Introduction
Wound healing is a complicated tissue response to harm resulting in skin recovery.Keloid scarring or hypertrophic can be productive of modifications in wound healing process.1 Between 30% and 90% of patients have hypertrophic scars and keloids, which are produced by burns, trauma, surgery, acne, and various other skin diseases.1–3 Scar formation is determined by Fitzpatrick’s skin type; for instance, Caucasians are much less prone to keloids and hypertrophic scars than Asians and Africans, and if they do develop such scars, they tend not to be as severe as those in more susceptible populations. The prevalence of keloids among African American, Latin American, and Asian American populations is reported to be from 0.3% to 16%. Hypertrophic scars have been demonstrated to develop in 30% to 75% of burn patients and 75% of surgical patients.4 Recent research has revealed depressed self-worth and harmed the quality of life in affected persons as a result of physical, psychological, and social sequelae underlining the necessity for more beneficial therapy alternatives for these patients.5,6 However, treatments for hypertrophic or keloid scarring are currently tremendously challenging for clinicians due to invalid outcomes of numerous therapeutic approaches.
In this case report, we describe a case of scar repair following trauma on the facial region resulting from a car accident leading to degloving injury. The case was treated by sequential therapy at Chengdu Second People’s Hospital, resulting in suturing scar repaired as analogously normal skin. The following case notes are provided to further study sequential therapy for scars and advocate an effective treatment alternative to improve patients’ life quality avoiding disfigurement.
Case Presentation
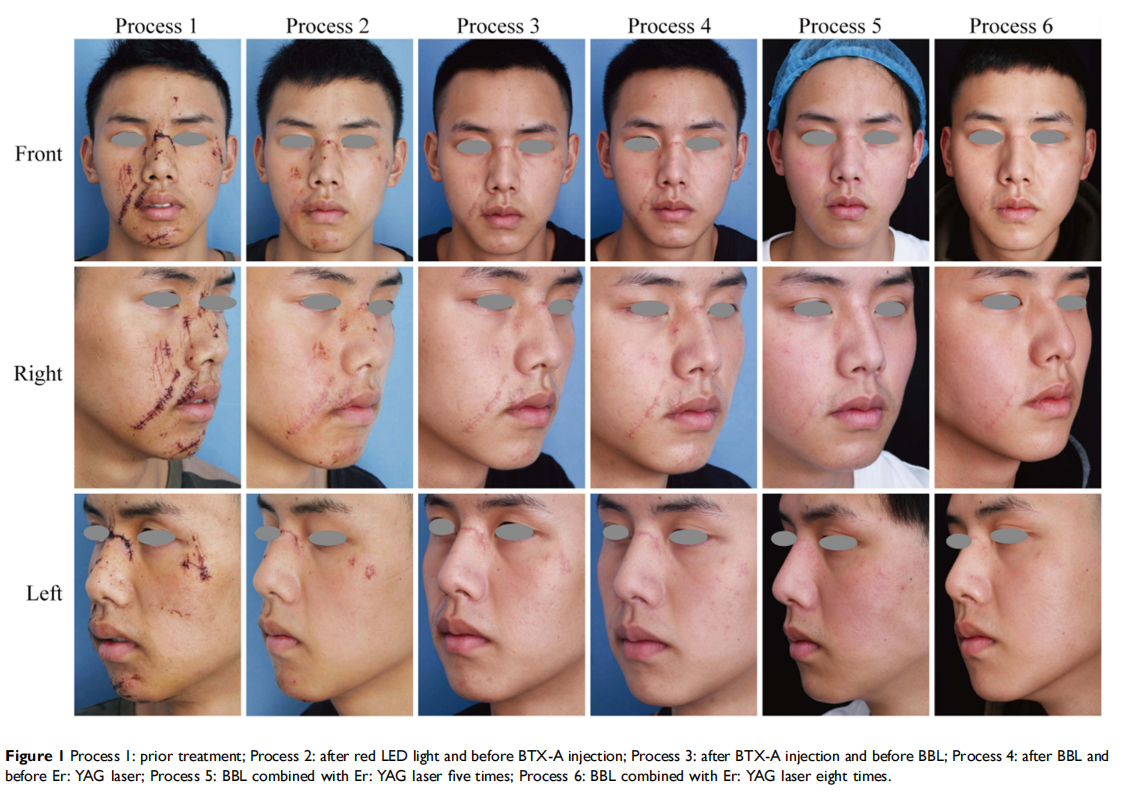
A 19-year-old male with facial postoperative trauma suture resulting from being involved in a car accident on March 29, 2019 presented a strong desire to prevent scar hyperplasia on his face. We developed a sequential treatment based on wound healing as follows. Red LED therapy (20 min, 96 J/cm2 , 633 nm) was applied twice on the full face from March 30, 2019 to June 02, 2019. On June 04, 2019, we injected Botulinum Toxin Type A (BTX-A), a cumulative dose of 36 IU once. Between June 8, 2019 and July 15, 2019, red LED therapy combined with Broad Band Light (BBL) were performed at 4-week intervals for two sessions. Energy density was 9 J/cm2 , the cutoff filters were 560 nm, the spot size was 1.5×4.5 cm2 , the temperature was 15 °C, the pulse durations were 10 ms, and the pulse delays were 30 ms. From August 19, 2019, we combined BBL and Er: YAG laser (Profile, USA), emitting at a wavelength of 2940 nm eight times. Treated areas were handled to depths between 100 and 110 µm, with a coverage density of 11%. As the correction attained promptly after the process was visible and acceptable, the treatment proved to be secure and efficacious for correcting wound healing (Figure 1). Now, we have collected the most recent patient images following a ten-step process of BBL and Er: YAG laser is displayed as follows (Figure 2). Our case is almost achieved to scarless healing, which is difficult to imagine given the enormous car accident that occurred to him.

