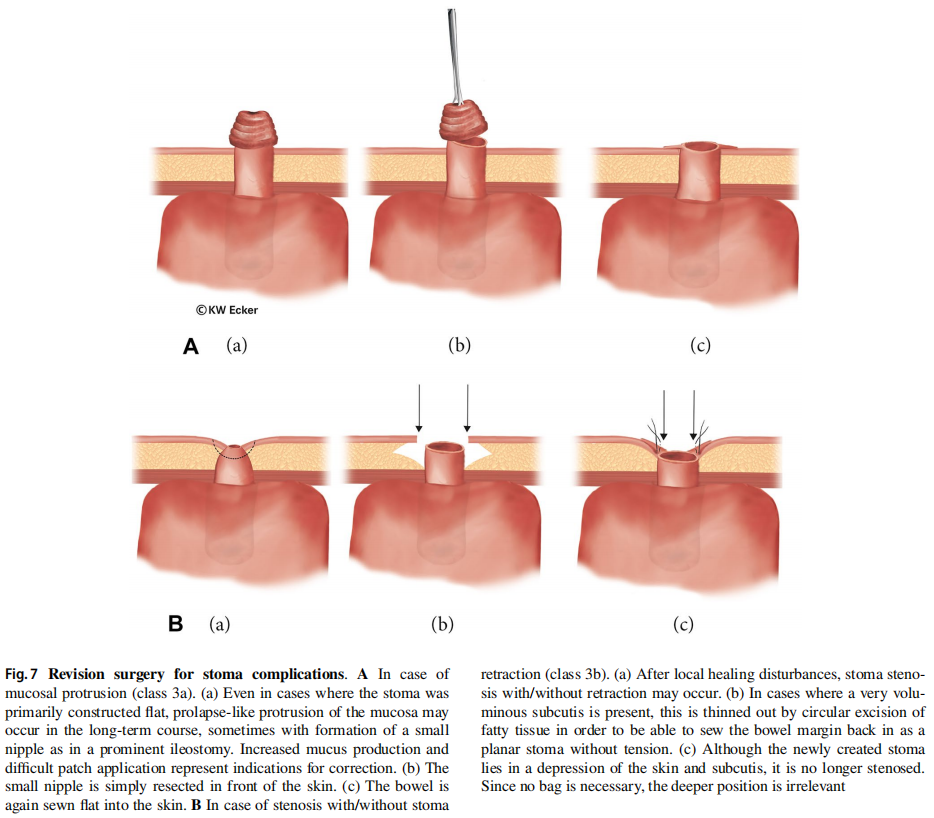
Class 3a: mucosal protrusion/full‑wall prolapse
In rare cases, mucosal protrusion may occur at the stoma. If the efferent loop was too generously dimensioned during stoma placement, full-wall prolapse of varying extent may also result. Depending on the excess mucosa, excessive mucus production is involved, which can overtax the absorption capacity of the special plaster for covering the stoma. Increased mucus secretion can first be managed conservatively using mini-bags; otherwise, surgical correction may be indicated (Fig. 7A).
Class 3b: stoma retraction with/without stenosis
If the efferent loop was inadvertently too short during stoma formation, or if the edge of the bowel was poorly perfused, retraction with/without stenosis may result. The consequences are more difficult intubation and usually also pain. Incipient stenosis at the skin level can usually be arrested with regular bougienage using Hegar’s pins. Sooner or later, however, corrective interventions are unavoidable (Fig. 7B).
