Chronic wounds are wounds where the normal healing process has been disrupted at one or more points in the phases of haemostasis, inflammation, proliferation, and remodelling. In these wounds, there is usually an underlying pathology, which produces a delay in the healing process. Some of the pathologies are infection, ischaemia, metabolic conditions, immunosuppression, and radiation (Leveriza-Oh and Phillips, 2012).
Wound infection can lead to the interruption of several processes along the wound healing pathway. Most community-acquired infections are caused by methicillin-resistant Staphylococcus aureus (MRSA) and beta-hemolytic streptococci. Initial antimicrobial choice is empiric and, in simple infections, should cover Staphylococcus spp. and Streptococcus spp (Ramakrishnan et al, 2015).
Bacteria can form a biofilm that goes unrecognised by host cells and is impermeable to most systemic and topical antimicrobials (Andrews et al, 2021). A biofilm develops when microorganisms adhere to and begin to grow on the surface of a wound. Bacteria within a biofilm secrete a glue-like matrix, which allows the biofilm to establish itself more completely on the wound and makes it more resistant to antimicrobial treatment and the patients’ immune system (Percival et al, 2015).
Bacteria also produce inflammatory mediators that inhibit the inflammatory phase and the epithelialisation phase of wound healing. Bacteria in an infected wound causes cell death, leading to an increase in the local inflammation response and prolonged acute inflammatory phase. The presence of necrotic tissue prevents the in-growth of new tissue. In addition, necrotic tissue also serves as a culture for bacterial proliferation, leading to a vicious pathologic cycle (Swezey, 2022).
With the increasing trend in the prevalence of microbial antibiotic resistance, the use of topical antimicrobials has become favoured for infected or open wounds healing by secondary intention. It is imperative for good clinical practices to help in minimising the possibility of bacteria developing resistance to antimicrobial therapies.
To combat the antimicrobial resistance issue, a multimodal approach has been introduced, known as antimicrobial stewardship (AMS) that focuses on prevention of infection and promotion of judicious use of antimicrobials, as well as improving the safety and quality of patient care (Fletcher et al, 2020).
Mupirocin has a wide spectrum of activities against Gram-positive bacteria, including staphylococci and streptococci, and against certain Gram-negative bacteria, including Haemophilus influenzae and Neisseria gonorrhoeae (Roghmann et al, 2021), but is much less active against Gram-negative bacilli and anaerobes. Rode et al (1989) concluded that mupirocin, with its novel mode of action, lack of cross resistance with other antibiotics, active penetration through eschar, and in vivo efficacy, may play an important role in the future treatment of MRSA wound infections.
In this report, we aim to describe a case series of six patients with simple skin and soft tissue infection and a chronic wound that were treated with mupirocin ointment as a topical antimicrobial at the Wound Care Clinic, Kuala Lumpur Hospital, Malaysia.
Methods
Patients attending the Wound Care Clinic, Kuala Lumpur Hospital were recruited by simple randomisation. Their wounds were assessed using the TIME concept (Dowsett and Newton, 2005), and were cleansed with non-toxic cleansers such as a topical disinfectant. If necessary, debridement/desloughing were performed. Mupirocin ointment (Supirocin ointment, Glenmark Pharmaceuticals (M) Sdn Bhd) was applied over the wound bed and covered with a low-adherent absorbent secondary dressing and crepe bandage.
Patients were seen twice a week in the Wound Care Clinic during appointments for dressing, wound bed and wound healing assessment. Digital photography, wound assessment and measurement were documented during every visit for the period of the study. The study period was 2–4 weeks; however, we continued to monitor the wounds to assess the effect of wound bed preparation on healing.
