Introduction
Since the appearance of highly active antiretroviral treatments (HAART) the process of HIV/AIDS becoming a chronic disease in the industrialised world has led to a dramatic change in the illness paradigm [1]. Patients who would previously have been terminally ill are now chronically ill, and palliative care has become chronic care [2,3]. This situation requires a completely new approach to care of the HIV/AIDS patient.
For patients, a chronic disease course means visiting their hospital every three months, first to perform a blood test, second for the follow-up appointment and, finally, to collect their medication from the hospital pharmacy. This clinical routine can interfere with patients’ attempts to return to normality in their daily lives, and may create problems with employers due to work absences [4,5]. In addition, patients need to be closely monitored in order to maximise their adherence to medication, and therefore prevent the development of resistance.
For the infectious diseases physician the follow-up of a chronic HIV patient has become easier, because these patients are relatively young, show few comorbidities and do not require complex monitoring, simply a blood test and routine appointments every three months to check on results.
However, there is still no cure for the infection and the number of chronic HIV-infected patients is increasing year by year, thereby placing greater demands on healthcare systems. As a result there is a need to optimise health resources, both in terms of infrastructure and staffing levels.
In this regard, ideas about how to approach this situation may be gained by looking at other chronic diseases such as diabetes [6–9], chronic obstructive pulmonary disease [10–12] or congestive heart failure [13–15], which have made use of telemedicine for several years now. Research has shown that a multidisciplinary management programme and home-based intervention can reduce hospital readmission rates and length of hospital stay in patients with chronic cardiac disease [16–18], as well as improving their quality of life [19–21]. In the case of diabetes, telemedicine allows the frequent transmission of blood glucose values to healthcare providers, thereby enabling them to modify the medical regime and/or diet so as to improve metabolic control [22–25].
Telecare involves the delivery of health and social care to individuals within the home or wider community, with the support of systems enabled by information technology [26]. It introduces new forms of assessment designed to improve the quality and variety of information which clinicians have about a patient’s health status. Measures of functional status and quality of life, in addition to physiological monitoring, can be translated into accurate predictors of health risk, and they can be combined with electronic alarm systems to initiate an appropriate course of action. This information is invaluable in identifying and treating problems, sometimes at an earlier stage [27].
A further aspect is that the coordination of the care team and the involvement of patients in their own care [28] seem to be factors of great importance for good chronic disease management [29]. A multidisciplinary care team is also desirable in a disease such as HIV/AIDS, where psychological and social factors have an increasing influence on a patient’s health status. Indeed, chronic care requires a holistic model that integrates doctors, psychologists, nurses, social workers and pharmacists into the same team, of which the patient should also be seen as a member [30].
Telemedicine is attractive to physicians because it offers them the possibility of reaching all those patients who need their advice regardless of distance, while the appeal to patients is that it gives them a greater access to health care. Naturally, both groups prefer the face-to-face consultation whenever possible, but consultations can sometimes be offered through a form of telemedicine, which is more convenient, cheaper, less time-consuming and may be equally satisfactory for both parties. Furthermore, telemedicine may reduce the patient’s travelling time and absence from work, thereby decreasing the overall societal costs.
Given the current situation facing patients and health providers, and the enormous possibilities offered by the internet, we developed a telemedicine service to complement standard care. Specifically, this involved a telecare follow-up for stable HIV-infected patients in the chronic phase of their disease. The present study evaluate the home care provided by this telemedicine system called Virtual Hospital, comparing standard care received by HIV-infected patients with Virtual Hospital care. The objective of the study is to demonstrate that Virtual Hospital could improve and facilitate the access of the patients to the health system without any deleterious effect on their care. The technical structure of the system has already been published in several telemedicine journals [31,32].
Methods
An open-label, two-arm, prospective randomised study was performed between January 2005 and December 2007 in a university hospital in Barcelona. Participants were 3500 HIV outpatients. The protocol for this trial and supporting CONSORT checklist are available as supporting information; see Checklist S1 and Trial Protocol S1.
The main goals were the definition, development, clinical routine installation and evaluation of a telemedicine service that compares standard care with telecare follow-up for stable HIV-infected patients in the chronic phase of their disease. The study was approved by the local Human Research Ethics Committee. Patients signed written informed consent and were randomised (with balanced randomization [1:1] through a computer generated randomization list without any restriction) to either: Arm I, where they were monitored virtually via the internet during the first year of follow-up; or arm II, where they were monitored in the day hospital via standard care. After one year of follow up, patients switched their care to the other arm.
Standard Care in a stable HIV infected adult consists firstly in to perform a blood test (to assess biochemical parameters, CD4 T cells, HIV-1 viral load) 15 days before the day of consultation in the Infectious Diseases Day Care Hospital (laboratory needs 2 weeks to have all the results of the blood test performed). Secondly, the infectious disease physician during consultation, checks the analysis, asks about any clinical change and expends antiretroviral prescriptions if the patient is treated. Thirdly, patient goes with the antiretroviral prescription to the hospital Pharmacy to perform a visit with the pharmacist to check antiretroviral compliance and finally to collect the drugs. The patient repeats this clinical routine every 3–4 months.
The telecare system, Virtual Hospital, offered integrated online patient monitoring by a multidisciplinary care team (nine infectious diseases specialists, three nurses, one psychologist, one psychiatrist, three pharmacists and one social worker), allowing the patient to be remotely followed-up by these professionals and have access to their own clinical and pharmaceutical files. See test web http://web.gbt.tfo.upm.es/clinic/login.asp.
Inclusion criteria were stable patients (CD4 .250 cells/mm3 during at least the three months prior to inclusion to the study) who had access to a computer and to broadband. No other specific demographics (risk groups, educational level and nationality) or clinical characteristics (hepatitis B or C coinfection) were considered selection criteria. Exclusion criteria were HIV-infected adults with current therapeutic failure (defined by detectable viral load on treatment or CD4 cell count ,250 cells/ml), tumours, opportunistic infections, or pregnant women.
The architecture of this web-based system had two parts. The first was the hospital infrastructure, where we added our server to the existing demilitarised zone (DMZ) of the hospital, which was protected by a firewall and integrated into the hospital’s information system network. Health professionals accessed this server via the hospital’s intranet. The second part was the home infrastructure, where the patient accessed the server via a basic broadband connection and, for security reasons, through a virtual private network (VPN) (Figure 1). Of critical importance in the system was the connection of the server with three databases. The Virtual database was the new database created for the telemedicine system, where the data of patients involved in the trial were stored. This database was filled and synchronised with the HIV/ AIDS database, which the Infectious Diseases Service of the Hospital Clinic has been using over the last twenty years; this database includes the records of over 5,000 HIV/AIDS patients. Finally, the server was also connected to the pharmacy database, where all the available drugs and data related to antiretroviral compliance were recorded.