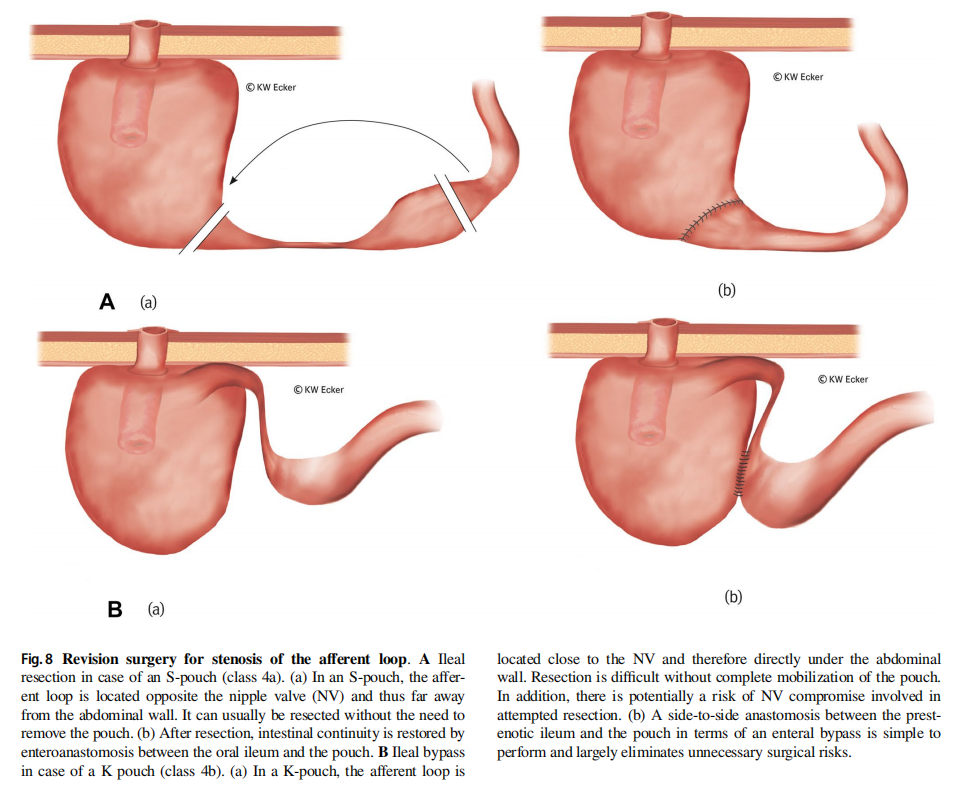
Reoperations at the afferent loop (class 4)
Revisions of the afferent loop are usually required because of stenosing or fistulating complications of Crohn’s disease.
Class 4a: afferent loop in S‑pouch
In the case of an S-pouch, resection can be performed without releasing the pouch completely since the afferent loop is opposite the valve and easily accessible (Fig. 8A).
Class 4b: afferent loop in K‑pouch
In the case of a K-pouch, resection of the afferent loop would require complete release of the pouch. In difficult situations, this could also endanger the NV due to its neighboring relationship to the afferent loop. Therefore, it may be wise to perform an intestinal bypass in selected cases (Fig. 8B).
Discussion
While most surgical reports are limited to NV revision surgery [6], this paper presents a synoptic overview over the variety of correction methods. The broad technical repertoire of corrective surgery helps to achieve astonishingly high cumulative CI survival rates of up to 78.8% after 44 years in patients with at least one revision surgery [8]. A requirement for intervention may result from all structural components of the CI (NV, pouch, stoma, and afferent loop). Therefore, four revision classes are defined herein. There are large differences between these classes in terms of the influence of the primary surgical technique and the underlying disease on pathogenesis of the respective complications.
In agreement with the literature, complications of the NV (class 1) are purely technical and characterized by instability of the nipple formation. They may arise when the small intestine attempts to reverse the forced unnatural intussusception. Stabilization with metal staplers, as commonly performed today, has ameliorated this problem considerably but not eliminated it completely [1]. Surgical techniques correspond to the severity of the complication. This means that restabilization of an existing valve takes priority over constructing a new one. If in the latter case the afferent loop is suitable, the method is referred to as the “turnaround” procedure; if a transposed higher small bowel loop is necessary, this is referred to as “pedicle” repair [6].
In contrast, complications of the pouch (class 2) and the afferent loop (class 4) are clearly related to the underlying disease. Diffuse inflammation (pouchitis in ulcerative colitis) requires sacrifice of the CI in favor of IS if conservative measures fail. On the other hand, penetrating complications of circumscribed inflammation (fistulas in Crohn’s disease) may be treated by limited excision, as with fistulas of other pathogeneses. The aim is to preserve pouch and function. In familial polyposis, recurrent adenomas can usually be resected endoscopically, and desmoids in the mesentery may be suppressed pharmacologically. Stenoses and fistulas of the afferent loop are indicative of Crohn’s disease, even in cases where the previous diagnosis was different. Because pouch fistulas that surround the valve at the base open in the outlet and thereby produce incontinence, they have traditionally been classified as valve complications [6]. However, the valve is morphologically uninvolved and must not be repaired in the process of surgical fistula closure. Therefore, in the authors’ opinion, these fistulas are more correctly classified as pouch fistulas. While immediate postoperative occurrence is rather to be considered a result of disturbed blood circulation or a suture insufficiency, all fistulas in the long-term course correspond to complications of Crohn’s disease. Regardless of the time of occurrence, the surgical corrective procedures are identical. For all types of late fistula, there are also conservative options (e.g., biologics) that can be used to avoid surgical intervention, or after surgery as prophylaxis against relapse as in non-pouch surgery [9]. Some complications of the pouch, such as foreign body accumulation (e.g., enteroliths), can be treated endoscopically [10].
In stoma complications (class 3), technical inadequacies, connective tissue weakness, unusual aging processes, and disease recurrence may be involved in complication pathogenesis. In this sense, the focus in CI is particularly on mucosal protrusion and retraction. If local correction is indicated, it is often to be performed in conjunction with abdominal revision for other complications.
