Foot complications from diabetes are one of the main causes of lower limb amputation, with enormous medical, functional, and emotional consequences (Goodridge et al, 2005; Lincoln et al, 2008; Chen et al, 2011; Yao et al, 2012). Diabetes-related lower extremity conditions like peripheral neuropathy, peripheral vascular disease and infection, further increase the risk of amputation (Boulton, 1996; Sharoni et al, 2017). Peripheral neuropathy causes sensation loss in the feet, thus patients with sensory neuropathy may fail to perceive foot problems and they will be more susceptible to foot deformities and ulceration. People with diabetes mellitus are 10–15 times more likely to receive lower extremity amputation than non-diabetic individuals (Van Houtum, 1997). Furthermore, lower extremity amputation is associated with high morbidity and mortality (Abdullah and Abdullah, 2010; Li et al, 2014; Muhammad-Lutfi et al, 2014; Ahmad Sharoni et al, 2017), 40.7% of patients became institutionalised after having an amputation (Lavery et al, 2003; Murray et al, 2005; Singh et al, 2005; Wong, 2005). The suboptimal outcome poses a heavy health and socioeconomic burden on the healthcare resources and society.
To tackle this the by World Health Organization (WHO) announ2ced its Global Diabetes Compact (2020a), which will bring together in one package all WHO materials for the prevention and management of diabetes. Before the COVID-19 pandemic 420 million people suffered from diabetes (World Health Organization, 2020b) and the number is expected to rise to 700 million by year 2045.
Demand for long-term health care is growing rapidly and one of the most serious challenges facing the healthcare systems is how to empower and engage the public in chronic disease management.
Statistics showed that the incidence of diabetic foot ulcers (DFU) and rate of amputation was on an increasing trend over the past decade (Bekele and Chelkeba, 2020). In an article reviewing 35 published papers between January 1966 and October 2005 describing the trends and differences in prevalence of people with type 2 diabetes, the percentage of undiagnosed diabetes of local population was 52.6% (95% confidence interval: 49.8% to 55.5%; Wong and Wang, 2006). Patients’ awareness to try and stop the rising trend in prevalence of diabetes is of the utmost importance, otherwise, a tremendous increase in burden caused by diabetes will be seen (Wong and Wang, 2006). With the increasing number of people with diabetes and prolonged life expectancy, it was estimated that by 2025, 12.8% of the local population, representing more than 1 million people will suffer from the disease (Lewis, 1995). Reviewing the cases admitted to our orthopaedic wards from January 2018 to March 2018, a total 55 patients were admitted due to DFUs and chronic wound management. The mean age of patients was 70.4 years old (range: 39–97), and 63% of these patients have diabetes-associated conditions. In this group, 23% required surgical debridement and over 46% ended up with an amputation. According to the statistics listed in a review, the proportion of “younger” patients, aged under 60, receiving amputation is greatly increased, from 17% to 42% (Muhammad-Lutfi et al, 2014). Impacts of diabetes-associated conditions for both economic and social implications are, as demonstrated, significant. A well-designed and evidenced-based foot care programme is essential to increase public awareness.
The public awareness of diabetic foot care is low (Dixit et al, 2011; Muhammad-Lutfi et al 2014). At present practice in wound care offers routine wound care support from designated community health centres and self-dressing at home, with regular clinic follow-ups, which are months apart. Introducing the mobile phone application (mobile app) targeting DFU patients, they can report any issue with their feet/wounds by taking pictures or sending a message to an orthopaedic surgeon who specialises in the foot and ankle. This kind of patient feedback mechanism provides timely professional care without further delay.
E-health has a proven role in the selfmanagement of chronic diseases and has a positive effect on self-efficacy, continuous behavioural and clinical outcomes among patients with chronic diseases (Murray et al, 2005; Kerr et al, 2005; Wang et al, 2014). The popularity of using smartphone in older generations transforms the e-health experience to tip-to-healthcare through a mobile phone application (Lin et al. 2020). Self-surveillance and direct feedback on DFU management would be useful to patients with diabetes.
Aim
The objectives of this study are 1) to introduce the mobile phone application specific for patients with DUFs 2) to assess the change in health-related quality of life (HRQOL) outcomes of the participants before and after using the mobile app using Diabetes Foot Self-Care Behaviour Scale (DFSCB).
Materials and methods
A mobile app “Happy Feet” was developed that included functions suitable for patients with a DFU foot ulcer including:1) Self-care educational materials in video format, 2) Information on diabetic foot care by electronic version of a pamphlet and information on future educational talks, 3) Self-administered HRQOL questionnaire.
