伤口世界
- 星期二, 08 10月 2024
Hallmarks of aging: An expanding universe(2023)--1
Carlos Lo´ pez-Otı´n,1,2,3,* Maria A. Blasco,4 Linda Partridge,5,6 Manuel Serrano,7,8,9 and Guido Kroemer10,11,12,*
1 Departamento de Bioquı´mica y Biologı´a Molecular, Instituto Universitario de Oncologı´a (IUOPA), Universidad de Oviedo, Oviedo, Spain
2 Instituto de Investigacio´ n Sanitaria del Principado de Asturias (ISPA), Oviedo, Spain
3 Centro de Investigacio´ n Biome´ dica en Red de Ca´ ncer (CIBERONC), Madrid, Spain
4 Telomeres and Telomerase Group, Molecular Oncology Program, Spanish National Cancer Centre (CNIO), Madrid, Spain
5 Department of Genetics, Evolution and Environment, Institute of Healthy Ageing, University College London, London, UK
6 Max Planck Institute for Biology of Ageing, Cologne, Germany
7 Institute for Research in Biomedicine (IRB Barcelona), Barcelona Institute of Science and Technology (BIST), Barcelona, Spain
8 Catalan Institution for Research and Advanced Studies (ICREA), Barcelona, Spain
9 Altos Labs, Cambridge, UK
10 Centre de Recherche des Cordeliers, Equipe labellise´ e par la Ligue contre le cancer, Universite´ de Paris, Sorbonne Universite´ , INSERM U1138, Institut Universitaire de France, Paris, France
11 Metabolomics and Cell Biology Platforms, Gustave Roussy, Villejuif, France
12 Institut du Cancer Paris CARPEM, Department of Biology, Hoˆ pital Europe´ en Georges Pompidou, AP-HP, Paris, France
*Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (C.L.-O.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (G.K.)