Results
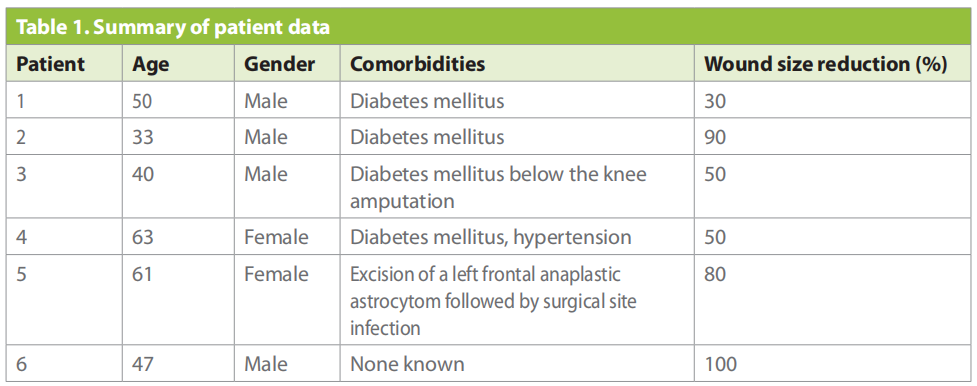
A total of six patients of aged 33 to 63 years old with various wounds, including diabetic foot ulcers and post-surgery wounds (≥10cm2 and ≤100cm2 ) were randomly selected and assessed using the TIME concept. All patients completed the study within the study period and were included in the analysis. A summary of patient data can be found in Table 1. All six patients showed improvement in terms of prevention of infection and biofilm and promotion of wound healing assessed using the TIME concept, with 1 patient achieving wound closure within 4 weeks of treatment (Table1).
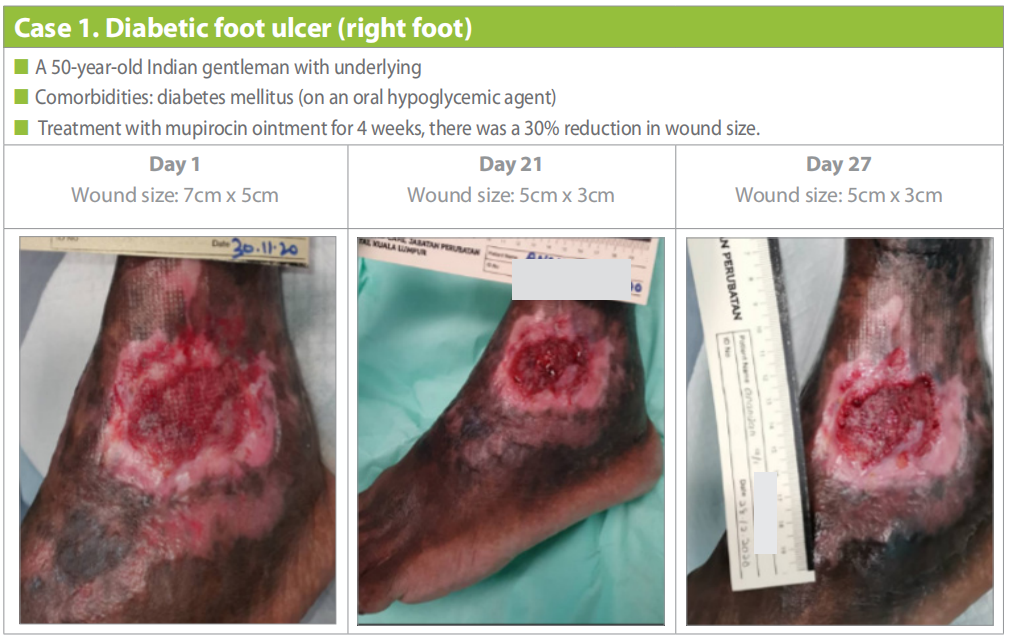
Case 1
A 50-year-old Indian gentleman with diabetes mellitus was admitted with a left diabetic foot ulcer of 27 days’ duration. The patient underwent wound debridement after blisters and pus discharge presented over the lateral aspect of his left ankle in early November 2020.
Following 4 weeks of treatment with mupirocin ointment, the wound had reduced in size from 7cm (length) x 5cm (width) to 5cm (length) x 3cm (width) and increased granulation tissue was observed. The wound bed remained clean throughout the study (Case 1).
Case 2
A 33-year-old Malay gentleman with underlying diabetes mellitus presented with a chronic wound over the dorsum of his left foot following a motor vehicle accident in 2019. He had also sustained left foot compartment syndrome and underwent a fasciotomy in 2019. He had a split-thickness skin graft, but the skin graft became infected and the wound failed to close.
The wound bed was clean following 4 weeks of treatment with mupirocin ointment, with 20% healthy granulation tissue visible by day 12 and up to 80% by day 43. The wound had reduced in size from 7cm (length) x 5cm (width) to 1cm (length) x 1cm (width) and healing had progressed well (Case 2).

Case 3
A 40-year-old Malay gentleman with underlying diabetes mellitus for the past 13 years underwent a below knee amputation in 2018. He presented with a lateral ulcer on the sole of his left foot, which had appeared between July and December 2020. Wound debridement was done once under the orthopaedic team and he was referred to the Wound Care Clinic for further ulcer management.
