Abstract
Importance
While telehealth use in surgery has shown to be feasible, telehealth became a major modality of health care delivery during the COVID-19 pandemic.
Objective
To assess patterns of telehealth use across surgical specialties before and during the COVID-19 pandemic.
Design, Setting, and Participants
Insurance claims from a Michigan statewide commercial payer for new patient visits with a surgeon from 1 of 9 surgical specialties during one of the following periods: prior to the COVID-19 pandemic (period 1: January 5 to March 7, 2020), early pandemic (period 2: March 8 to June 6, 2020), and late pandemic (period 3: June 7 to September 5, 2020).
Exposures
Telehealth implementation owing to the COVID-19 pandemic in March 2020.
Main Outcomes and Measures
(1) Conversion rate defined as the rate of weekly new patient telehealth visits divided by mean weekly number of total new patient visits in 2019. This outcome adjusts for a substantial decrease in outpatient care during the pandemic. (2) Weekly number of new patient telehealth visits divided by weekly number of total new patient visits.
Results
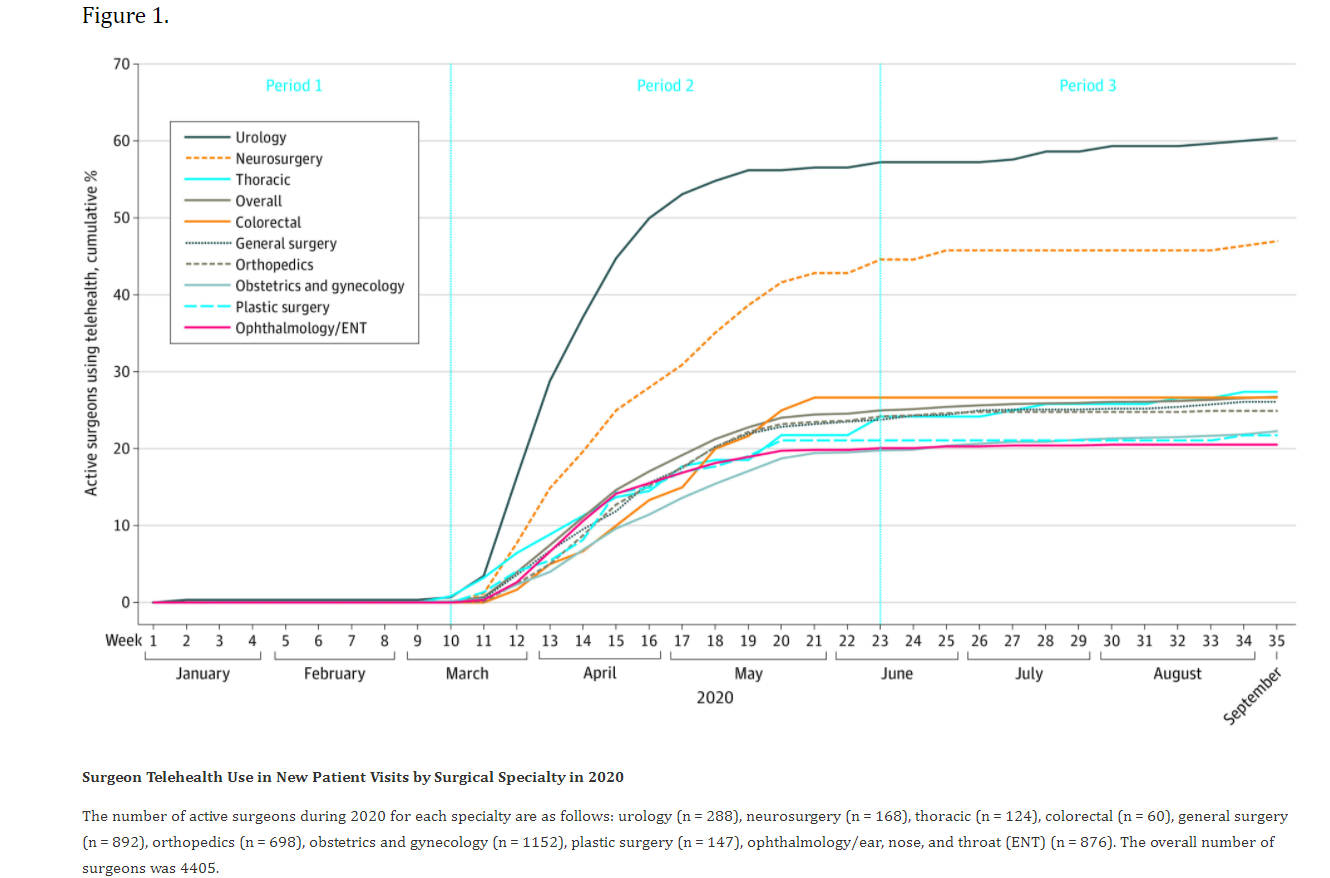
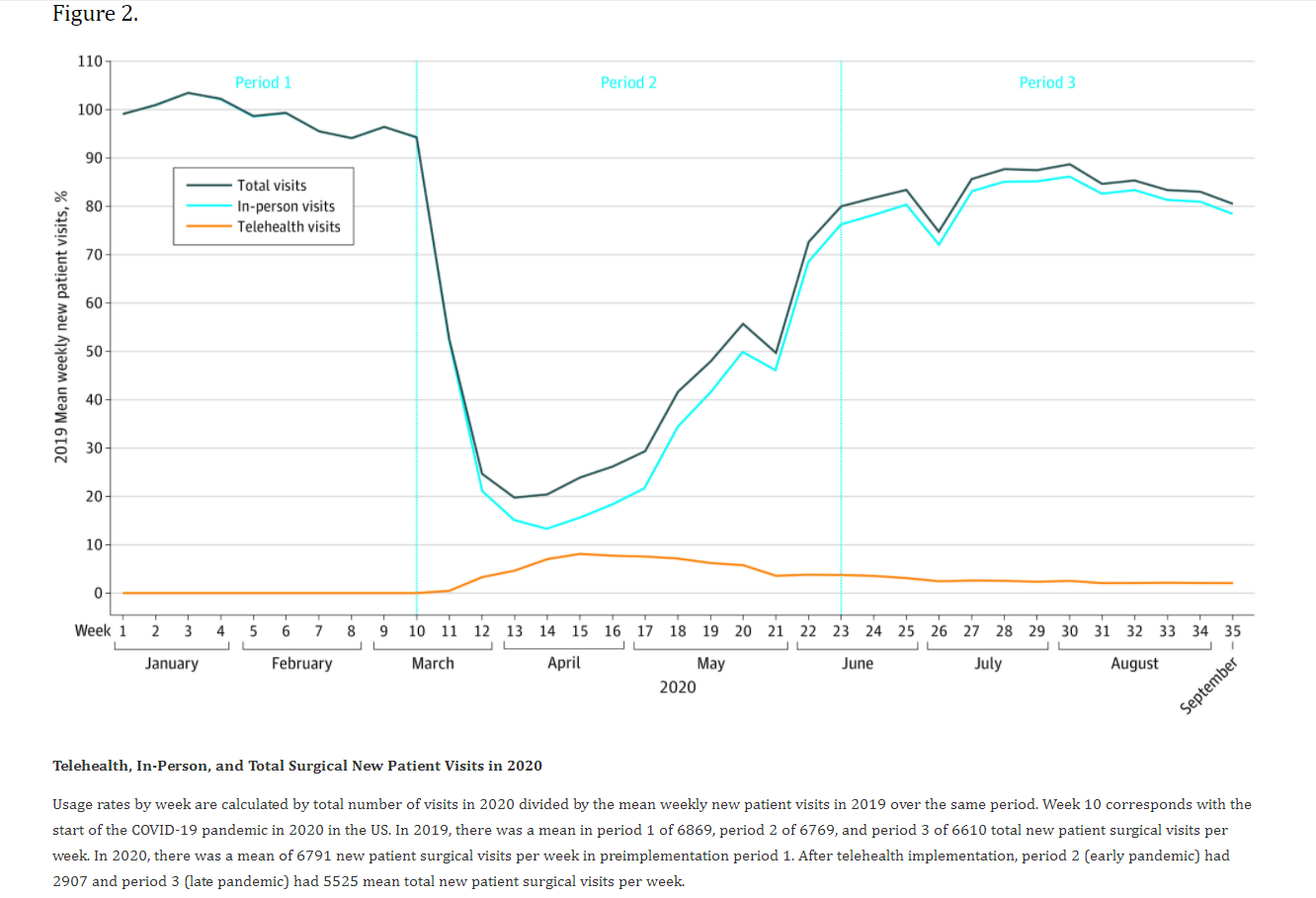
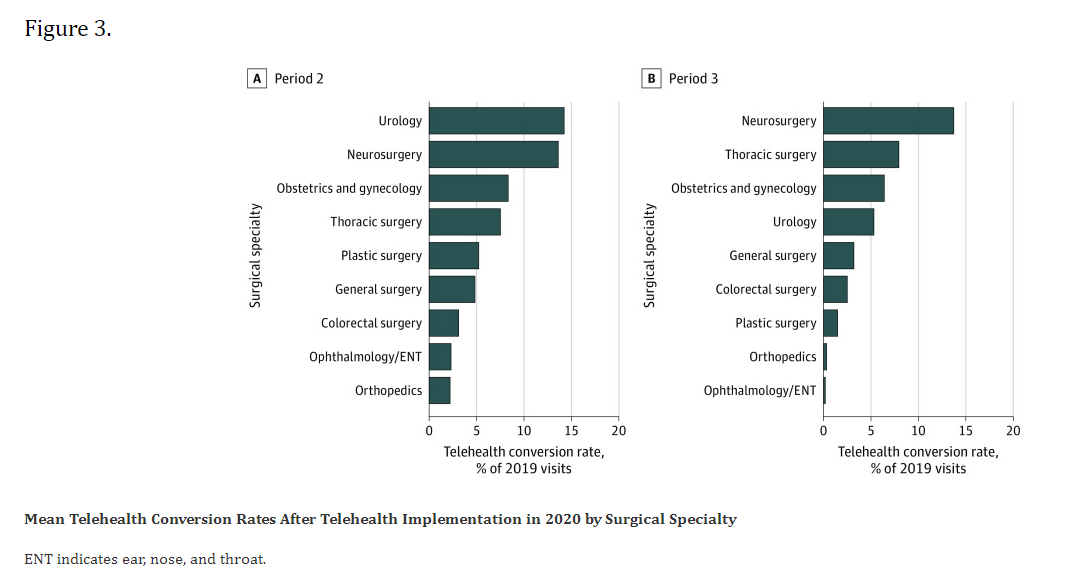
Among 4405 surgeons in the cohort, 2588 (58.8%) performed telehealth in any patient care context. Specifically for new patient visits, 1182 surgeons (26.8%) used telehealth. A total of 109 610 surgical new outpatient visits were identified during the pandemic. The median (interquartile range) age of telehealth patients was 46.8 (34.1-58.4) years compared with 52.6 (38.3-62.3) years for patients who received care in-person. Prior to March 2020, less than 1% (8 of 173 939) of new patient visits were conducted through telehealth. Telehealth use peaked in April 2020 (week 14) and facilitated 34.6% (479 of 1383) of all new patient visits during that week. The telehealth conversion rate peaked in April 2020 (week 15) and was equal to 8.2% of the 2019 mean weekly new patient visit volume. During period 2, a mean (SD) of 16.6% (12.0%) of all new patient surgical visits were conducted via telehealth (conversion rate of 5.1% of 2019 mean weekly new patient visit volumes). During period 3, 3.0% (2168 of 71 819) of all new patient surgical visits were conducted via telehealth (conversion rate of 2.5% of 2019 new patient visit volumes). Mean (SD) telehealth conversion rates varied by specialty with urology being the highest (14.3% [7.7%]).