The target sampling population was the patients visiting the weekly diabetes clinic in a tertiary hospital, although everyone could download the mobile app onto their mobile phones. Subject inclusion criteria were male or female subjects over the age of 18, individuals with diabetic foot and mobile phone users; and the exclusion criteria were non-consenting patients who had not provided the written informed consent, and pregnancy or breast-feeding.
Ethics approval was obtained from the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee (Approval No: 2017.657). The study protocol followed the Declaration of Helsinki and ICH-GCP. Informed consent and an educational pamphlet were explained and signed before patient recruitment. The mobile app was launched in November 2016 and started recruiting patient at the clinic at the same time. An educational talk in an old age home was held after six months to raise the community awareness of the use of the mobile app. The mobile app is still running through now, although the data collection was stopped in March 2019 for reporting purposes.
Inside the mobile app – “Happy feet”
The mobile app contained medical information related to DFUs. The information was taken from the National Diabetes Education Program (NDEP) “Feet Can Last a Lifetime” proposed by the National Institutes of Health (NIH) and the Centres for Disease Control and Prevention (National Diabetes Education Program, 2000). Briefly, the medical information contained the following:
Self-care knowledge and behaviour
Education of diabetes management
Prevention of foot ulcers
Foot caring tips and guide for good footwear
Self-care video for a Healthy diet.
The user interface was simple and suitable for middle to older aged patients. The mobile app targeted at both patients and their carers.
Educational pamphlet and talk
Every patient with diabetes suffering from a foot ulcer received a pamphlet when they visited the clinic. The pamphlet titled “Foot care for diabetic patients” contained the following information: causes of diabetic foot, diabetic foot care, and choosing suitable socks. Links to download the mobile app was also included.
A health education talk was held, aiming at promoting community primary health care using the mobile app. The health talk targeted diabetic foot sufferers, their family members, their carers, as well as health professionals including doctors and nurses.
The Diabetes Foot Self-Care Behaviour Scale (DFSBS)
DFSBS evaluated the participants’ foot selfcare behaviour through seven questions. Part 1 consisted of four questions that were on a 7-point Likert scale, asking for the number of days, in the last seven days, they carried out different kinds of foot care. In part 2 three questions, on a 5-point Likert scale, asked about the frequency patients or carers carried out foot care.
The answers of the four questions were modified following patients’ suggestions. The answers in Part 1 changed to the same choices in part 2 with the following changes: “Never” in part 2 corresponded to “0 day” in part 2, likewise “Seldom” corresponded to every “1–2 days”, “Sometimes” corresponded to every “3–4 days”, “Frequent” to every “5–6 days” and “Always” to “7 days” i.e everyday.
Data collection
Data, from subjects with confirmed diabetes either recruited at the diabetes clinic or at the educational talk was collected. They completed DFSBS the first time on the day of study recruitment, and after three and six months through telephone interviews.
Data analysis
The number and percentage of patients answering the seven questions at the three time points (baseline, post-3 months and post-6 months) was tabulated. Chi-square tests were carried out to look for any statistical difference among the three time points. Mean and standard deviation of scores of individual questions and total scores were also calculated and compared among the 3 time points using One-way ANOVA. A line chart graphically representing the changes in mean scores was plotted. Data analysis were carried out using IBM SPSS 26.0 (Armonk, New York). A two-sided p≤0.05 was considered statistically significant.
Results
A total of 301 questionnaires received from 151 patients suffering from diabetes who entered the study at baseline. There were 79 patients who completed the questionnaire after three months, and 71 patients completed the questionnaire after six months. The mean age of patients was 67.8 (range: 51 to 82).
The attitudes of patients with diabetes to foot care changed over time. The percentage of patients who never examined the bottom of their feet or toes, dried the toes after washing, applied lotion, checked the inside of the shoes, and broke in new shoes slowly to avoid skin damage significantly decreased from baseline and three months, to six months, indicating better foot care behaviour over time (Table 1). Patients significantly increased the time spent on foot care, performing tasks on 5–6 days of the week after 3 months. After six months the patient spent time performing these tasks on 3–6 days of the week. The frequency that patients or the caregivers examined the bottom of their feet had changed from either none (25.8%), 3–4 days of the week (21.2%) or all 7 days of the week (21.9%). All comparisons showed statistically significant (p<0.01).