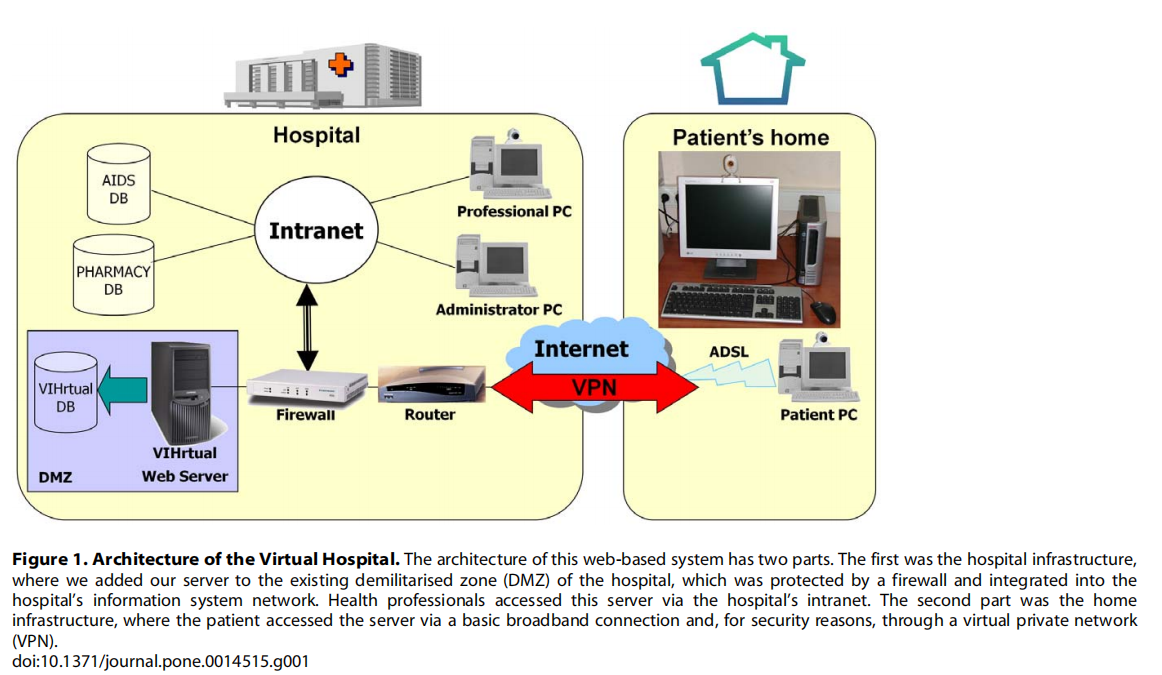
The graphical interface was carefully designed in order to make it user friendly for both professionals and patients. Another main goal was to develop a low-cost system so as to enable an increased number of patients to be offered such care in the future. This is why low-cost, home web cams and broadband were some of the chosen technologies for the implementation. Security was one of the most carefully designed aspects of the project, mainly because of its experimental nature and due to the characteristics of the disease in question. As well as securing the communications, via VPN tunnelling, patient data were also encrypted and all personal identification data were removed. A completely separate tool was developed outside the web system, so that only the system administrator would have access to it. All access to the system was monitored, and the system automatically sent an alert e-mail to the technical manager in the event of recurrent access. More technical information about Virtual Hospital has been previously reported [31,32].
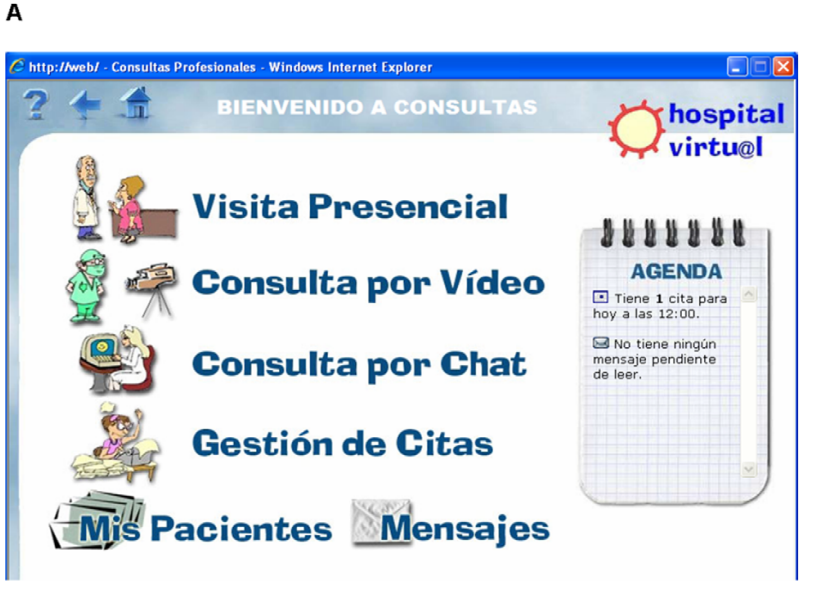
Virtual Hospital offered four main services: Virtual Consultations, Telepharmacy, Virtual Library and Virtual Community.
Virtual consultations had two levels: first, appointments/consultations conducted via videoconferencing; and second, chat sessions or message exchanges for emergency or off-schedule consultations. During any of these sessions the Electronic Health Record was available to both professionals and patients (see Figure 2). However, whenever patients wish it, in addition to the virtual consultations they might have an in-person consultation with the health professionals. It should be noted that psychological and social data were also integrated into the patients’ records. An electronic diary was also available so that at the end of the appointment, the patient and the professional could set a time for the next one.
