INTRODUCTION
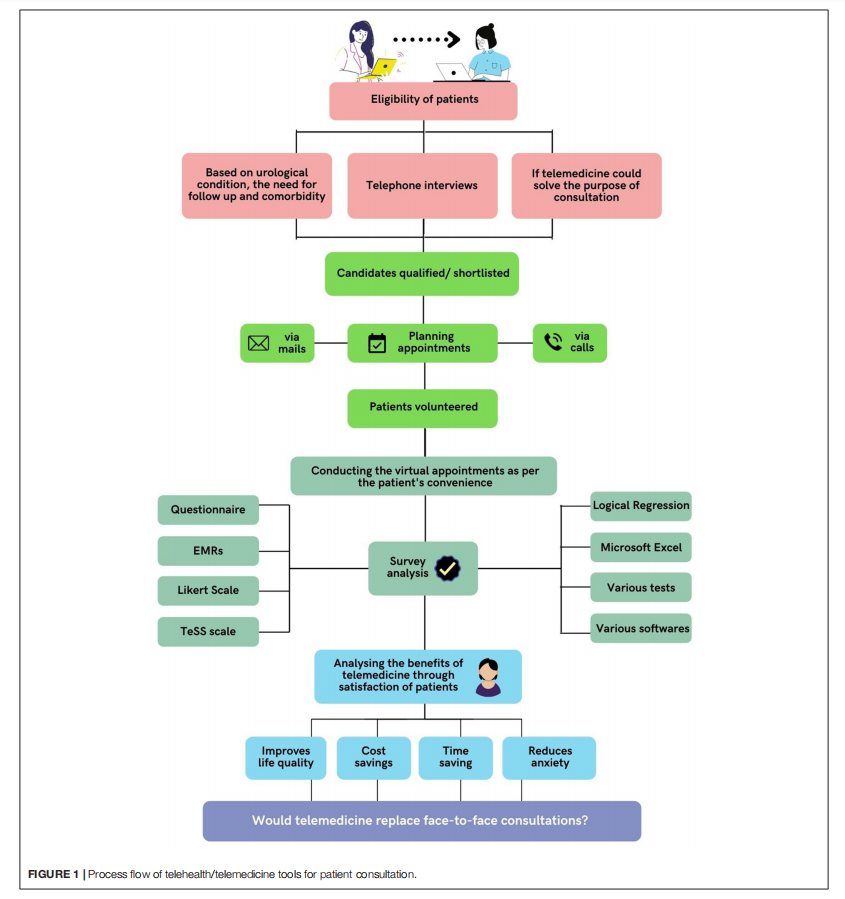
Telehealth is a rapidly developing healthcare that entails electronic communication between patients and clinicians, and telemedicine is a subset of telehealth (1). The WHO defines telemedicine as “the delivery of healthcare services, by all healthcare workers using the information and communication technologies for the exchange of dependable data for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and continuing education of healthcare providers, where distance is an important aspect” (2). The telephone utilization to minimize office visits was first documented in the Lancet in 1879. Telemedicine has evolved into a wide range of forms and uses electronic devices to improve healthcare delivery in various contexts (3). Video visits (VVs) have provided a real-time audio–visual substitute to traditional in-person appointments. Such an interactive communication model has allowed clinicians, patients, and families to communicate in real-time (4). Teleclinics have been reported to be successful in post-surgery and post-cancer therapy follow-up and provide consultation services for diagnosing patients with urolithiasis (5,6). Recent research has looked into the usage of video consulting in urology centers for hematuria referrals and follow-up appointments for a variety of illnesses, including benign prostatic hyperplasia (BPH), kidney stone disease (KSD), and urinary tract infections (UTIs), having greater levels of acceptability as well as fulfillment (7–9). Telemedicine has shown to be dependable and successful as a patient-care technique and has been effectively deployed in various healthcare settings and specialties (10–13).Figure 1 shows the process flow of telehealth/telemedicine tools that are used in patient consultation.