Following application of the mupirocin ointment, an improvement was noted in terms of granulation tissue growth, reduction in wound size, and thinning of the wound edges. Initial wound size was 5cm (length) x 8cm (width); however, after 3 months of treatment with mupirocin ointment, the wound had reduced in size to 2cm (length) x 5cm (width), a total reduction of 50% (Case 3). Offloading the affected foot was advised and callus debridement was regularly performed.

Case 4
A 63-year-old lady with underlying diabetes mellitus and hypertension had necrotising fasciitis of her left foot in 2012 when debridement was performed. Post-necrotising fasciitis, she had a chronic wound at the dorsum of the left foot. Following treatment with mupirocin ointment, the wound reduced in size and increased epithelialisation was observed by day 31 (Case 4).

Case 5
A 61-year-old lady had an underlying left frontal anaplastic astrocytoma tumour, which was removed by excision surgery in June 2016. This was complicated by a surgical site infection (SSI), post-surgery. The last wound debridement for the SSI was done in September 2017, after which she was free of infection. She first presented to our clinic in March 2020 with pus discharge from the scalp at the surgical site. The scalp infection significantly improved following 15 weeks of treatment with mupirocin ointment (Case 5).

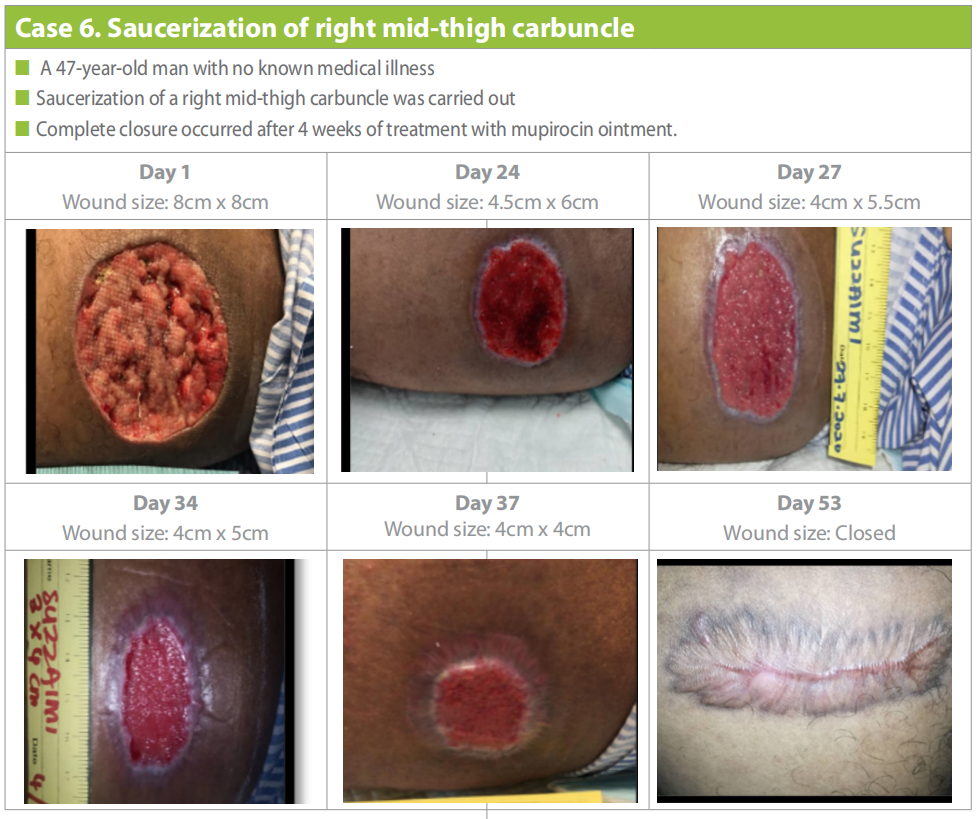
Case 6
A 47-year-old gentleman with no known comorbidities underwent saucerization of a right mid-thigh carbuncle in July 2020. The wound healed significantly following treatment with mupirocin ointment and wound closure occurred after 4 weeks of treatment (Case 6).