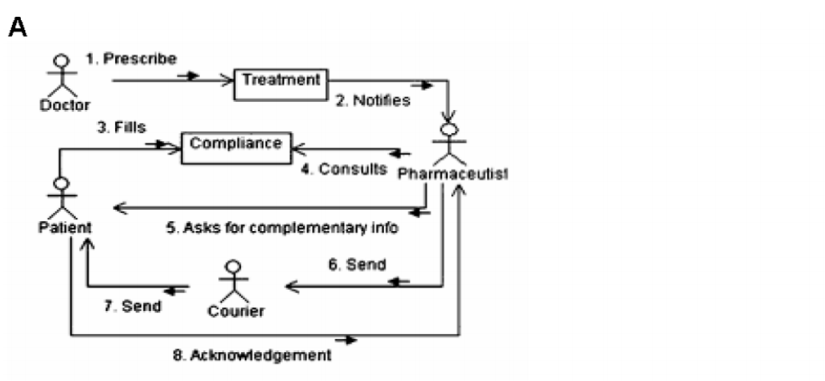
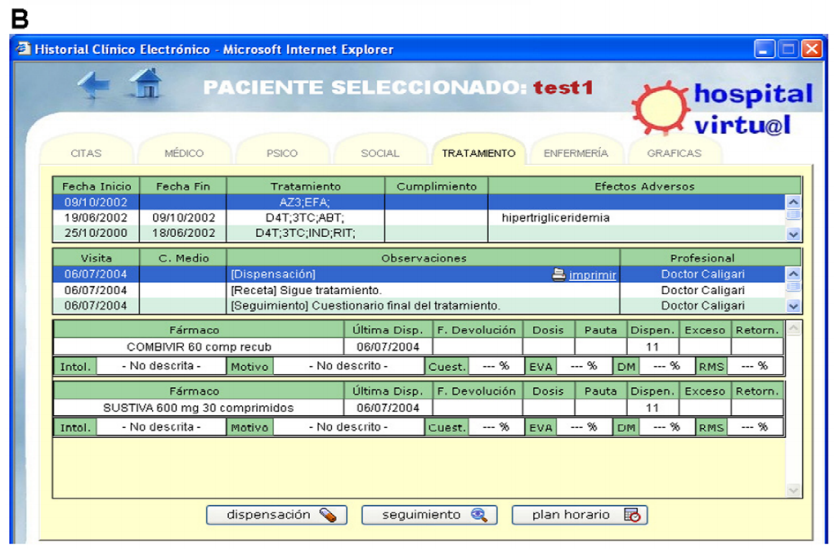
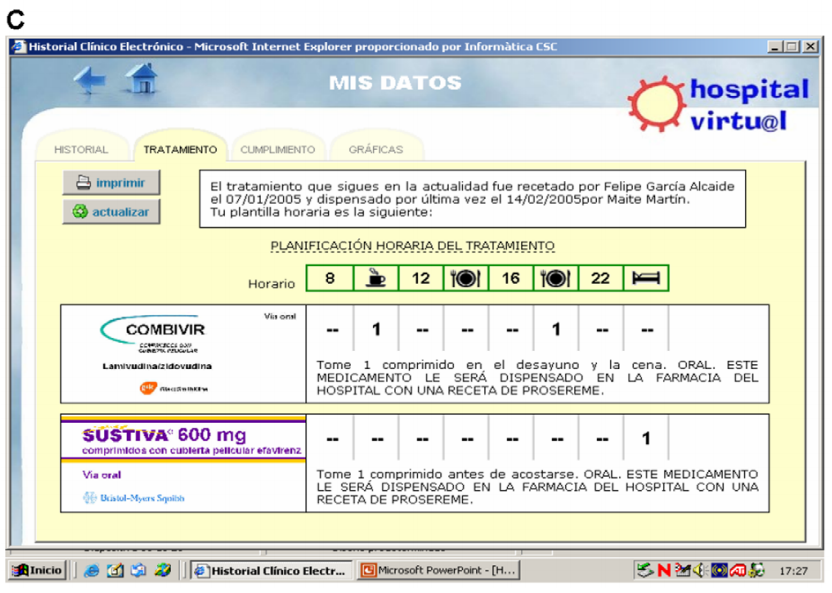
Telepharmacy allowed the pharmacist to receive electronic prescriptions, to perform virtual consultations about compliance, adverse events or interactions, and to send the antiretroviral medication to the patient’s home by courier. The standard care in our centre is that patients take their antiretroviral prescriptions to the hospital pharmacy, where the pharmacist sees the patient, checks whether he/she is having any problems with treatment, and dispatches the drugs (in Spain antiretroviral drugs are given out exclusively in hospital pharmacies). The telepharmacy system enabled patients to track the evolution of their treatment on charts and consult basic information regarding the available antiretroviral drugs. The new process and the telepharmacy system are shown in Figure 3.
Virtual library stored validated information about HIV as links to other web pages, for both patients and professionals. All links were categorised by their type of source and were included in different groups according to the subject they referred to.
Virtual community provided space to exchange information about the disease and the project, as well as to share opinions or comment on articles and news items. The information offered by this tool differed according to the user (i.e. healthcare professional or patient). Exclusive to professionals was the clinical session option, where they could share opinions about the cases they were responsible for at the time.
A brief twenty-minute introduction to the system’s functioning was offered to both professionals and patients prior to starting the study. An external company was hired to help patients with any technical problems involving hardware or software (patients had a telephone number to call in such cases). This company resolved most of the problems by telephone, but when necessary a technician went to the patient’s house.
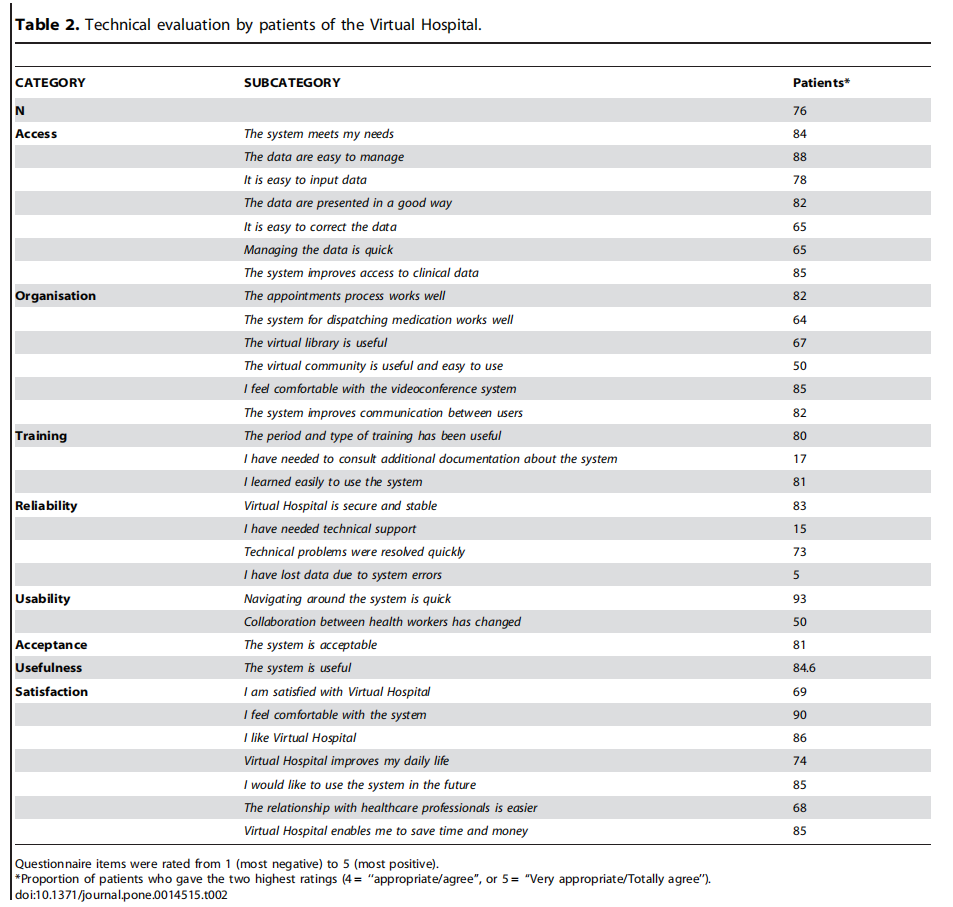
The technical performance of Virtual Hospital was evaluated by both professionals and patients. Validated questionnaires were used to assess different aspects of the system, with items being rated on a five-point scale, from 1 for the most negative appraisal (‘‘Not appropriate/Totally disagree’’) to 5 for the most positive one (‘‘Very appropriate/Totally agree’’). Parameters regarding access, organisation of the system, the need for training, reliability, usability, acceptance, usefulness and satisfaction were also evaluated.