Revision surgery is without a doubt at least as demanding as primary CI/KP surgery. However, in skilled hands, it can be extremely successful and thus represents an integral part of pouch surgery. Without exaggerating, we would like to note that apart from severe pouchitis, there is hardly any complication in CI that could not be eliminated by revision surgery. This is not only important for restoring the best possible quality of life: of even greater importance seems to be the avoidance of pathophysiological consequences of resection of terminal ileum sections in terms of hardly compensable water and electrolyte losses. Interested surgeons are recommended and encouraged to participate in technical workshops and to perform their first procedures under the supervision of an experienced tutor.
Conclusion
Based on classes of complications, the specialized surgeon may find differentiated techniques at their disposal to save the CI and avoid unnecessary sacrifice of the artificial continence organ. However, more reports are needed to evaluate the suitability and safety of these techniques from different perspectives.
Acknowledgements The authors thank Prof. Matthias Glanemann, Director of the Clinic for General, Visceral, Vascular, and Pediatric Surgery at Saarland University Hospital in D-66450 Homburg, Saar (Germany), and Carsten Krüger, Commercial Director of the MediClin Müritz-Klinikum in D-17192 Waren (Germany), for kind permission to view patients’ medical records in the clinic archive
Author contribution This work is part of the dissertation of Mathias Tönsmann. All authors contributed to the paper’s conception and design: Nils Karl Josef Ecker wrote the first draft of the manuscript. Mathias Tönsmann analyzed the medical records and generated the surgical illustrations with special graphics software. Karl-Wilhelm Ecker developed the classification of revision surgeries and revised the manuscript for important intellectual content. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding DEAL. Open Access funding enabled and organized by Projekt
Availability of data and material All data and materials used are secured digitally by the corresponding author.
Code availability No code available.
Declarations
Competing interests The authors declare no competing interests.
Ethical approval The study was approved by the Ethics Committee of the Medical Association of Saarland, Germany (ID no. 24/15) on 04.02.2015 and the Ethics Committee of the University of Rostock, Germany (registration number A 2015-0040) on 07.04.2015.
Consent to participate Not applicable.
Consent for publication Not applicable.
Conflict of interest The authors declare no competing interests.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
References
1. Nessar G, Wu JS (2012) Evolution of continent ileostomy. World J Gastroenterol 18:3479–3482. https://doi.org/10.3748/wjg.v18. i27.3479
2. Ecker NKJ, Möslein G, Ecker KW (2021) Continent ileostomy: short- and long-term outcome of a forgotten procedure. British Journal of Surgery Open. https://doi.org/10.1093/bjsop en/zrab095
3. Hultén L (1985) The continent ileostomy (Kock’s pouch) versus the restorative proctocolectomy (pelvic pouch). World J Surg 6:952–959. https://doi.org/10.1007/BF01655401
4. Kock NG (1969) Intra-abdominal ‘reservoir’ in patients with permanent ileostomy preliminary observations on a procedure resulting in fecal ‘continence’ in five ileostomy patients. Arch Surg 99:223–231
5. Fazio V, Kiran R, Remzi F et al (2013) Ileal pouch anal anastomosis anastomosis : analysis of outcome and quality of life in 3707 patients. Ann Surg 257:679–685. https://doi.org/10.1097/ SLA.0b013e31827d99a2
6. Denoya PI, Schluender SJ, Bub DS et al (2008) Delayed kock pouch nipple valve failure: is revision indicated? Dis Colon Rectum 51:1544–1547. https://doi.org/10.1007/s10350-008-9350-0
7. Ecker KW, Dinh C, Ecker NKJ, Möslein G (2022) Conversion of ileo-pouch anal anastomosis to continent ileostomy: strategic surgical considerations and outcome. Colorectal Dis 24:631–638. https://doi.org/10.1111/codi.16064
8. Ecker KW, Tönsmann M, Ecker NKJ, Möslein G (2021) Salvage surgery for continent ileostomies (CI) after a first successful revision: more long-term blame on the reservoir than the nipple valve. Int J Colorectal Dis 37:553–561. https://doi.org/10.1007/ s00384-021-04054-x
9. Eberhardson M, Myrelid P, Söderling JK et al (2022) Tumour necrosis factor inhibitors in Crohn’s disease and the effect on surgery rates. Colorectal Dis 24:470–483. https://doi.org/10.1111/ codi.16021
10. Moattar H, Begun J, Florin T (2015) Enteroliths in a Kock continent ileostomy: case report and review of the literature. Endoscopy 47:Suppl 1 UCTN:E200–1. https://doi.org/10.1055/s-0034- 1391302
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is excerpted from the International Journal of Colorectal Disease by Wound World.