https://doi.org/10.1016/j.cell.2022.11.001
SUMMARY
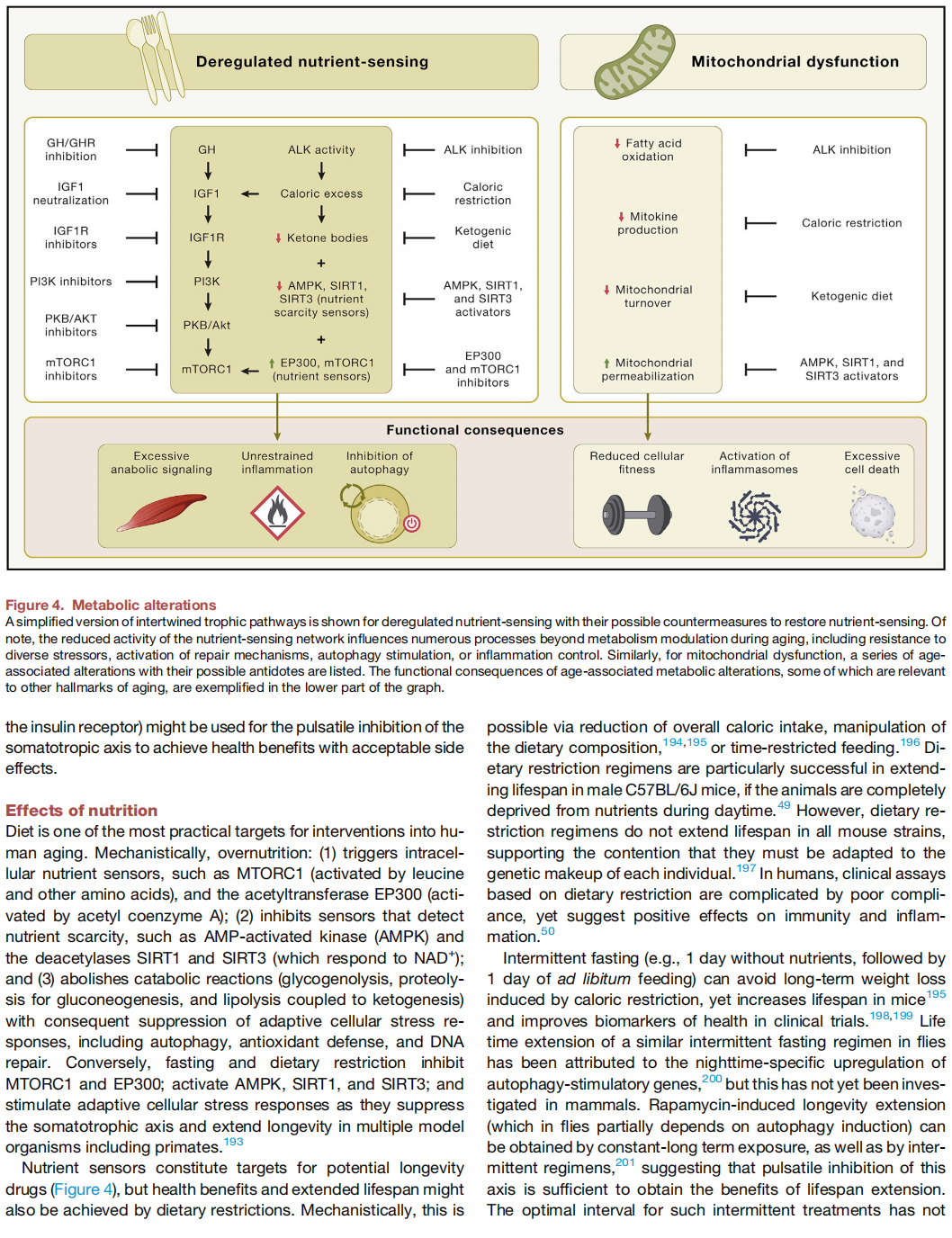
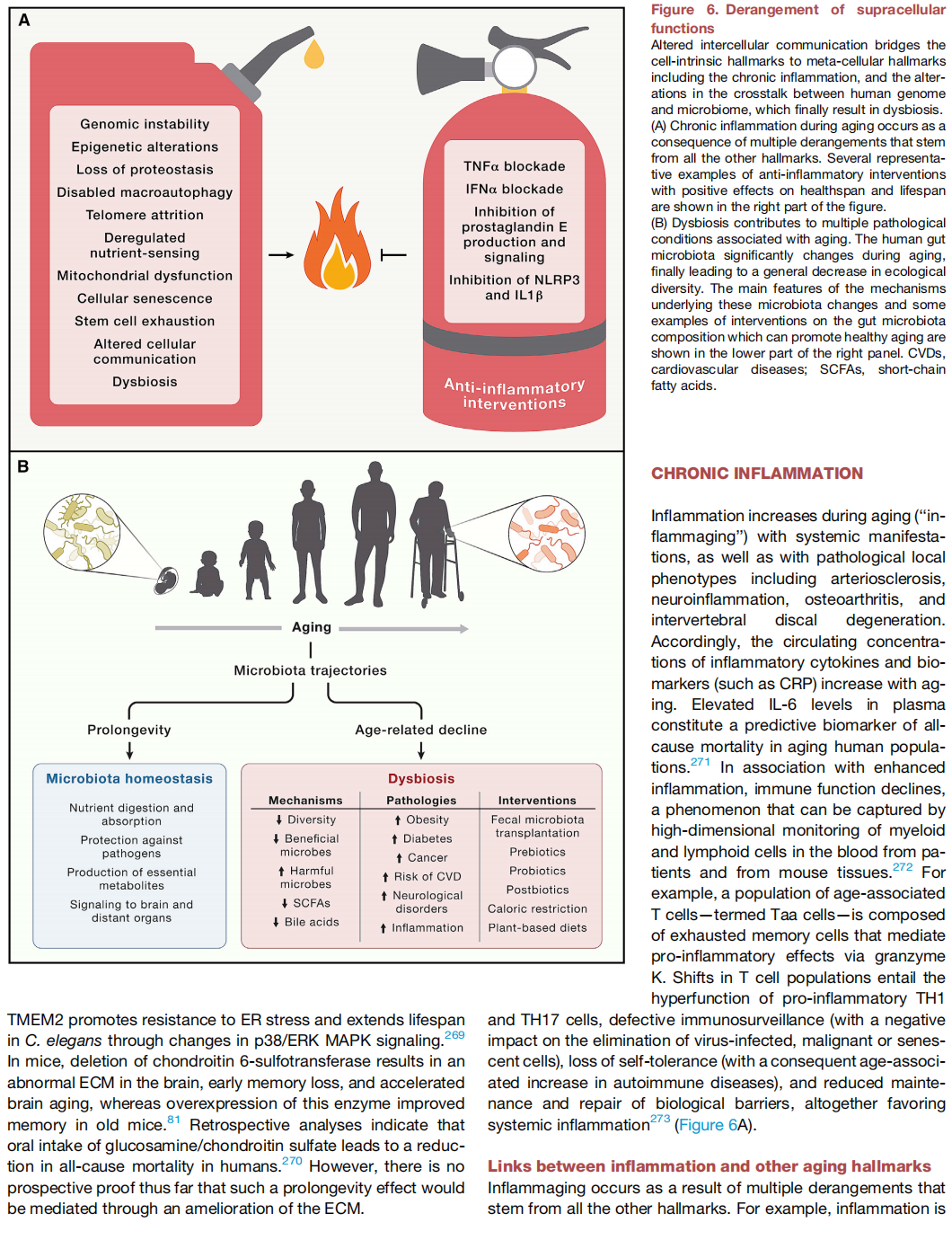
Aging is driven by hallmarks fulfilling the following three premises: (1) their age-associated manifestation, (2) the acceleration of aging by experimentally accentuating them, and (3) the opportunity to decelerate, stop, or reverse aging by therapeutic interventions on them. We propose the following twelve hallmarks of aging: genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, disabled macroautophagy, deregulated nutrient-sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, altered intercellular communication, chronic inflammation, and dysbiosis. These hallmarks are interconnected among each other, as well as to the recently proposed hallmarks of health, which include organizational features of spatial compartmentalization, maintenance of homeostasis, and adequate responses to strees.
- 星期一, 30 9月 2024
Reprogramming to recover youthful epigenetic information and restore vision
Yuancheng Lu1, Benedikt Brommer2,3,11, Xiao Tian1,11, Anitha Krishnan3,4,11, Margarita Meer5,6,11, Chen Wang2,3, Daniel L. Vera1, Qiurui Zeng1, Doudou Yu1, Michael S. Bonkowski1, Jae-Hyun Yang1, Songlin Zhou2,3, Emma M. Hoffmann3,4, Margarete M. Karg3,4, Michael B. Schultz1, Alice E. Kane1, Noah Davidsohn7, Ekaterina Korobkina3,4, Karolina Chwalek1, Luis A. Rajman1, George M. Church7, Konrad Hochedlinger8, Vadim N. Gladyshev5, Steve Horvath9, Morgan E. Levine6, Meredith S. Gregory-Ksander3,4,* , Bruce R. Ksander3,4,* , Zhigang He2,3,* , David A. Sinclair1,10,*,#