The Virtual Hospital was also evaluated in terms of its clinical performance, assessing the impact on HIV clinical parameters [CD4 cell count, viral load (VL), opportunistic infections, death], the need to start combined AntiRetroviral Treatment (cART) and cART-compliance throughout the study follow-up. Adherence was evaluated at each clinical consultation by monitoring pharmacy refills and through self-reports and was considered high if the patients take more than 90% of the scheduled medication [33].
Quality of life was evaluated through a questionnaire that has been validated in HIV patients, the Mini International Neuropsychiatric Interview (MINI) [34,35]. This assessed various aspects including mental and physical health, cognitive and social functioning, energy levels and vitality, perceived social support, sleep and sexuality. Scores were standardised on a scale from 0 to 100, where 0 corresponds to better quality of life and 100 to a worse one.
Psychological and emotional Impact was evaluated using several validated screening questionnaires: the Hospital Anxiety and Depression (HAD) Scale [36,37] to measure anxiety and depression, Goldberg’s General Health Questionnaire (GHQ-28) [38,39] to screen for symptoms of psychopathology, and the Psychosocial Adjustment to Illness Scale (PAIS) [40] to measure the impact of a medical condition on general psychosocial functioning.
A qualitative statement about health services utilization in the study population, was registered in one of the questionnaires that patients field. There were two questions (question 7 and 9) addressing this issue. Question 7 was: How many times per year, do you consult the following health care providers? (7.1–7.3 Infectious Diseases Unit, 7.4 Pharmacy, 7.5 Social Work, 7.6 Psychiatry, 7.7 Primary Care, 7.8 Others). The answers were: never, one or two per year, each three or four months, each two months, each month, more than once per month. Question 9 was: How often has consulted to the following health care providers in the last three months? (Excluding Virtual Consultations) (9.1–9.3 Infectious Diseases Unit, 9.4 Pharmacy, 9.5 Social Work, 9.6 Psychiatry, 9.7 Primary Care, 9.8 Others). The answers were: never, ever, several times, once a month, more than once a month.
Quantitative characteristics were described as medians and the interquartile range (IQR), while qualitative data were given as frequencies and percentages. Laboratory parameters were compared using a Wilcoxon signed-rank test. Intra-individual changes in these parameters were compared for the period monitored by Virtual Hospital versus the period involving standard care (intraarm or intra-individual variations), and variability between arms at the end of the two-year follow-up was also compared (inter individual variations). All statistical analyses were performed using SPSS version 15.0.1. Patients were analyzed in the groups to which they were randomly assigned and a per-protocol analysis was conducted.