Benefits of Telemedicine in Healthcare
Telehealth has piqued the interest of clinicians and decisionmakers, particularly since the expanded usage of the internet, with its potential to reduce healthcare costs and improve convenience (14). It uses advanced telecommunication technology to improve healthcare accessibility and availability (15). Telemedicine has a favorable impact on patients and offers cost-saving (4, 16). Enhancements in the patients’ well-being, increased healthcare access in under-served areas, reduced travel time and expenses, shorter wait times, and fewer admissions in hospitals are a few of the benefits (17–19). Telemedicine has the potential to improve healthcare outcomes in the remote areas by lowering costs and boosting access to specialized treatments (20). It also ensures better information access (21). Other indirect advantages include increased adaptability in scheduling, increased availability of space in clinics and parking lots, reduced traffic, and reduced greenhouse gas emissions (22, 23).
Shin et al. (24), in their study, examined the patient contentedness and savings and clinical results of televisits in female pelvic medicine and reconstructive surgery at an urban educational center and identified that the patients reported a variety of savings, such as 88 (48.1%) of them saved at least 1 h in travel time and 54 (28.9%) saved more than $25 on transportation costs. The patient and family burden was reduced because 43 (23%) had a healthcare issue that made it hard to go for face-to-face appointments, 37 (19.8%) said that traveling for face-to-face appointments was grueling, and 41 (21.9%) said that doing a televisit allowed them to avoid taking time off work. More than half of all patients 94(51.4%) indicated they generally spend more than half an hour in the waiting area for face-to-face sessions (24).
Importance of Telemedicine During COVID-19
On March 20, 2020, the WHO proclaimed novel coronavirus disease-19 (COVID-19), caused by severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2), an epidemic (25). The SARS-CoV-2 infection and the burden of urgent and challenging healthcare situations and needs took varied forms around the world (26, 27). Before the pandemic, telemedicine was infrequently used for follow-up visits rather than new appointments (28). The pandemic provided an exceptional chance to evaluate the efficacy of telemedicine for both new and follow-up patient consultations, as most of these appointment sessions were conducted over the phone (29).
As the epidemic enters a more chronic phase (30), with possible peaks in the future, it is critical to strike a balance between virtual treatment and a secure environment for inperson appointments. The approach of conducting telephone interviews with approved clinical tools such as checklists and questionnaires has the potential to be widely used to manage the COVID-19 pandemic’s growing limitations successfully. It is a cost-effective and resource-efficient approach that protects both patients and healthcare providers while ensuring the care of vulnerable patients. (31). In addition, telephone interviews have the potential to provide social support to patients who are lonely, worried, and afraid of abandonment as a result of the pandemic (32).
Cancer remains the leading cause of death, and individuals are unwilling to compromise on their care. When there is a need for social separation, rapid introduction of telehealth is tolerated well, with a clear “red line” for alterations in the current interactions of patients and physicians. Human dignity in urooncology will be preserved by balancing future telemedicine implementation with the patients’ demands for personal contacts (33). Because of the immunosuppression and numerous routine hospital visits, the patients of cancer having systemic treatment may be at increased possibility of developing a critical case of COVID-19(27). Telehealth can safeguard cancer patients and healthcare providers from infections during face-to-face encounters, given the existing necessity for social and patient– physician separation (33).
Urology, Telemedicine, and COVID-19
Telemedicine in urology can reduce patient contact, lower infection rates among staff, allow isolated urologists to continue providing care (34). It can help with urological conditions such as monitoring kidney stones, renal cysts, and long-term lower urinary tract symptoms (LUTSs) management. Ureteric colic can also be diagnosed via phone appointment because its clinical setting is comparatively unharmful. Symptoms and scan results can be evaluated and relayed over the phone without a requirement for physical evaluation at a follow-up appointment (35, 36).
Despite the apparent advantages of telehealth, the long-term patient outcomes of urological telehealth are unknown (37). Some urologic oncology patients, mainly those with prostate cancer, have reported high satisfaction with telemedicine. Telemedicine visits were used as a consequent endpoint in a study of metformin in prostate cancer patients (38). Patients with prostate cancer who had undergone prostatectomy were highly satisfied with telemedicine (39). Apart from the prostate cancer population, the research on remote care in urologic oncology is still lacking (40). The COVID-19 epidemic has forced major changes in the healthcare worldwide, including urology (41). The pandemic has put a significant strain on hospital resources (42). As hospitals pose a substantial infection exposure through COVID-19 positive patients and asymptomatic exposed medical workers, deferred access for patient care has been suspended chiefly (43). In the COVID-19 scenario, urology is regarded as a non-essential clinical service by the international healthcare delivery system, even though the patient’s quality-of-life is significantly impacted by urological disease (44, 45).