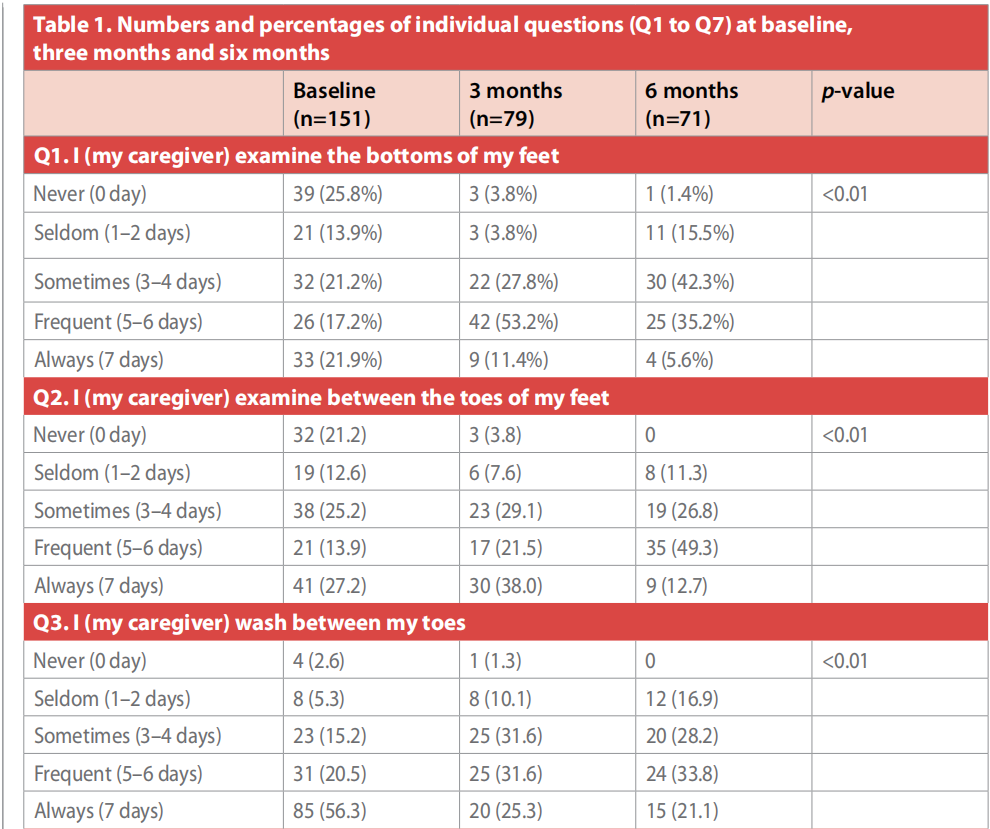
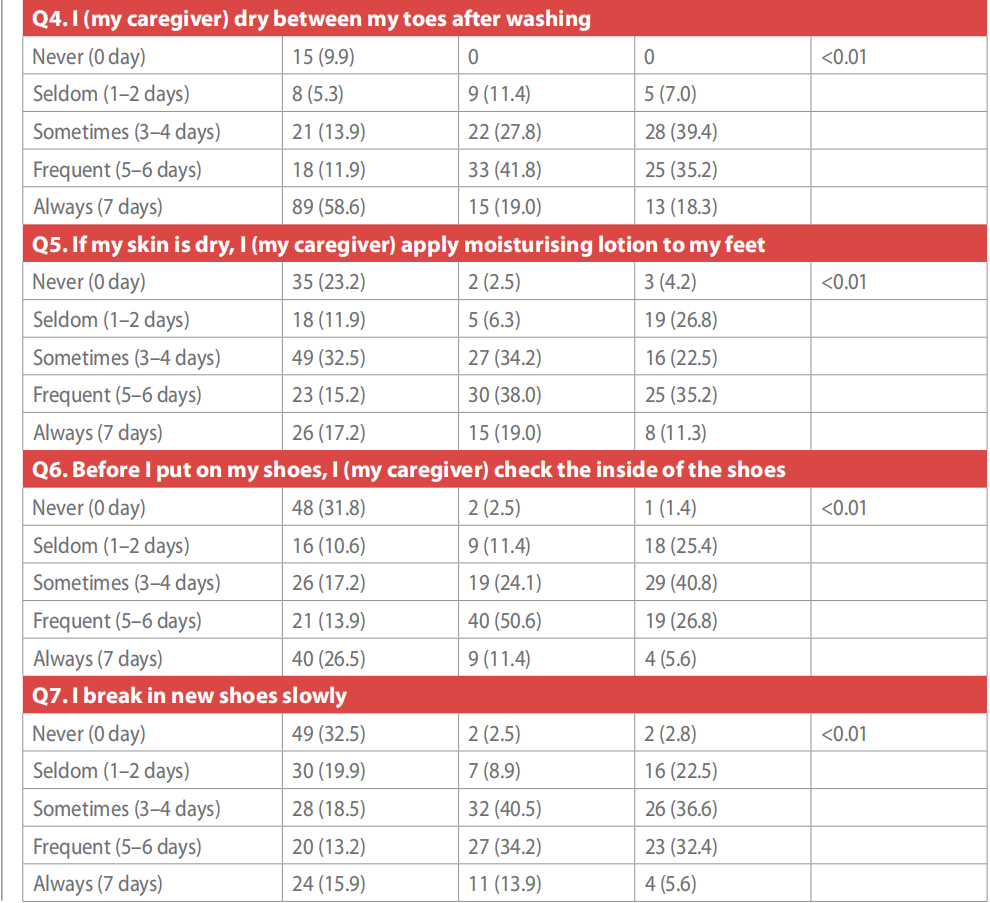
Significant differences in frequency of care after three months and six months were also observed (Table 2). Mean total scores of individual questions and total scores were significantly increased between baseline and three months in all questions, except “wash between my toes” and “dry after washing”. After six months, mean scores were increased in “examining between the toes” and “breaking in new shoes slowly”. Mean scores in “washing between toes” and “dry between toes after washing” were decreased at six months. No significant difference was found when comparing between three months and six months. Mean total scores in three months were significantly higher than baseline (p<0.01) (Figure 1).
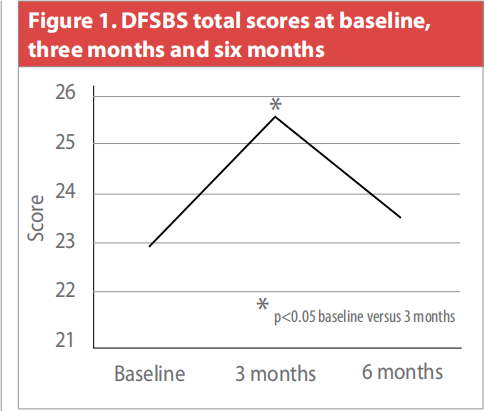
The total scores of DFSBS increased from 22.80 at baseline to 25.54 at post-3 months and dropped to 23.63 at post-6 months.
Discussion
All study subjects confirmed the diagnosis of diabetes mellitus type 1 or 2. This study aimed to determine the variability of selfcare diabetes foot assessment patterns using the “Happy Feet” mobile app. The concept of e-health through the mobile app promoted self-checking of their DFU. The results from DFSBS showed significant improvements in self-care behaviour assessment of individual foot through baseline, post-3 month and post-6 month. Statistical differences were found in all questions suggesting the mobile app offered substantial supports on their self-care behaviour. Our results were similar to previous studies.
The total scores of DFSBS increased from baseline to post-3 months and the dropped a little post-6 months. Our findings are similar to earlier studies, in which the total scores ranged from 20.82 to 25.37 (Wong and Wang, 2006). At baseline, the highest total score was found in Q3 (I wash between my toes), which was also comparable with previous studies (Abdullah and Abdullah, 2010, Muhammad-Lutfi et al, 2014). Toe washing habit ranked top could be a seasonal issue. The educational talk, aiming at promoting the use of mobile app, was held in April, in the study region spring is hot and humid and people tends to bath more often. Moreover, some participants having persistent ulcer on their feet were advised by doctors and nurses to clean and wipe their inner toes daily.
Apart from cleaning the inner toes more frequent, participants were more likely to aware of their bottoms of their feet, between the toes, drying between the toes, moisturising the feet, checking the shoes inside and wearing in new shoes slowly. Raising the effectiveness of self-care in patients with DFUs and their carers using a mobile app was proven useful and sustainable. The mobile app comes with selfmanagement knowledge provided by medical specialists, which was also proven useful. The inapp questionnaire survey continuously provides the easiest way for patients or carers to reflect their motivations, in terms of frequency, and monitors the HRQOL of the patients closely.