Sample size calculations (using McNemar’s test of paired proportions with a significance level of 5%) showed that 77 patients would have 80% power in detecting differences of 25% when the expected proportion of discordant pairs was 35%. The selection of this difference is consistent with other studies that found that non-adherence was associated with poorer virological outcomes [41–44]. With an estimated lost-to-follow-up rate of 10%, the total sample size required would be 90 patients.
Results
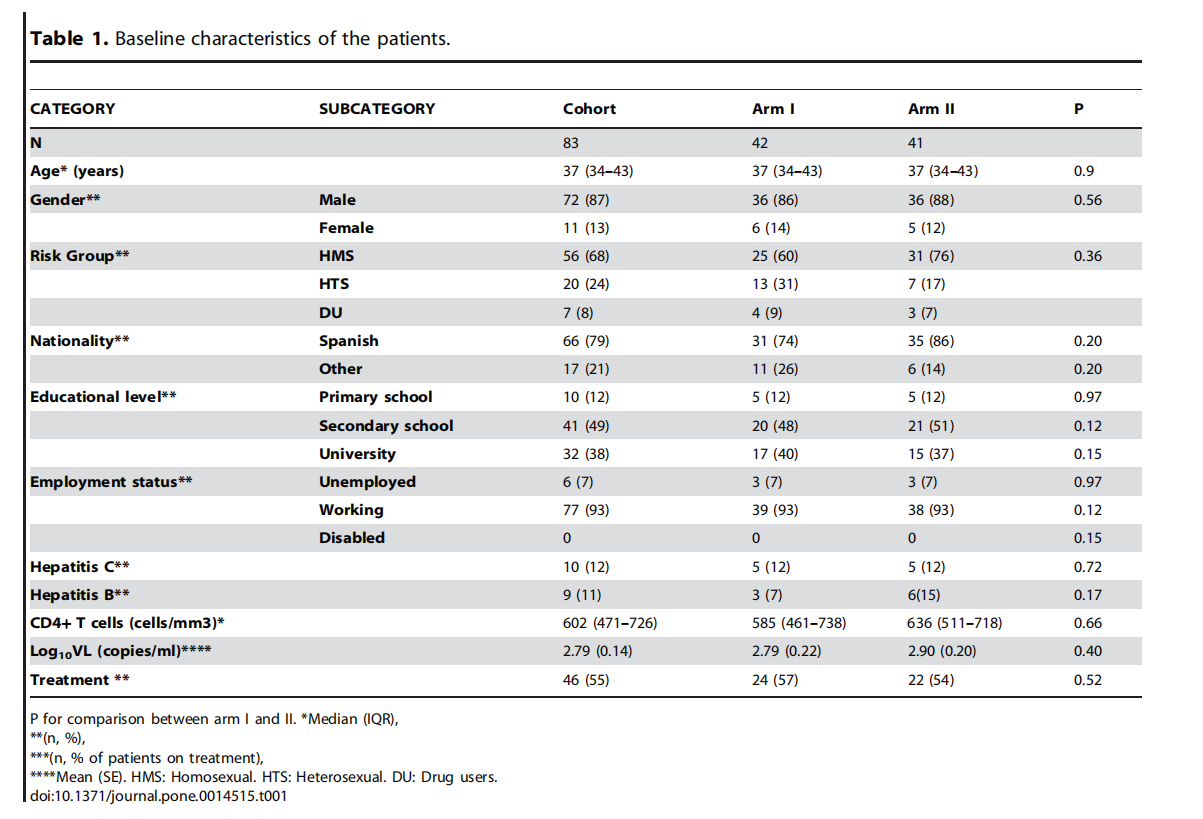
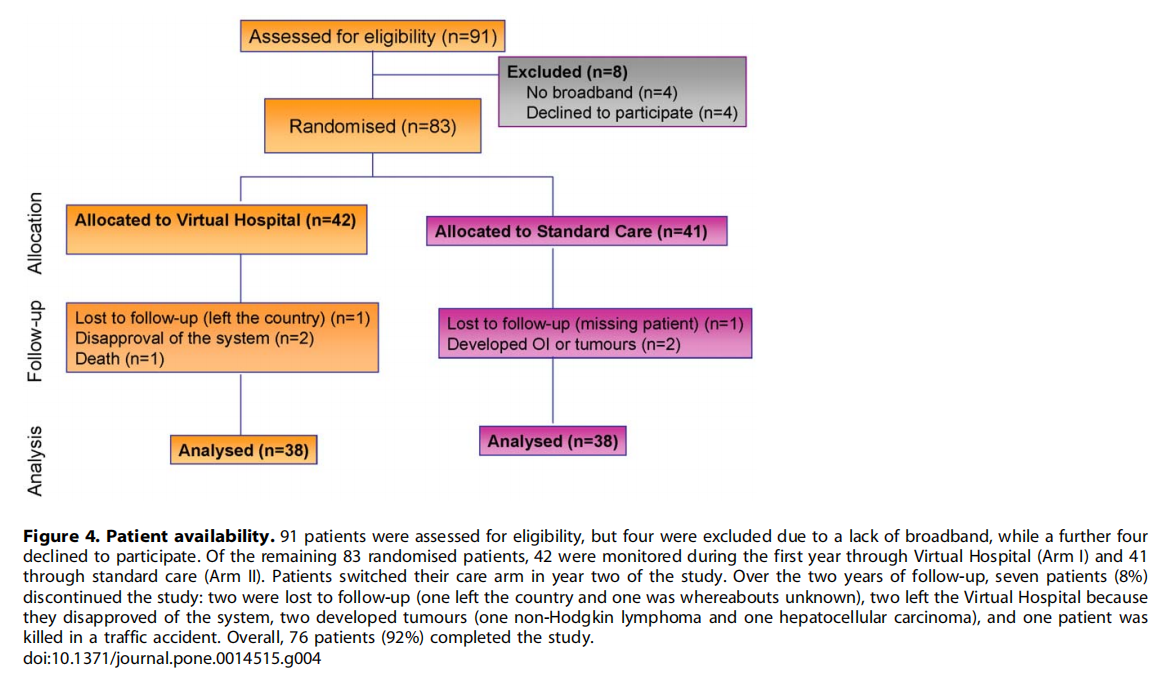
Initially, 91 patients were assessed for eligibility, but four were excluded due to a lack of broadband, while a further four declined to participate. Of the remaining 83 randomised patients, 42 were monitored during the first year through Virtual Hospital (Arm I) and 41 through standard care (Arm II). Patients switched their care arm in year two of the study. Baseline characteristics of the patients were well-balanced between the arms (see Table 1). Overall, 93% (n = 77) of the cohort had an active working life and 38% (n = 32) had a university degree. A similar number of patients (n = 46, 55% of the overall cohort) were receiving antiretroviral therapy at baseline (see Table 1). Over the two years of follow-up, seven patients (8%) discontinued the study: two were lost to follow up (one left the country and one was whereabouts unknown), two left the Virtual Hospital because they disapproved of the system, two developed tumours (one non-Hodgkin lymphoma and one hepatocellular carcinoma), and one patient was killed in a traffic accident (see patient availability in Figure 4). Overall, therefore, 76 patients (92%) completed the study.
Technical evaluation
Questionnaires submitted by patients (n = 76) revealed a high level of technical satisfaction with the system after one year of Virtual Hospital care (Table 2). Overall, 85% of patients (n = 65) considered that Virtual Hospital improved their access to clinical data, as compared with standard care, and they felt comfortable with the videoconference system. The system was rated by 82% (n = 62) of patients as an easy way to communicate among users. The same questionnaires were also completed by professionals (n = 18), with similar results (data not shown).
Clinical evaluation
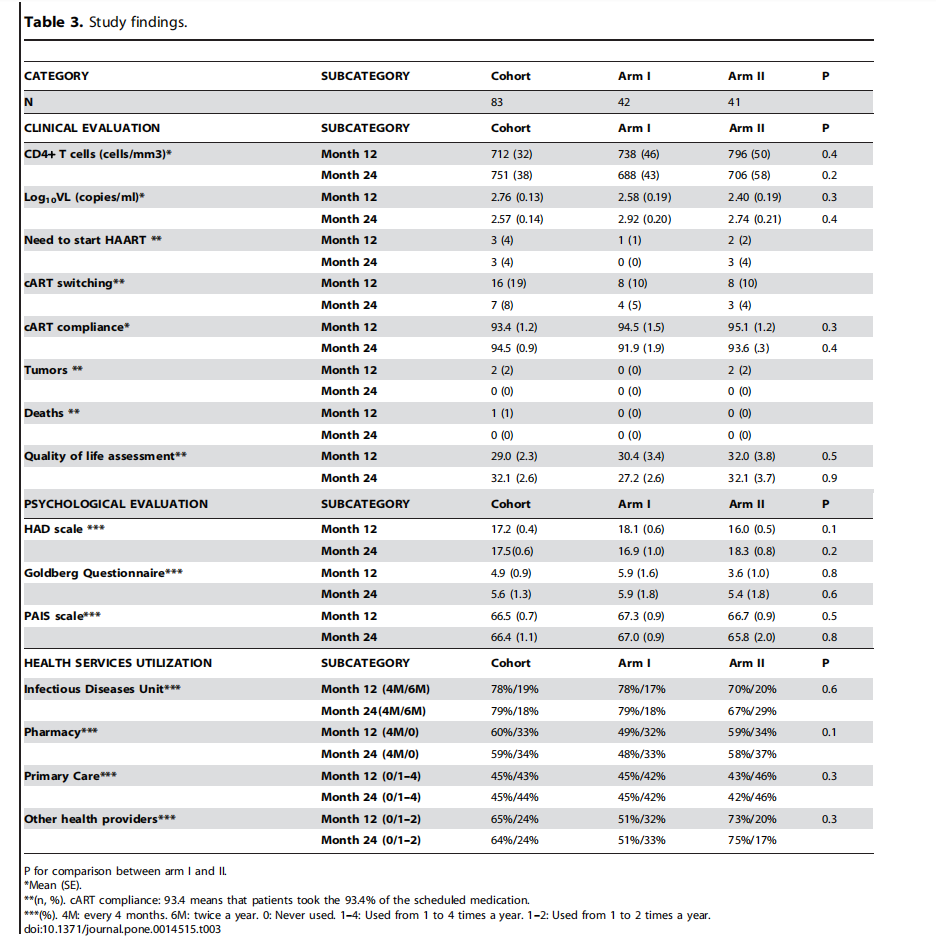
No opportunistic infections were reported. Regarding the immunologic evaluation there were no intra-individual (data not shown) or inter-individual differences over time in CD4 cell counts as monitored through Virtual Hospital versus standard care (See Table 3).