Stay-at-home policies restricted the clinic visits, including urological visits (46). In such cases, telemedicine was a practical solution for providing patients with follow-up care (47, 48).
The COVID-19 pandemic has paved way for the technological advancements in the field of healthcare. Technology assisted consultation is proven to be beneficial for the patients (40, 49, 50). “Does the National Health Service (NHS) future lie in telephone consultations?” The results and experiences of the patients using NHS urology service’s with telemedicine for various urological issues included clinic types ranging from post-radical prostatectomy to PSA surveillance, general, functional, and andrology followup. Patients with lower urinary tract symptoms, hematuria, and stones were observed in the general urology clinic. Patients were not evaluated individually for telephone clinic eligibility. As a result, phone calls were used to discuss difficult management decisions and deliver bad news. During the pandemic, they discovered high levels of overall contentment with the usage of telephone appointments for urology patients. Patients in the PSA surveillance and post-radical prostatectomy clinics, on the other hand, reported significantly higher levels of satisfaction (50).
In a study for outpatient hematuria referrals, involving the implementation of teleurology with the help of teleconsultation to gather clinical information using a standardized algorithm, patients reported higher overall satisfaction and acceptance rates as an expedited evaluation strategy (7). Teleconsultation-based services increase urologic access by enabling asynchronous web-based consults and patient co-management between primary care providers and urologists. Patients in the neurourology unit frequently have disabilities that make travel difficult and necessitate the appearance of caregivers during medical appointments. Furthermore, these patients’ follow-up generally involves multiple visits, with all of the recognized effects regarding medication adherence, contentedness in general, personal uneasiness, and general and medical healthcare expenses.
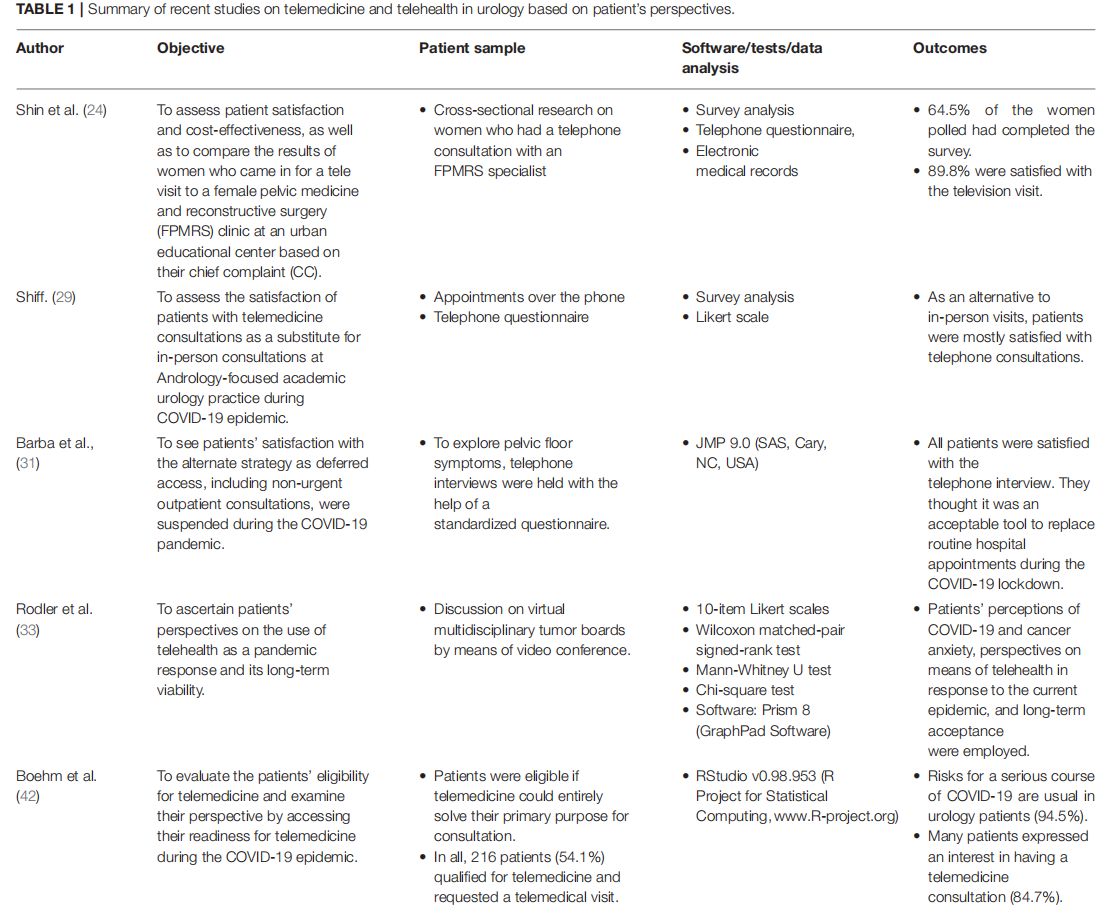
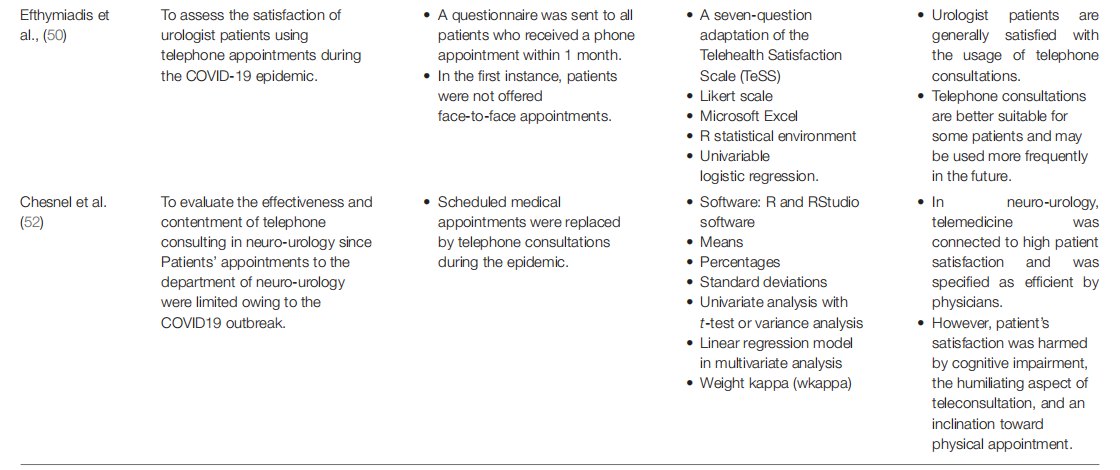
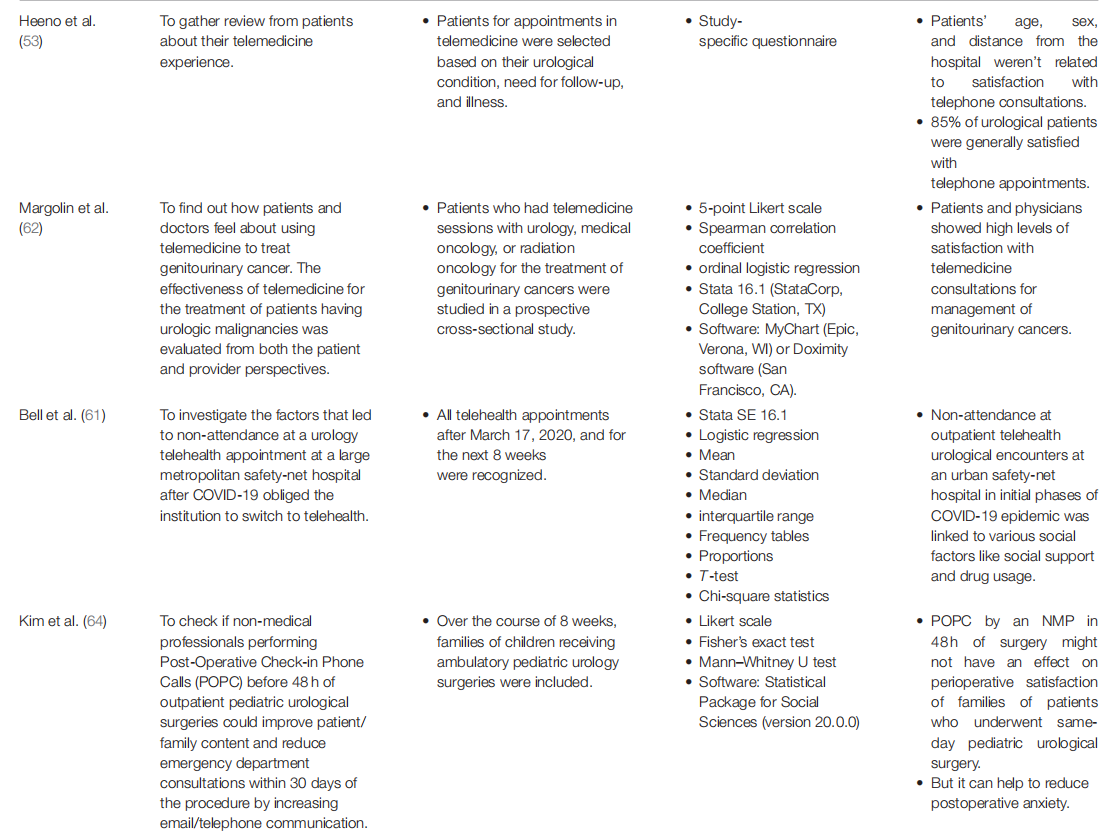
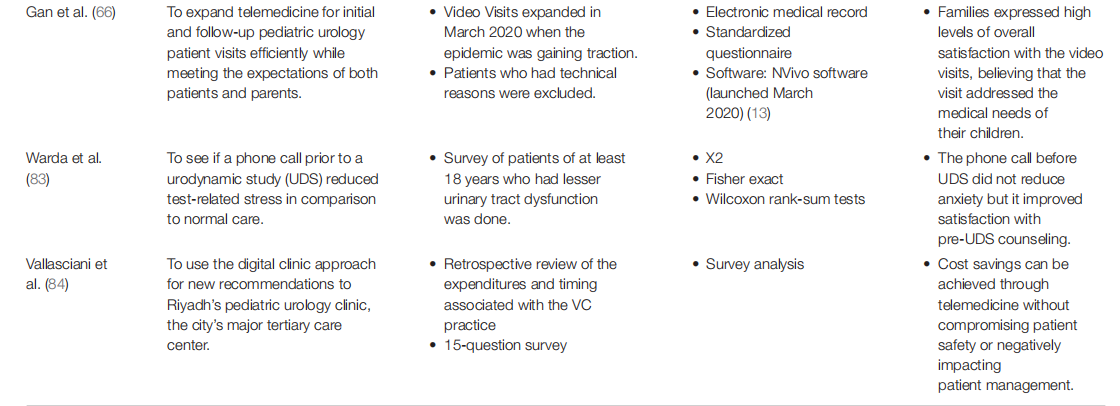
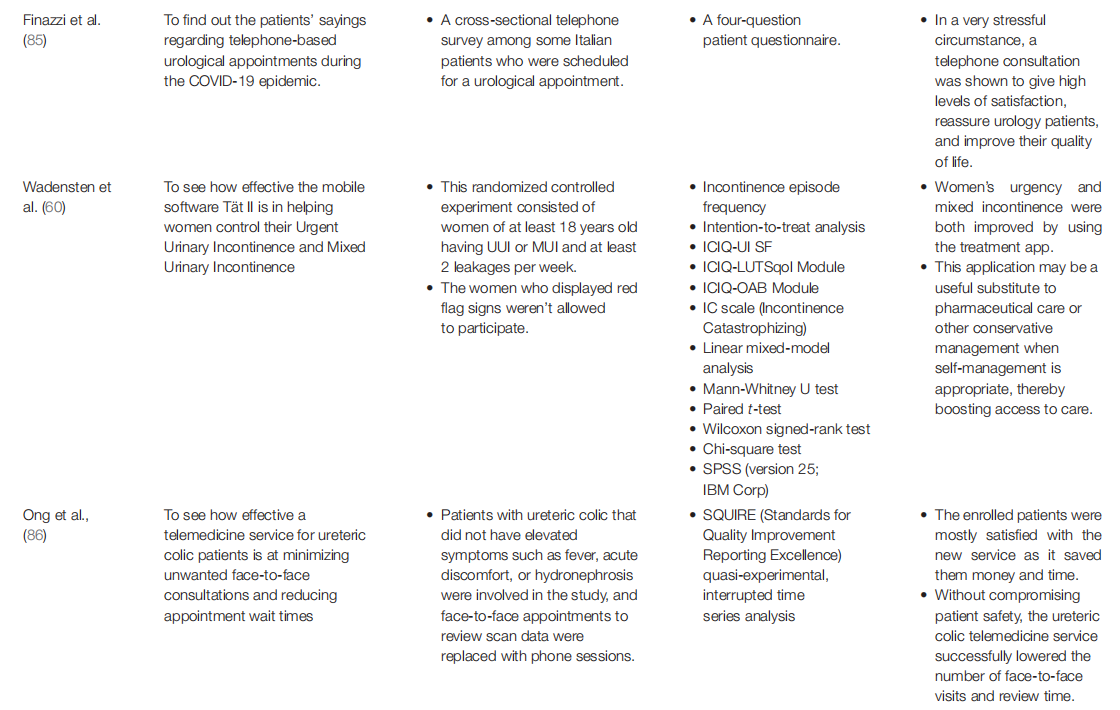
Telemedicine could be beneficial in patients attending neuro-urology appointments (51). In a recent report, clinicians used telemedicine to ensure patient follow-up at the neuro-urology department dealing with problems such as persisting urine incontinence, vesicoureteric reflux, and repetitive urinary tract infections, which are pretty common in neuro-urologic patients. Telephone consultation was used because of a delay in implementing telephone consultation (using video equipment) and cognitive impairment of a few of the patients. In conclusion, telemedicine in the area of neuro-urology was related to a significant level of patient satisfaction (52). Table 1 summarizes the recent studies on telemedicine and telehealth in urology based on patient’s perspectives.