Another important finding from this study is that the e-health delivered by a mobile app is proven feasible and possible. Policymakers can obtain up-to-date information on patients with DFUs through the mobile-based evidencebased platform, allowing allocation of exact resources and funding to aid this patient population. In terms of the medical sector, doctors and nurses provide timely support to the patients. That would possibly reduce the chance of the symptoms getting worse or delayed wound management subsequent to amputation. Hospital resources can be revisited and reallocated. The in-app educational materials provide the most accurate source of information on DFU care. This is important to provide evidence-based information to the patients to avoid conspiracy through social media or web search engines. Much information is inaccurate and non-scientific, which may lead to delayed DFU treatment.
The mobile app has the unique features that standout from similar apps, and it is designed for both patients and caregivers. Patients and caregivers can access the evidence-based orthopaedic related information from a team of orthopaedic specialists. Nowadays, related information can be easily accessible through the internet and mobile devices, but the information are not always accurate. Information provided in printed matter, electronic version, and video materials prepared by sponsors or certain health-care companies are sometimes incorrect and biased. Our mobile app includes a self-administered HRQOL questionnaire (DFSBS) that can let orthopaedic specialists evaluate how well the patients or caregivers take care of the diabetic foot. This is to maintain their quality of life by reducing the amputation rate due to negligence, delay or mismanagement of their wound. Introducing the electronic version of DFSBS allows patients to provide instant feedback to the orthopaedic specialists and the orthopaedic specialists can promptly investigate further any concerns avoiding delayed responses. The ultimate goal is to act as an alternative channel for patients with diabetes to interact with medical personnel in a pro-active manner.
The mobile app targets for patients of all ages and caregivers. Their education level and social status of patients, caregiver, and general public can be largely diverse, therefore, we aim at accessing the useful materials in several tabs and swipes. We also evaluate the readibility of the materials to make sure the contents in the materials are understandable for lay users.
Data protection and security are always our concerns. Data is encrypted by standard encryption algorithm (AES, DES). A secured connection is used to protect the communication between the application and the server. All data is stored in our local server. All data stored on the server were encrypted. All users are requested to login before reviewing.
The rolling out of this mobile app means much to the people with diabetes living in community settings. The roll out also aims to reduce the cost on public hospital resources by lowering the incident of surgical management of DFUs and encouraging patients’ independence in disease management. We recommend institutes adopting this mobile app work together and share their experience and data in order to provide better wound management in patients with diabetes through different levels of collaborations.
Limitations
Limitations were inevitably found in this study. This study employed convenience sampling method which means the sample population may not be representative of the entire diabetic population. Similar to other studies, the diabetes foot self-care behaviour scale is predominantly relied on self-reported memory of past behaviours, which subject to recall and reporting biases. A majority of our study participants were treated by inpatient or outpatient care in tertiary hospitals. This healthcare umbrella may be different from the general population which may make the data not entirely generalisable to other populations.
Conclusions
Through a mobile phone application, the self-care behaviour (aware of their bottoms of feet, between the toes, drying between the toes, applying moisturising the feet, checking the shoes inside and wearing in shoes slowly) of diabetes mellitus patients suffering from foot ulcers substantially increased after three months using the application. It was still increased after six months compared with the day of recruitment/starting to use the application. The mobile app contains educational materials that provide evidencebased information different from unreliable sources, such as social media or search engines. Both policymakers and medical professionals will benefit from the mobile app providing accurate and correct information to this group of patients.
Acknowledgements
This study is funded by the HCPF: HCPF (Project No.: 29150514). 1. The Evangelical Lutheran Church of Hong Kong Sheen Hok Charitable Foundation Kwan Shon Hing Yu Chui Neighbourhood Elderly Centre 2. The Hong Kong Society for Rehabilitation.
Declaration of interest
All authors declared no conflict of interest.
Appendices
Further details on the application and educational videos can be obtain by contacting the editor.