Conclusions and Relevance
Results from this study showed that telehealth use grew across all surgical specialties in Michigan in response to the COVID-19 pandemic. While rates of telehealth use have declined as in-person care has resumed, telehealth use remains substantially higher across all surgical specialties than it was prior to the pandemic.
Introduction
The COVID-19 pandemic created an urgent need to overhaul health care delivery. The US health care system suddenly faced 2 new mandates: minimize patient and clinician exposure to COVID-19 and maintain patient access to health care. Telehealth, in the form of video and audio-only visits, had the potential to address these challenges. In the pandemic’s early months, national telehealth use in Medicare beneficiaries grew from 13 000 visits per week to nearly 1.7 million.1 Within surgical fields, telehealth had been previously used for preoperative and postoperative follow-up visits2,3,4,5 although at low levels prior to the COVID-19 pandemic.6,7While telehealth use in surgery has shown to be feasible, the profession found itself in a novel situation during the COVID-19 pandemic, wherein telehealth became a major modality of health care delivery.
While it is clear that telehealth uptake has increased during the COVID-19 pandemic, several unknowns remain. First is the extent to which surgical specialties used telehealth vs in-person care during the COVID-19 pandemic. While some specialties (eg, psychiatry) do not require the physical examination and in-office testing, this is not the case for surgical specialties. Additionally, the amount of care provided through telehealth is expected to vary from the early months of the pandemic (March to June 2020) through to the later part of the pandemic (June to September 2020) because during the later period, many health care systems and practices allowed in-person visits because of the availability of masks and social distancing practices. Second, it is not known whether surgical specialties were able to convert in-person appointments to telehealth. National data indicate that 60% to 70% of patients deferred care during the pandemic.7,8 In this study, conversion rate refers to the extent to which surgical specialties were able to salvage visits compared with patient volumes in 2019. Finally, the variation in these patterns of telehealth use across surgical subspecialties is not known. The capacity for telehealth conversion in each surgical specialty may differ because of differences in the balance of outpatient vs inpatient care, the range of diagnoses able to be determined without tactile portions of the physical examination, the sensitivity of the visit’s content, and whether cases were elective vs urgent or emergent.
Few studies of telehealth exist because of the relatively new nature of patients accessing telehealth from home.9 Prior studies of surgical telehealth have limited their scope primarily to patient acceptability and the feasibility of the clinic to use telehealth.4Other contemporary studies have also been limited to single institutions or specific diagnoses and operations.10,11,12 The objective of this study is to assess the patterns of telehealth use across surgical specialties before and during the COVID-19 pandemic with the hypothesis that there will be significant variation by surgical specialty.
Methods
Data and Study Population
We used claims from a large commercial insurance payer in Michigan for this analysis. The plan covers 3.5 million individuals per year, approximately 700 000 of whom saw a surgeon in 2019. For our primary analysis, we identified new adult outpatient visits with a surgeon (Current Procedural Terminology [CPT] codes 92002, 92004, 99201-99205) during a 9-month period (January 5 to September 5, 2020). We focused our primary analysis on new patient visits, which are more reliably billed for and thus more reliably included in claims data. Postoperative visits for established patients may be part of a global or bundled payment for surgery and thus are more likely to be missing from claims data. While our primary analysis was limited to new patient visits, we performed a sensitivity analysis using all surgical evaluation and management claims. We included all 9 available surgical specialties: colorectal surgery, general surgery, neurosurgery, obstetrics and gynecology, ophthalmology/ear, nose, and throat (ENT), orthopedics, plastic surgery, thoracic surgery, and urology. The study was deemed exempt from review by the University of Michigan institutional review board given that all data were deidentified.