Discussion
Increasing evidence has implicated biofilms in at least 70% of chronic infections in humans (Boisvert et al, 2016). Increasing antibacterial resistance, along with insufficient number of antibiotics being developed by the pharmaceutical industry, has made biofilm eradication strategies increasingly important (World Health Organization, 2020). Ha et al (2008) performed a study on drug susceptible isolates of Staphylococcus aureus and allowed them to form biofilms in vitro. They found that topical mupirocin concentrations of 125 μg/ml could reduce Staphylococcus aureus biofilm mass by more than 90%.
A study done by Gilbert et al (1989) showed bacteriologic irradication rates were 97% (30 of 31 patients) in the mupirocin-treated group, compared with 87% (27 of 31 patients) in the fusidic acid-treated group. Another study done by White et al (1989) showed Staphylococcus aureus and/or beta-haemolytic streptococci appeared to be eliminated significantly in more patients treated with mupirocin (96%) compared with those treated with sodium fusidate (88%; p=0.03).
When treatment with topical mupirocin was compared with oral antibiotics in skin infections in general practice, mupirocin ointment cured 86% and improved 13% (Villiger et al, 1986). This was significantly better than erythromycin (47% cured, 26% improved) and similar to flucloxacillin (76% cured, 23% improved).
Conclusion
In this study, all six patients showed improvement in terms of prevention of infection and biofilms and promotion of wound healing by reduction in the bacterial bioburden. Out of six patients, only one achieved wound closure within four weeks of treatment, the others had a reduction in wound size, an increase granulation tissue and no signs of infection. Hence, it can be suggested that topical antimicrobial mupirocin ointment helps to promote wound healing and treats wound infection.
References
1. Andrews KL, Derby KM, Jacobson TM et al. Prevention and management of chronic wounds. Cifu DX (ed): In Braddom’s Physical Medicine and Rehabilitation (6th edn), 2021
2. Fletcher J, Edwards-Jones V, Fumarola S et al (2020) Best Practice Statement: Antimicrobial stewardship strategies for wound management. Wounds UK, London
3. Dowsett C, Newton H (2005) Wound bed preparation: TIME in practice. Wounds UK. 1(3):58–70. https://tinyurl.com/ yckwazwt (accessed 10.05.2022)
4. Ha KR, Psaltis AJ, Butcher AR et al (2008) In vitro activity of mupirocin on clinical isolates of Staphylococcus aureus and its potential implications in chronic rhinosinusitis. Laryngoscope 118(3):535–40. https://doi.org/10.1097/ mlg.0b013e31815bf2e3
5. Leveriza-Oh M, Phillips TJ (2005) Dressings and postoperative care. Surgery of the Skin:117–35. https:// doi.org/10.1016/b978-0-323-02752-6.50013-4
6. Percival SL, McCarty SM, Lipsky B (2015) Biofilms and wounds: an overview of the evidence. Adv Wound Care (New Rochelle) 4(7):373–81. https://doi.org/10.1089/ wound.2014.0557
7. Ramakrishnan K, Salinas RC, Higuita NIA (2015) Skin and soft tissue infections. Am Fam Physician 92(6):474–83. https://www.aafp.org/afp/2015/0915/p474.html
8. Rode H, Hanslo D, de Wet PM et al (1989) Efficacy of mupirocin in methicillin-resistant Staphylococcus aureus burn wound infection. Antimicrob Agents Chemother 33(8):1358–61. https://doi.org/10.1128/aac.33.8.1358
9. Roghmann MC, Lydecker AD, Shardell M et al (2021) Effect of mupirocin for Staphylococcus aureus decolonization on the microbiome of the nose and throat in community and nursing home dwelling adults. PloS one 16(6):e0252004
10. Swezey L (2020) Necrotic wounds: Overview and treatment options. WoundSource. https://www.woundsource.com/ blog/necrotic-wounds-overview-and-treatment-options (accessed 24.04.2022)
11. Villiger JW, Robertson WD, Kanji K et al (1986) A comparison of the new topical antibiotic mupirocin (‘bactroban’) with oral antibiotics in the treatment of skin infections in general practice. Curr Med Res Opin 10(5):339–45. https:// doi.org/10.1185/03007998609111100
12. White DG, Collins PO, Rowsell RB (1989) Topical antibiotics in the treatment of superficial skin infections in general practice—a comparison of mupirocin with sodium fusidate. J Infect 18(3):221–9. https://doi.org/10.1016/ s0163-4453(89)80058-1
This article is excerpted from the Wounds Asia 2022 | Vol 5 Issue 1 | by Wound World.