The patient provided written informed permission to have any accompanying photos and case details published.
Discussion
Most researches have determined the validity of topical corticosteroids, CO2 laser treatment, cryosurgery, surgery, sheet application, silicone gel application, pressure application, radiotherapy, and intralesional injection of corticosteroids, 5-fluorouracil, triamcinolone and interferon, and so on.7–9 Despite taking these steps, scar hyperplasia has resulted in disfigurement and is difficult to revert to normal skin, impairing the quality of life in numerous patients who suffer from distress as much as those with other chronic skin diseases.5 With a plethora of therapy options available, it is critical to understand how to integrate different approaches with patients over time to assist in their recovery.
Skin injury healing procedure is frequently accompanied by scar formation in adults.10 In the initial stage of healing, extremely alive fibroblasts promote healing and injury closure. However, in the late stage of wound healing,11 excessive deposition of collagen and extracellular matrix (ECM) originated from extremely alive fibroblasts results in improper scar formation, impairing the original tissue’s functional recovery.12,13 In our case, we employ various treatments to target different wound healing stages to attain the best therapeutic outcome.
In the initial phase, red LED therapy was applied twice to accelerate wound healing. As regional blood circulation has improved, the wound healing energy of 630 nm and its application in soreness attenuation have been considerably illustrated. This athermal effect modulates the actions of the mark cells, reducing pain, depleting edema, and expediting the wound-healing process, as demonstrated in the current research, with pain, erythema, and edema half to one-third the size of the unirradiated aspect.14
After removing stitches, we injected BTX-A into each of the burned areas. Its employment in diverse medical conditions has expanded over the years in both aesthetic and medical applications. Most physicians prefer it due to its efficacy and scarcity of side effects. The mechanism of efficiency of BTX-A has been manifested to involve wound tension process, collagen, and fibroblasts.15 Apoptosis-inducing myofibroblasts and reprogramming them to become scar-resolving cells are emerging as potential therapeutic techniques for reversing existing fibrosis.16 Early postoperative BTX-A injection in the medial canthal zone decreases hypertrophic efficiency scarring.15,17 Intralesional BTX-A injection was more effective than intralesional corticosteroid injection in treating keloid and hypertrophic scar.3 In our case, we could observe that after injecting BTX-A, the patient did not experience significant erythema and proliferation.