Identifying Telehealth Visits
We categorized new patient visits by in-person office visits or telehealth visits (audio-only or video visits), using appropriate telehealth modifier codes. Because of relaxed billing rules during the pandemic, we could not reliably differentiate audio-only visits from video visits and therefore did not report audio-only visits separately. However, we did perform a sensitivity analysis that included audio-only billing codes (CPT codes 99441-99443). We counted only 1 visit per day per patient; for patients with multiple visits in 1 day, we categorized them as having a telehealth visit that day if one of the visits was by telehealth. These excluded claims accounted for 0.5% of total claims.
During our 9-month study period, we defined 3 pandemic time periods based on trends observed in the raw data: period 1 (pre–COVID-19 pandemic), period 2 (early pandemic), and period 3 (late pandemic). Period 1 represents January 5 to March 7, 2020. Because clinics began to accelerate in-person care several weeks into the pandemic, we examined 2 periods during the COVID-19 pandemic. Period 2 represents the early pandemic and spans March 8 to June 6, 2020, when national and state telehealth regulations were relaxed to accommodate social distancing measures and Michigan stay-at-home orders were executed.13 Period 3 represents the late pandemic when emergency orders, such as the ban on elective procedures, lifted and spans June 7 to September 5, 2020. Our control group comprised new patient visits in the prior year (2019) for the same calendar weeks of each period. All of the examined visits are associated with a surgeon.
Defining Telehealth Conversion
Our primary outcomes describe telehealth conversion due to telehealth implementation in 2020. Telehealth conversion is the rate of new patient telehealth visits per week divided by the mean weekly total new patient visit volume in the prior year (2019). Mean weekly total new patient visit volume in the prior year is calculated over the corresponding dates in each period the prior year: January 6 to September 7, 2019. We then examined telehealth conversion after telehealth implementation by surgical specialty to determine which specialties were more or less likely to convert in-person appointments to telehealth. We examined the mean telehealth conversion rates in each study period.
Statistical Analysis
We performed a descriptive analysis of the surgical telehealth uptake in 2020 compared with in-person visits. In addition to demographics, we examined whether patients were from rural areas as determined by zip code with a Rural-Urban Commuting Area code of 2 or 314 and whether patients were from higher-income areas as determined by zip code median income higher than the median income for all patients.15 Univariate χ2 and Wilcoxon rank sum test analyses were used as appropriate to assess differences in patient characteristics between those who used telehealth vs those who received care in person. We plotted the trends in overall telehealth surgical use over time.
Sensitivity Analysis
We performed a sensitivity analysis to assess the robustness of our primary findings. Some surgical specialties may have reserved telehealth use for established patients, while some may have coded audio-only visits outside of the new and established visit codes. Thus, we performed a sensitivity analysis for period 2 to examine whether adding established patient visits or audio-only visits to the cohort changed which specialties were more or less likely to adopt telehealth. In our first sensitivity analysis, we added established patient visits (CPTcodes 92012, 92014, 99211-99215). In a second sensitivity analysis, we added audio-only visits (CPTcodes 99441-99443) to the new and established patient visits.
We used SAS statistical software version 9.6 (SAS Institute) to prepare our cohorts and perform all statistical analyses. All statistical tests were 2-sided and performed at the 5% significance level.
Results
Overall Surgical Telehealth Conversion
Telehealth was used by 2588 of 4405 active surgeons (58.8%) in any patient care context. Active surgeons were those with at least 1 new patient visit in 2020. Specifically for new patient visits, 1182 active surgeons (26.8%) used telehealth (Figure 1). We identified 109 610 surgical new outpatient visits from March 8, 2020, through September 5, 2020. Of these visits, there were 6634 telehealth visits (6.1%) and 102 976 in-person visits (94.0%). This is compared with the 8 telehealth visits (<0.1% of 173 939 total visits) during the same time in 2019.