References
1. Abdullah MAH, Abdullah AT (2010) Annual report of National Orthopaedic Registry Malaysia (NORM) Diabetic Foot 2009. https://tinyurl.com/8pdxby24 (accessed 8 October 2021)
2. Ahmad Sharoni SK, Mohd Razi, MN, Abdul Rashid NF Mahmood YE (2017) Self-efficacy of foot care behaviour of elderly patients with diabetes. Malays Fam Physician 12(2):2–8
3. Bekele F, Chelkeba L (2020) Amputation rate of diabetic foot ulcer and associated factors in diabetes mellitus patients admitted to Nekemte referral hospital, western Ethiopia: prospective observational study. J Foot Ankle Res 13(1):65. https://doi.org/10.1186/s13047-020-00433-9
4. Boulton AJ (1996) The pathogenesis of diabetic foot problems: an overview. Diabet Med 13 Suppl 1:S12–6
5. Chen MY, Huang WC, Peng YS et al (2011) Effectiveness of a health promotion programme for farmers and fishermen with type-2 diabetes in Taiwan. J Adv Nurs 67(9):2060-7
6. Goodridge D, Trepman E, Embil JM (2005) Health-related quality of life in diabetic patients with foot ulcers: literature review. J Wound Ostomy Continence Nurs 32(6):368–77. https://doi.org/10.1097/00152192- 200511000-00007
7. Kerr C, Murray E, Stevenson et al (2005) Interactive health communication applications for chronic disease: patient and carer perspectives. J Telemed Telecare 11 Suppl 1:32–4. https://doi.org/10.1258%2F1357633054461912
8. Lavery LA, Armstrong DG, Wunderlich RP et al (2003) Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care 26(5):1435–8. https:// doi.org/10.2337/diacare.26.5.1435
9. Lewis GF (1995) Diabetic dyslipidemia: a case for aggressive intervention in the absence of clinical trial and cost effectiveness data. Can J Cardiol 11 Suppl C:24c–28c
10. Li R, Yuan L, Guo, X-H et al (2014) The current status of foot self-care knowledge, behaviours, and analysis of influencing factors in patients with type 2 diabetes mellitus in China. International Journal of Nursing Sciences 1(3):266–71. https://doi.org/10.1016/j.ijnss.2014.05.023
11. Li, TTC, Bautista JR, Core R (2020) Seniors and mobiles: A qualitative inquiry of mHealth adoption among Singapore seniors. Inform Health Soc Care 45(4):360–73. https://doi.org/10.1080/17538157.2020.1755974
12. Lincoln NB, Radford KA, Game FL, Jeffcoate WJ (2008) Education for secondary prevention of foot ulcers in people with diabetes: a randomised controlled trial. Diabetologia 51(11):1954–61. https://doi.org/10.1007/ s00125-008-1110-0
13. Muhammad-Lutfi AR, Zaraihah MR, Anuar-Ramdhan IM (2014) Knowledge and Practice of Diabetic Foot Care in an InPatient Setting at a Tertiary Medical Center. Malays Orthop J 8(3):22–6. https://dx.doi.org/10.5704%2FMOJ.1411.005
14. Murray E, Burns J, See TS et al (2005) Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev (4):CD004274. https:// doi.org/10.1002/14651858.cd004274.pub4
15. National Diabetes Education Program (2000) Feet Can Last a Lifetime: A Health Care Provider’s Guide to Preventing Diabetes Foot Problems, National Diabetes Education Program https://tinyurl.com/vxx9njy8 (accessed 8 October 2021)
16. Sharoni SKA, Abdul Rahman H, Minhat HS et al (2017) A selfefficacy education programme on foot self-care behaviour among older patients with diabetes in a public long-term care institution, Malaysia: a quasi-experimental pilot study. BMJ Open 7(6):e014393. https://doi.org/10.1136/ bmjopen-2016-014393
17. Singh N, Armstrong DG, Lipsky BA (2005) Preventing foot ulcers in patients with diabetes. JAMA 293(2):217–28. https://doi.org/10.1001/jama.293.2.217
18. Lavery LA, Van Houtum WH, Armstrong DG (1997) Institutionalization following diabetes-related lower extremity amputation. Am J Med 103(5):383–8. https://doi. org/10.1016/s0002-9343(97)00163-0
19. Wang J, Wang Y, Wei, C, et al (2014) Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health 20(6):570–83. https:// doi.org/10.1089/tmj.2013.0243
20. Wong KC, Wang Z (2006) Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract 73(2):126–34. https://doi.org/10.1016/j.diabres.2006.01.007
21. Wong MW (2005) Lower extremity amputation in Hong Kong. Hong Kong Med J 11(3):147–52
22. World Health Organization (2020a) WHO announces the Global Diabetes Compact [Online]. https://tinyurl. com/25y44jcv (accessed 6 October 2021)
23. World Health Organization (2020b) Coronavirus disease (COVID-2019) situation reports: Situation report - 52 [Online]. https://tinyurl.com/2f8wdf6k (accessed 6 October 2021)
24. Yao H, Ting X, Minjie W et al (2012) The investigation of demographic characteristics and the health-related quality of life in patients with diabetic foot ulcers at first presentation. Int J Low Extrem Wounds 11(3):187–93. https://doi.org/10.1177/1534734612457034
This article is excerpted from the Wounds Asia 2021 | Vol 4 Issue 3 | by Wound World.