IPL therapy might influence the neovascularization that has been demonstrated to be effective on surgically induced scars. It is effective not only in ameliorating the appearance of keloids and hypertrophic scars besides their origin but also in depleting height, redness, and hardness of scars.18 In our case, after the wounds healed, we applied Broad Band Light (BBL), which is the world’s most powerful IPL device to promote vascular contraction and inhibit scar hyperplasia. Our immediate postoperative effect is by the standard of eupyrexia, reddish, slight tingling, and can naturally subsidize after ice compress for half an hour. We selected low energy to take advantage of photobiomodulation over photothermy. Three months later, we applied the erbium: yttrium aluminum garnet (Er: YAG) laser combined with BBL eight times. Skin roughness, wrinkle depth, viscoelastic and elastic deformities can completely be amended over time within the scar treated with Er: YAG fractional ablation.19,20 In the pig model, Er: YAG treatment ameliorated scars over CO2 laser treatment, as increased levels of antifibrotic proteoglycan Decorin, MMP-2, and MMP-9 were discovered in Er: YAG treated scar samples, indicating that Er: YAG treatment involved remodeling the dermis in the region through cutting off likely scar substance and preventing scar output.21 Compared to CO2, diode, and Nd: YAG lasers, Er: YAG laser has been recognized as a laser with less tissue damage extension and superior incision regularity.22 In addition, Er: YAG ablative fractional lasers can induce thermal injury at a deeper dermal layer than non-ablative fractional lasers, making them more effective for thicker scars.
In conclusion, we combined various treatments at different wound healing stages to achieve the best therapeutic effect. Sequential therapy has shown improvement in scar treatment to be employed as a substitute therapy for scar management.
Acknowledgments
Xiaoqing Li and Mei He are co-first authors in this study. Our institutional approval was obtained to publish the case
Disclosure
The authors declare no conflicts of interest.
References
1. Barolet D, Boucher A. Prophylactic low-level light therapy for the treatment of hypertrophic scars and keloids: a case series. Lasers Surg Med. 2010;42(6):597–601. doi:10.1002/lsm.20952
2. Arno AI, Gauglitz GG, Barret JP, Jeschke MG. Up-to-date approach to manage keloids and hypertrophic scars: a useful guide. Burns. 2014;40 (7):1255–1266. doi:10.1016/j.burns.2014.02.011
3. Bi M, Sun P, Li D, Dong Z, Chen Z. Intralesional Injection of Botulinum Toxin Type A Compared with Intralesional Injection of Corticosteroid for the Treatment of Hypertrophic Scar and Keloid: a Systematic Review and Meta-Analysis. Med Sci Monit. 2019;25:2950–2958. doi:10.12659/MSM.916305
4. Austin E, Koo E, Jagdeo J. The Cellular Response of Keloids and Hypertrophic Scars to Botulinum Toxin A: a Comprehensive Literature Review. Dermatol Surg. 2018;44(2):149–157. doi:10.1097/ DSS.0000000000001360
5. Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006;297(10):433–438. doi:10.1007/s00403-006-0651-7
6. Leventhal D, Furr M, Reiter D. Treatment of keloids and hypertrophic scars: a meta-analysis and review of the literature. Arch Facial Plast Surg. 2006;8(6):362–368. doi:10.1001/archfaci.8.6.362