1. Department of Genetics, Blavatnik Institute, Paul F. Glenn Center for Biology of Aging Research, Harvard Medical School, MA, USA;
2. Department of Neurology, Boston Children’s Hospital, Harvard Medical School, MA, USA;
3. Department of Ophthalmology, Harvard Medical School, Boston, MA, USA;
4. Schepens Eye Research Institute of Mass Eye & Ear, Harvard Medical School, MA, USA;
5. Division of Genetics, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, MA, USA;
6. Department of Pathology, Yale School of Medicine, New Haven, CT, USA;
7. Department of Genetics, Wyss Institute for Biologically Inspired Engineering, Harvard University, MA, USA;
8. Department of Molecular Biology, Cancer Center and Center for Regenerative Medicine, Massachusetts General Hospital, MA, USA;
9. Department of Human Genetics, David Geffen School of Medicine, University of California Los Angeles, CA, USA;
10. Laboratory for Aging Research, Department of Pharmacology, School of Medical Sciences, The University of New South Wales, Sydney, Australia;
11. These authors contributed equally: B. B., X. T., A. K., M. M.;
Users may view, print, copy, and download text and data-mine the content in such documents, for the purposes of academic research, subject always to the full Conditions of use:http://www.nature.com/authors/editorial_policies/license.html#terms
#* Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。.