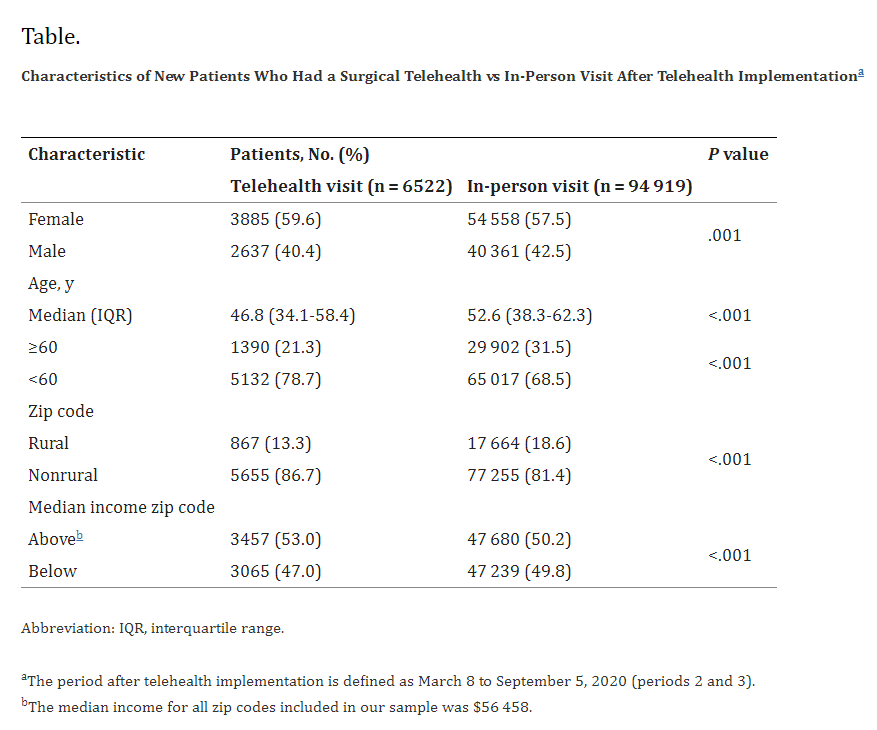
 Weekly telehealth use peaked in April 2020 (week 14), accounting for 34.6% (479 of 1383) new patient visits for that week. The Table shows patient characteristics for patients who used telehealth vs in-person visits following telehealth implementation (periods 2 and 3). The median (interquartile range) age of telehealth patients was 46.8 (34.1-58.4) years compared with 52.6 (38.3-62.3) years for patients who received care in-person (P < .001). There were more women than men among all surgical patients. Rural patients were less likely to use telehealth visits than nonrural patients (867 of 18 531 [4.7%] vs 5655 of 82 910 [6.8%]; χ2 = 115.5; P < .001). Patients who lived in below–median income zip codes were less likely to use telehealth compared with those who lived in above–median income zip codes (3065 of 50 304 [6.1%] vs 3457 of 51 137 [6.8%]; χ2 = 18.8; P < .001).
Weekly telehealth use peaked in April 2020 (week 14), accounting for 34.6% (479 of 1383) new patient visits for that week. The Table shows patient characteristics for patients who used telehealth vs in-person visits following telehealth implementation (periods 2 and 3). The median (interquartile range) age of telehealth patients was 46.8 (34.1-58.4) years compared with 52.6 (38.3-62.3) years for patients who received care in-person (P < .001). There were more women than men among all surgical patients. Rural patients were less likely to use telehealth visits than nonrural patients (867 of 18 531 [4.7%] vs 5655 of 82 910 [6.8%]; χ2 = 115.5; P < .001). Patients who lived in below–median income zip codes were less likely to use telehealth compared with those who lived in above–median income zip codes (3065 of 50 304 [6.1%] vs 3457 of 51 137 [6.8%]; χ2 = 18.8; P < .001).
 1,2,3,4
1,2,3,4 