Changes in viral load were also similar within individuals (data not shown) and between arms when comparing the periods for Virtual Hospital and standard care (See Table 3). Patients on treatment continued to have an undetectable viral load throughout the study period in both arms except 1 patient in arm II.
Twenty-three patients (28%) switched antiretroviral therapy during the study follow-up. Therapeutic changes were due to: simplification (in 15 patients); because of side events related to medication (in 6 patients); virologic failure (in 1 patient) and in 1 patient because of interrupted manufacture of the antiretroviral being taken.
6 patients (7%) started cART throughout the study. cART switching and the need to start cART was similar between arms (Table 3).
cART-compliance was high (more than 90%) and was similar within individuals (data not shown) and between arms during the two years of follow-up (Table 3).
Quality of life and Psychological and emotional evaluation
Quality of life assessment did not shown any difference between arms during the two years of the study (Table 3). In addition, none of the psychological tests performed (HAD scale, Goldberg Health Questionnaire, Psychosocial Adjustment to Illness Scale) observed differences between arms during follow-up (Table 3)
Health services assessment
Regarding the consultation to the health care providers (n = 76), most of the patients (78%, n = 59) performed a consultation every four months to the Infectious Disease Unit and most of the remaining patients twice a year. About sixty percent of patients (n = 46) consulted Pharmacy every 4 months and 33% (n = 25) of the patients never did it (those who are untreated). 76% (n = 58) of the patients never used Psychiatry services. The utilization of these stable patients to the Social Work services was very low. Primary care physicians and other health care providers were never consulted by 45% (n = 34) and 64% (n = 49) of the patients, respectively (See Table 3). There were no differences in health services utilization between study arms during study follow-up.
Excluding Primary care, all the consultations performed not only infectious diseases specialists, but pharmacists, social worker and psychiatrists are integrated in the multidisciplinary care team of Virtual Hospital, allowing the patient to be remotely followed-up by these professionals too.
On the other hand, analyzing the health services utilization out of Virtual Consultations 69% (n = 52), 74% (n = 56) and 86% (n = 65) of the patients always consulted the Infectious diseases Unit, Pharmacy and Psychiatry services, respectively, using the virtual system. Again, similar results were observed between study groups.
Costs Evaluation
Regarding budget to develop this telemedicine system, there were costs related to equipment in the hospital infrastructure. Hardware and software Virtual Hospital development cost was 50.000 euros. An external company was hired to help patients with any technical problems involving hardware or software installation, training or maintenance of the system with a cost of 70 euros per patient/year. Posting service cost, used eventually for medication delivery to patient home, was about 50 euros per patient/year. Home infrastructure (computer and broadband connection) was supported by patients.
Discussion
We report the results of a prospective randomised study using a new model of multidisciplinary home care for chronic and stable HIV patients. The approach is based on a telemedicine platform, the Virtual Hospital, which covers the entire process of patient care (consultations, medical care, psychological and social support, medication, quality of life) via the internet and allows patients access to their own file. The study shows that Virtual Hospital constitutes a feasible, fairly satisfactory and safe tool for the clinical care of stable HIV-infected patients, and it has no deleterious effect on HIV clinical parameters, antiretroviral compliance, quality of life, or psychological and emotional status.
Patients were very satisfied with the system, as it has been showed by the satisfaction questionnaire and the low rate of withdrawal [76 from the 91 patients randomized ended the study (83%)]. In addition, when this study ended (december 2007), patients involved in it express their willingness to continue on Virtual Hospital and from then until now Virtual Hospital is being used as a routine work tool of the Infectious Disease Unit of the Hospital. Nowadays, there are round 200 patients cared of their HIV infection with such internet service. Otherwise being cared via Virtual hospital has not increased health resources utilization because of most of patients (69%, n = 52), out of Virtual consultations has never consulted to the Infectious diseases Unit even though almost a thirty percent of the study population (23 patients, 28%) has switched their antiretroviral medication, certainly one of the more difficult points in HIV management.
Telemedicine in HIV has been assessed in low-resource settings, both as an additional tool to help in the routine care of HIV-infected patients and for the training and education of healthcare providers [45]. Teleconferences, calls by mobile phones and ehealth systems have all been used to support comprehensive HIV treatment programmes. In developed countries, telemedicine has been used as a tool to solve communication problems, as a prevention strategy for gay men [46] or special populations such as Latinos [47] or African-Americans [48], and to improve health outcomes including antiretroviral adherence [49], access to care for HIV-infected prisoners [50], clinical monitoring of highly treatment-experienced HIV-infected patients [51], cardiovascular risk assessment electrocardiograms at distance [52], and smoking cessation interventions [53]. The main innovation of our webbased system is that, to our knowledge, this is the first time that a telemedicine approach has enabled the whole range of HIV care to be offered to stable and chronic patients.
New procedures and improvements in telemedical patient education could support self-management and self-care of this disease through tools such as access to electronic medical records, availability of constant information updates, and the development of a custom online community of patients. The system is also scalable for future functionality and enables the integration of both information and services, which could facilitate cooperation between different professionals (primary and specialist care), creating units to improve the care of HIV infection.
Our platform provides a technical infrastructure that can simultaneously support telemedicine programmes for different chronic diseases and patients with different risk levels. Indeed, platforms like the Virtual Hospital are destined to play a major role in facilitating new strategies for chronic care management, for example, by means of out-of-hospital follow-up, patient empowerment and care coordination, thereby improving patient care without an associated rise in costs. Several chronic diseases such as diabetes, congestive heart failure or chronic obstructive pulmonary disease have all used telemedicine with similar findings [6–25].