Senior authors;
Contributions
Y.L. and D.A.S. conceived the project. Y.L., X.T., and D.A.S. wrote the manuscript with input from all co-authors. Y.L. was involved in all experiments and analyses. M.S.B. and J.-H.Y. provided early training to Y.L.. B.B., C.W., Q.Z., D.Y., S.Z., and Z.H. contributed to the optic nerve crush studies and imaging. A.K., D.Y., Q.Z., E.M.H., E.K., M.S.G.-K., and B.R.K. contributed to the glaucoma and ageing studies. M.M.K. and B.R.K. performed OCT imaging and analysis. M.M. and V.N.G. conducted ribosomal DNAm age analysis for mouse RGCs. M.E.L. developed DNAm ageing signature. D.L.V. performed the RNA-seq and gene association analysis. X.T. conducted human neuron experiments. S.H. conducted human methylation clock analysis. X.T., J.-H.Y., and K.H. helped with transgenic mouse fibroblasts work. M.S.B., X.T., M.B.S., A.E.K., L.A.R., helped with systemic AAV9 experiments. N.D., and G.M.C. helped with plasmid constructs and AAV9 production. K.C. helped with grant applications and project management. M.S.G.-K., B.R.K., Z.H., and D.A.S. jointly supervised this work.
Conflict of interest
D.A.S. is a consultant to, inventor of patents licensed to, board member of and equity owner of Iduna Therapeutics, a Life Biosciences company developing epigenetic reprograming therapies. D.A.S. is an advisor to Zymo Research, an epigenetics tools company. Additional disclosures are at https://genetics.med.harvard.edu/sinclair/people/sinclair-other.php. Y.L., L.A.R. and S.H. are equity owners of Iduna Therapeutics, a Life Biosciences company. D.L.V. is an advisor to Liberty Biosecurity. M.S.B. is a shareholder in MetroBiotech. K.C. is an equity owner in Life Biosciences and affiliates. N.D. and G.M.C. are co-founders of Rejuvenate Bio. Disclosures for G.M.C. can be found at http://arep.med.harvard.edu/gmc/tech.html. M.E.L. is a bioinformatics advisor to Elysium Health. Y.L., N.D. and D.A.S. are inventors on patents arising from this work (WO/2020/069373 and WO/2020/069339), filed by the President and Fellows of Harvard College. The other authors declare no competing interests.
- 星期日, 29 9月 2024
男性雄激素性秃发中西医诊疗专家共识
国家皮肤和性传播疾病专业质控中心毛发专家委员会,国家中西医结合医学中心毛发专病医联体,中国整形美容协会中医美容分会,中华中医药学会皮肤科分会毛发学组,北京中西医结合学会皮肤性病专业委员会毛发学组
National Professional Quality Control Center for Skin and Sexually Transmitted Diseases, Hair Expert Comittee; National Center of Integrated Traditional Chinese and Westerm Medicine Hair Diseases Medical Treatment Combination; Chinese Plastic and Aesthetic Association of Traditional Chinese Medicine Cosmetology Branch; Working Group for Hair Diseases, China Association of Chinese Medicine, Dermatology Branch; Working Group for Hair Diseases, Beijing Association of the Integrating of Traditional and Western Medicine Dematological and Venereal Diseases Professional Committee
[摘要]雄激素性秃发(AGA)是临床最常见的脱发性疾病,男性AGA发病率更高,严重影响患者的身心健康和生活质量。目前认为该病与遗传易感性和脱发部位毛囊细胞对雄激素的高反应性密切相关。诊断主要依据病史、脱发模式和皮肤镜检查。中医药治疗是我国AGA防治的优势和特色,为了推广男性AGA的规范化中西医诊治理念,提高我国在该领域的诊治水平,特组织编写了该专家共识。
[关键词]雄激素性秃发,男性; 中西医;诊疗;专家共识
[中图分类号] R758.71
[文献标识码] A
[文章编号] 1000- 4963(2024 )05- -0305-07
doi: 10.16761/j.cnki.1000- 4963.2024.05.014
- 星期五, 27 9月 2024
2023中国临床实践指南:雄激素性脱发诊断与治疗
中华医学会整形外科学分会中国雄激素性脱发诊断与治疗指南制订工作组整形美容 .