7. Ogawa R, Akita S, Akaishi S, et al. Diagnosis and Treatment of Keloids and Hypertrophic Scars-Japan Scar Workshop Consensus Document 2018. Burns Trauma. 2019;7:39. doi:10.1186/s41038- 019-0175-y
8. Alster T, West T. Treatment of scars: a review. Ann Plast Surg. 1997;39(4):418–432. doi:10.1097/00000637-199710000-00014
9. Chen M, Davidson T. Scar management: prevention and treatment strategies. Curr Opin Otolaryngol Head Neck Surg. 2005;13 (4):242–247. doi:10.1097/01.moo.0000170525.74264.f8
10. Monavarian M, Kader S, Moeinzadeh S, Jabbari E. Regenerative Scar-Free Skin Wound Healing. Tissue Eng Part B Rev. 2019;25 (4):294–311. doi:10.1089/ten.teb.2018.0350
11. Long Y, Wei H, Li J, et al. Effective Wound Healing Enabled by Discrete Alternative Electric Fields from Wearable Nanogenerators. ACS Nano. 2018;12(12):12533–12540. doi:10.1021/acsnano.8b07038
12. Duffield J, Lupher M, Thannickal V, Wynn T. Host responses in tissue repair and fibrosis. Annu Rev Pathol. 2013;8:241–276. doi:10.1146/annurev-pathol-020712-163930
13. Shen Y, Xu G, Huang H, et al. Sequential Release of Small Extracellular Vesicles from Bilayered Thiolated Alginate/ Polyethylene Glycol Diacrylate Hydrogels for Scarless Wound ACS Nano. 2021;15(4):6352–6368. doi:10.1021/ acsnano.0c07714
14. Trelles MA, Allones I. Red light-emitting diode (LED) therapy accelerates wound healing post-blepharoplasty and periocular laser ablative resurfacing. J Cosmet Laser Ther. 2006;8(1):39–42. doi:10.1080/14764170600607731
15. Kasyanju Carrero LM, Ma WW, Liu HF, Yin XF, Zhou BR. Botulinum toxin type A for the treatment and prevention of hypertrophic scars and keloids: updated review. J Cosmet Dermatol. 2019;18(1):10–15. doi:10.1111/jocd.12828
16. Hinz B, Lagares D. Evasion of apoptosis by myofibroblasts: a hallmark of fibrotic diseases. Nat Rev Rheumatol. 2020;16 (1):11–31.
17. Huang RL, Ho CK, Tremp M, Xie Y, Li Q, Zan T. Early Postoperative Application of Botulinum Toxin Type A Prevents Hypertrophic Scarring after Epicanthoplasty: a Split-Face, Double-Blind, Randomized Trial. Plast Reconstr Surg. 2019;144 (4):835–844. doi:10.1097/PRS.0000000000006069
18. Erol OO, Gurlek A, Agaoglu G, Topcuoglu E, Oz H. Treatment of hypertrophic scars and keloids using intense pulsed light (IPL). Aesthetic Plast Surg. 2008;32(6):902–909. doi:10.1007/s00266-008-9161-7
19. Madni T, Lu K, Nakonezny P, et al. Treating Hypertrophic Burn Scar With 2940-nm Er: yAGLaser Fractional Ablation Improves Scar Characteristics as Measured by Noninvasive Technology. J Burn Care Res. 2019;40(4):416–421. doi:10.1093/jbcr/irz056
20. Ozog D. Commentary on Treatment of Hypertrophic Burn and Traumatic Scars With 2940 mm Fractional Ablative Er: YAG. Dermatol Surg. 2020;46(6):794–795. doi:10.1097/ DSS.0000000000002194
21. Rodriguez-Menocal L, Davis S, Becerra S, et al. Assessment of Ablative Fractional CO2 Laser and Er: yAGLaser to Treat Hypertrophic Scars in a Red Duroc Pig Model. J Burn Care Res. 2018;39(6):954–962. doi:10.1093/jbcr/iry012
22. Monteiro L, Delgado M, Garcês F, et al. A histological evaluation of the surgical margins from human oral fibrous-epithelial lesions excised with CO2 laser, Diode laser, Er: yAGlaser, Nd: yAGlaser, electrosurgical scalpel and cold scalpel. Med Oral Patol Oral Cir Bucal. 2019;24(2):e271–e280.
This article is by wound world,excerpted from the Clinical, Cosmetic and Investigational Dermatology.