The world’s population is aging. As we age, the incidence and prevalence of chronic illness continue to rise, and elderly patients typically have multiple chronic diseases. The HIV-infected population follows this same trend, but the fact that the rate of new HIV infections has remained stable since 1995 [54] means the effect is worsened by the growing number of HIV-infected patients. The Hospital Clinic in Barcelona receives about 250 new HIV-infected patients each year. This increase, coupled with the drastic decrease in mortality due to current antiretroviral treatments, produces a significant annual increase in the care burden (around 10%, with an annual increase of 1000 new appointments in the Day Hospital). Given the current situation facing not only patients (who are likely to remain clinically stable for years) but also health providers, it is important to consider the enormous potential of the internet. Here the Virtual Hospital has been shown to be a feasible and safe tool for providing multidisciplinary home care to chronic HIV patients.
Although our study did not set out to measure the economics of study arms, to assist the reader’s understanding of the importance of the work to health care providers and to society as a whole in implementing the new system, we have made a qualitative statement about whether, for example, cost savings could be expected with the new system. The population of this study for clinical monitoring of their infection, regardless of belonging to a study arm or another, required to perform a blood test, a medical visit and eventually, antiretroviral treatment.
Regarding costs of blood tests, both direct costs (unitary price of a standard blood analysis, a CD4 test and an HIV-1 RNA test) and indirect costs (transport costs and time invested to reach the laboratory, productivity cost, absenteeism, quality of life and psychosocial status) should be the same for both study arms, because this study contemplated to perform the blood tests on the same site.
Costs of medical consultations for the health system, as the estimated unit cost for an outpatient visit with an HIV specialist care provider would not be modified in both types of cares. However, indirect costs regarding the time that professionals spend on each visit, the resources on space, infrastructure and personnel needed for a consultation presumably would be lower in the telemedicine arm and higher the communication effectiveness between patients and professionals. For example, the median time of a consultation via telemedicine is usually 5 minutes, compared with 20 minutes of standard visits; virtual consultation can be made at any office with a computer connected to the Internet (it is not necessary a day care hospital unit investing large areas, technical infrastructure and staffing complex), the median time to response to a consultation in the virtual branch is usually 24 hours, thus minimizing possible deleterious effects that any delay in communication could cause on clinical management. In parallel the costs of medical visits for patients, both direct costs (transportation to hospital) and indirect costs would be diminished in the telematic care among others by reducing travel time or waiting time for visits and medications (the median Hvirtual waiting time consultation is about 10 minutes compared with 60–90 minutes of waiting time at standard care).
The direct costs of antiretroviral medicaments should also be the same in both cares, although indirect costs to obtain antiretrovirals in the virtual arm should be lower than in the standard care. In the standard care arm, the patient must go to the hospital pharmacy to pick up the medication, which would include additional costs in transportation and working-time losses as previously mentioned. In the virtual arm, either because the medication arrives directly to patient’s home by courier or because it is the patient who chooses the best time to pick up medication when receives virtual antiretroviral prescription, indirect costs would be lower.
Then to summarize, out an initial software development investment, the Virtual Hospital cost per patient/year was 120 euros (or 70 euros without posting service cost medication delivery to patient home). Taking into account, the mentioned advantages that implementing this new model would provide in terms of direct and indirect costs of medical consultations and antiretroviral prescriptions for the health system and for patients, we believe that Virtual Hospital could be moreover cost-effective.
The study shows that Virtual Hospital constitutes a feasible, fairly satisfactory, safe and a low cost tool for the clinical care of stable HIV-infected patients and it has no deleterious effect on HIV clinical parameters and health services utilization.
Telemedicine should be considered an appropriate support service for the entire management of chronic HIV infection, is likely to prove extremely useful in settings with poor access to the health system.
Supporting Information
Protocol S1. Trial Protocol.
Found at: doi:10.1371/journal.pone.0014515.s001 (0.69 MB DOC)
References
1. Martin DK, Thiel EC, Singer PA (1999) A new model of advance care planning: observations from people with HIV. Arch Intern Med 159: 86–92.
2. Palella FJ, Jr., Delaney KM, Moorman AC, Loveless MO, Fuhrer J, et al. (1998) Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 338: 853–60.
3. Reiter GS (2000) Comprehensive clinical care: Managing HIV as a chronic illness. AIDS Clinical Car 12(2): 13–9.
4. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. November 3, 2008; 1-139. Available: http:// www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed 2009 Jul 23.
5. Martin DJ, Brooks RA, Ortiz DJ, Veniegas RC (2003) Perceived employment barriers and their relation to workforce-entry intent among people with HIV/ AIDS. J Occup Health Psychol 8: 181–194.
6. Balas EA, Jaffrey F, Kuperman GJ, Boren SA, Brown GD, et al. (1997) Electronic communication with patients. Evaluation of distance medicine technology. JAMA 278(2): 152–9.
7. Pitte JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, et al. (2000) Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes. Am J Med 108(1): 20–7.
8. Lahtela JT, Lamminen H (2002) Telemedical devices in diabetes management. Ann Med 34(4): 241–7.
9. Farmer A, Gibson OJ, Tarassenko L, Neal A (2005) A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med 22(10): 1372–8.
10. Young M, Sparrow D, Gottlieb D, Selim A, Friedman R (2001) A telephonelinked computer system for COPD care. Chest 119(5): 1565–75.
11. Bourbeau J, Julien M, Maltais F, Rouleau M, Beaupre´ A, et al. (2003) Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self management intervention. Arch Intern Med 163: 585–91.
12. Cooper CB (2009) Respiratory applications of telemedicine. Thorax 64(3): 189–91.
13. Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S (2007) Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 334(7600): 942.
14. Lobodzinski SS, Jadalla AA (2010) Integrated heart failure telemonitoring system for homecare. Cardiolo J 17(2): 200–204.
15. Polisena J, Tran K, Cimon K, Hutton B, McGill S, et al. (2010) Home telemonitoring for congestive heart failure: a systematic review and metaanalysis. J Telemed Telecare 16(2): 68–76.
16. Shah NB, Der E, Ruggerio C, Heidenreich PA, Massie BM (1998) Prevention of hospitalizations for heart failure with an interactive home monitoring program. Am Heart J 135: 373–378.
17. Jerant AF, Azari R, Nesbitt TS (2001) Reducing the cost of frequent hospital admissions for congestive heart failure: a randomized trial of a home telecare intervention. Med Care 39(11): 1234–45.
18. Giordano A, Scalvini S, Zanelli E, Corra` U, Longobardi GL, et al. (2009) Multicenter randomised trial on home-based telemanagement to prevent hospital readmission of patients with chronic heart failure. Int J Cardiol 131(2): 192–9.
19. Eaton T, Withy S, Garrett JE, Mercer J, Whitlock RM, et al. (1999) Spirometry in primary care practice: the importance of quality assurance and the impact of spirometry workshops. Chest 116: 416–23.
20. Benatar D, Bondmass M, Ghitelman J, Abitall B (2003) Outcomes of chronic heart failure. Arch Intern Med 163: 347–52.
21. Whitten P, Love B (2005) Patient and provider satisfaction with the use of telemedicine: overview and rationale for cautious enthusiasm. J Postgrad Med 51: 294–300.