专业国家级医疗质量控制中心中国整形美容协会毛发 医学分会中 国女医师协会.
整形美容专业委员会
通信作者:张菊芳,西湖大学医学院附属杭州市第一人民医院医疗美容科,杭州310006, Email: zhjuf@ vip. sina. com;
吴文育,复旦大学附属华山医院皮肤科,上海200040, Email: wuwenyu@ huashan. org. cn;
牛冬,浙江农林大学动物科技学院、动物医学院,杭州311300, Email: dniu@ zafu. edu.cn;
龙笑,中国医学科学院北京协和医学院北京协和医院整形外科,北京100032, Email: pumclongxiao@ 126. com.
[摘要] 雄激素性脱发发病率逐年增高并呈现低龄化的趋势,困扰着众多患者。对于雄激素性脱发的治疗,近年来出现了很多新方式和思路,因此雄激素性脱发的治疗策略需要随之更新;另外,随着近年来毛发行业的发展,大量的从业者涌人雄激素性脱发诊治的相关岗位,因此需要经过证实的指南来进行指引。指南制订工作组遴选了有关临床问题,经过证据检索、专家论证,形成了相关推荐意见,以期能够进一步规范雄激素性脱发的治疗决策。
[关键词] 脱发;雄激素性脱发; 整形外科;指南
基金项目:杭州市医学重点学科( 002020004);上海市级医院皮肤科临床能力促进与提升专科联盟(SHDC22022302);上海市重中之重研究中心建设项目(2023702018);上海毛发医学工程技术研究中心(19D22250500);浙江省自然科学基金重点项目(LZ22C010003);北京协和医院中央高水平医院临床科研专项( 2022-PUMCH-B-042)
DOI: 10. 3760/ema. j. en1 14453-20231029-00156
Chinese guideline for the diagnosis and treatment of androgenetic alopecia ( 2023)
The Working Group of Chinese Guideline for the Diagnosis and Treatment of Androgenetic Alopeeia, Chinese Medical Association of Plastic Surgery; National Medical Quality Control Center for Plastic Surgery; Society of Hair Medicine, Chinese Association of Plastics and Aesthetics; Plastic & Aesthetic Surgery Comitee, China Medical Women 's Association
Corresponding author: Zhang Jufang, Department of Medical Cosmetology, Hangzhou First People' s Hospital, Westlake University, Hangzhou 310006, China, Email: zhjuf@ rip. sina. com; Wu Wenyu,
Department of Dermatology, Huashan Hospital, F'udan University, Shanghai 200040, China, Email: wuwenyu@ huashan. org. cn; Niu Dong, Animal Science College and Animal Medicine College , Zhejiang
A&F University , Hangzhou 311300,China, Email: dniu@ zafu. edu. cn; Long Xiao, Department of Plastic Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100032, China ,Email: pumclongxiao@ 126. com
[ Summary] The incidence rate of androgenetice alopecia is increasing year by year and presents a trend of younger age, which puzzles many patients. In recent years, there have been many new treatment
methods and ideas for androgenetic alopecia, so the treatment strategies for androgenetic alopecia need to be : updated accordingly. In addition, with the development of the hair industry in recent years, a large number of practitioners have flocked to positions related to the diagnosis and treatment of androgenetie alopecia, so proven guidelines are needed for guidance. The guide writing team selected relevant clinical issues, gave recommendations based on a thorough literature review of the latest reports and expert' s evaluation, in the hope of providing a treatment algorithm for androgenetic alopecia.