22. Montori VM, Hellgemoe PK, Guyatt GH, Dean DS, Leung TW, et al. (2004) Telecare for patients with type 1 diabetes and inadequate glycemic control: a randomized controlled trial and meta-analysis. Diabetes Care 27: 1088–94.
23. Polisena J, Tran K, Cimon K, Hutton B, McGill S, et al. (2009) Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obes Metab 11(10): 913–30.
24. Stone RA, Rao RH, Sevick MA, Cheng C, Hough LJ, et al. (2010) Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care 33(3): 478–94.
25. Larsen ME, Turner J, Farmer A, Neil A, Tarassenko L (2010) Telemedicinesupported insulin optimisation in primary care. J Telemed Telecare 16(8): 433–40.
26. Barlow J, Bayer S, Curry R (2003) The design of pilot telecare projects and their integration into mainstream service delivery. J Telemed Telecare 9(suppl. 1): 1–3.
27. Celler BG, Lovell NH, Basilakis J (2003) Using information technology to improve the management of chronic disease. Med J Aust 179(5): 242–246.
28. Holman HR, Lorig KR (2000) Patients as partners in managing chronic disease. Partnership is a prerequisite for effective and efficient health care. BMJ 320: 526–527.
29. Cretin S, Shortell SM, Keeler EB (2004) An evaluation of collaborative interventions to improve chronic illness care. Framework and study design. Eval Rev 28: 28–51.
30. Wiecha J, Pollard T (2004) The interdisciplinary eHealth team: chronic care for the future. J Med Internet Res 6(3): e22.
31. Caceres C, Gomez EJ, Garcia F, Chausa P, Guzman J, et al. (2005) A Home Integral Telecare System for HIV/AIDS Patients. Stud Health Technol Inform. 2005 114: 23–29.
32. Caceres C, Gomez EJ, Garcia F, Gatell JM, del Pozo F (2006) An integral care telemedicine system for HIV/AIDS patients. Int J Med Inform 75: 638–642.
33. Lima VD, Harrigan R, Murraya M, Moore DM, Wood E, et al. (2008) Differential impact of adherence on long-term treatment response among naı¨ve HIV-infected individuals. AIDS 22(17): 2371–2380.
34. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, et al. (1998) The MINI international Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview. J Clin Psychiatry 59(Supl 20): 22–33.
35. Trepanier LL, Rourke SB, Bayoumi AM, Halman MH, Krzyzanowski S, et al. (2005) The impact of neuropsychological impairment and depression on healthrelated quality of life in HIV-infection. J Clin Exp Neuropsychol 27: 1–15.
36. Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6): 361–370.
37. Herrero MJ, Blanch J, Peri JM, De Pablo J, Pintor L, et al. (2003) A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiatry 25(4): 277–283.
38. Goldberg DP (1973) The detection of psychiatric illness by questionnaire. London: Oxford University Press, 1972 Psychological Medicine 3: 257–257.
39. Lobo A, Pe´rez- Echevarrı´a MJ, Jime´nez- Azna´rez A, Sancho MA, et al. (1988) Emotional disturbances in endocrine patients. Validity of the scaled version of the General Health Questionnaire (GHQ-28). J Psych 152: 807–812.
40. Derogatis LR (1986) The psychosocial adjustment to illness. Journal of Psychosomatic Research 30(1): 77–91.
41. Duong M, Piroth L, Peytavin G, Forte F, Kohli E, et al. (2001) Value of patient self-report and plasma human immunodeficiency virus protease inhibitor level as markers of adherence to antiretroviral therapy: relationship to virologic response. Clin Infect Dis 33: 386–392.
42. Martin M, Del Cacho E, Codina C, Tuset M, De Lazzari E, et al. (2008) Relationship between Adherence Level, Type of the Antiretroviral Regimen, and Plasma HIV Type 1 RNA Viral Load: A Prospective Cohort Study. AIDS Research and Human Retroviruses 24(10): 1263–1268.
43. Lima VD, Harrigan R, Murraya M, Moore DM, Wood E, et al. (2008) Differential impact of adherence on long-term treatment response among naı¨ve HIV-infected individuals. AIDS 22: 2371–2380.
44. Maggiolo F, Ravasio L, Ripamonti D, Gregis G, Quinzan G, et al. (2005) Similar Adherence Rates Favor Different Virologic Outcomes for Patients Treated with Nonnucleoside Analogues or Protease Inhibitors. Clinical Infectious Diseases 40: 158–63.
45. Kiviat AD, Geary MC, Sunpath H, Moosa MY, Wilson D, et al. (2007) HIV Online Provider Education (HOPE): the internet as a tool for training in HIV medicine. J Infect Dis 196 Suppl 3: S512–5.
46. McKee MB, Picciano JF, Roffman RA, Swanson F, Kalichman SC (2006) Marketing the ‘‘Sex Check’’: evaluating recruitment strategies for a telephonebased HIV prevention project for gay and bisexual men. AIDS Educ Prev 18(2): 116–31.
47. Mahoney MR, Khamarko K, Goldschmidt RH (2008) Care of HIV-infected Latinos in the United States: a description of calls to the national HIV/AIDS Clinicians’ Consultation Center. J Assoc Nurses AIDS Care 19(4): 302–10.
48. Goldschmidt RH, Graves DW (2003) The National HIV Telephone Consultation Service (Warmline): a clinical resource for physicians caring for African-Americans. J Natl Med Assoc 95(2 Suppl 2): 8S–11S.
49. Dunbar PJ, Madigan D, Grohskopf LA, Revere D, Woodward J, et al. (2003) A two-way messaging system to enhance antiretroviral adherence. J Am Med Inform Assoc 10(1): 11–5.
50. Besch Cl (2007) Telemedicine improves access to care for HIV-infected prisoners. HIV Clin 19(1): 4–5.
51. LLibre JM, Domingo P, Del Pozo MA, Miralles C, Galindo MJ, et al. (2008) Long-distance interactive expert advice in highly treatment-experienced HIV-infected patients. J Antimicrob Chemother 61(1): 206–9.
52. Malacarne M, Cargnel A, Lucici D, Pizzinelli P, Porta A, et al. (2007) Feasibility of assessing autonomic dysregulation at a distance: the case of the HIV-positive patient. Telemed J E Health 13(5): 557–563.
53. Vidrine DJ, Arduino RC, Lazev AB, Gritz ER (2006) A randomized trial of a proactive cellular telephone intervention for smokers living with HIV/AIDS. AIDS 20(2): 253–60.
54. Status of the global HIV epidemic 2008 UNAIDS Global AIDS Epidemic Report. Available: http://www.unaids.org/globalreport/default.htm.
This article is excerpted from Online HIV Care by Wound world.