[Key words] Alopecia; Androgenetic alopecia; Plastie surgery; Guideline
Fund program: Hangzhou Key Discipline of Medieine ( 0020200044 ) ; Shanghai M unicipal Hospital Dermatology Clinical Ability Promotion and Enhancement Specialist Alliance .
( SHDC22022302) ; Shanghai Most Important Research Center Construction Project ( 2023Z702018) ; Shanghai Hair Medical Engineering Technology Research Center ( 19DZ2250500); Zhejiang Province
Natural Science Foundation Key Project ( LZ22C010003 ); National High Level Hospital Clinical Research Funding ( 2022-PUMCH-B-042)
Disclosure of Conflicts of Interest: The authors have no financial interest to declare in relation to the content of this article.
DOI: 10. 3760/ ema. j. en1 14453-2023 1029-00156
- 星期四, 26 9月 2024
中国敏感性皮肤诊治专家共识
何黎1 ,郑捷2 ,马慧群3 ,郝飞4 ,刘玮5 ,王刚6 ,李利7 ,高兴华8 ,项蕾红9 ,吴艳1 0 ,谢红付11 ,袁超12 ,林彤13 ,赖维14 ,刘盛秀1 5 ,张丽8 ,李吉1 1 ,严淑贤9 ,崔勇16 ,李虹17 ,陈抗18 ,周展超19 ,钟莉20 ,梁虹2 1 ,骆丹2 2 ,卢凤艳23 ,熊霞24 ,庞勤2 5 ,王玮蓁26 ,王秀丽12 ,朱丽萍1
[中图分类号] R 593. 1
[文献标识码] A
[文章编号] 1001 - 7089( 2017) 01 - 0001 - 04
[DOI] 10. 13735 /j. cjdv. 1001-7089. 201611168
[基金项目] 云南省“高原皮肤病防治转化医学协同创新中心”( 601160707) ; 教育部 2013 年度“创新团队发展计划”( RIT13067) 资助项目
[作者单位] 1. 昆明医科大学第一附属医院,云南 昆明 650032;
2. 上海交通大学附属瑞金医院,上海 200240;
3. 西安交通大学第二附属医院,陕西西安710000;
4. 第三军医大学第一附属医院( 西南医院) ,重庆400038;
5. 北京空军总医院,北京100142;
6. 第四军医大学西京医院,陕西 西安710000;
7. 四川大学华西医院,四川 成都610041;
8. 中国医科大学附属第一医院,辽宁 沈阳110001;
9. 复旦大学附属华山医院,上海200040;
10. 北京大学第一医院,北京 100034;
11. 中南大学湘雅医院,湖南 长沙 410008;
12. 上海市皮肤病医院,上海 200443;
13. 中国医学科学院皮肤病医院,江苏 南京210042;
14. 中山大学附属第三医院,广东 广州 510630;
15. 安徽医科大学附属医院,安徽 合肥 230032;
16. 中日友好医院,北京 100029;
17. 昆明薇诺娜皮肤医疗美容有限公司,云南 昆明 650031;
18. 海南省皮肤病医院,海南 海口 570000;
19. 南京展超丽格医疗美容诊所,江苏 南京 210000;
20. 重庆大学附属医院,重庆 400038;
21. 武汉大学人民医院,湖北 武汉 430060;
22. 南京医科大学第一附属医院,江苏 南京 210029;
23. 曲靖市第一人民医院,云南 曲靖 655000;
24. 西南医科大学附属中医医院,重庆 400038;
25. 天津市中医药研究院附属医院( 长征医院) ,天津 300120;
26. 武汉市第一医院,湖北 武汉 430070
[学术秘书] 朱丽萍,E-mail: 13529062890@ 103. com