The Perspective of Different Communities/Groups
It was observed in the studies that the patients’ age, gender, ethnicity, race, and distance from the hospital did not seem to be related to contentment associated with telephone consultations (52, 53). However, every healthcare system includes groups at risk of bad news, who may now face increased challenges due to a lack of digital literacy or access. Rural communities, elderly persons, ethnic/racial minority populations, people with low-socioeconomic positions, inadequate health education, and little English proficiency are more likely to face this obstacle (54–56).
Gender
Certain health conditions can cause feelings of disgrace, social separation, and low self-esteem, all of which can affect health-related quality-of-life (HRQoL) (57–59). Many women are affected by urgent urinary incontinence (UUI) and mixed urinary incontinence (MUI), significantly influencing their QoL. As a result, it is critical to provide effective treatment alternatives that can reach many patients, and eHealth technologies are fresh new ways to assist selfmanagement. Wadensten et al. (60), in their study, examined the usefulness of the mobile application Tät II for selfmonitoring of women having UUI and MUI and concluded that it was effective as the majority of the women who were present in the therapy group were happy with their treatment (60).
In their study, Shin et al. (24) attempted to assess the patient satisfaction and cost savings and analyzed visit outcomes using a main complaint of women for a televisit to the FPMRS clinic at an urban educational center. They did a cross-sectional review of all the women who finished a televisit to an FPMRS specialist at their institution and found out that 187 out of 290 (64.5%) women who were called completed the survey, and 168 (89.8%) of them were satisfied with the televisit. In total, 88 (48.1%) ended up saving at least 1 hour, and 54 (28.9%) saved more than $25 on transportation. In total, 99 (52.9%) televisits resulted in face-to-face follow-up, with chief complaint of prolapse (odds ratio [OR] = 4.2 (1.7– 10.3); p = 0.002), new patient (OR = 2.2 (1.2–4.2); p = 0.01), and Hispanic ethnicity (OR = 3.9 (1.2–13.6); p =.03) as considerable determinants. Because many participants were comfortable with FPMRS televisits at their urban academic center, telemedicine could become a main treatment within the FPMRS specialty even after the epidemic is gone. As more healthcare institutions adopt telemedicine, further research needs to be conducted to determine which patients will benefit the most from it (24).
Age
During the COVID-19 pandemic, Efthymiadis et al. surveyed patient satisfaction with telephone consultations, which was evaluated using an adaptation of the Telehealth Satisfaction Scale (TeSS). Patients who received a telephone appointment during 1 month were asked to fill out a survey. The patients’ responses were compared by the clinic type, age, and gender. Patients in post-radical prostatectomy and PSA surveillance clinics responded with more ’Excellent’ or ’Agree’ comments. A considerably higher number of ’Agree’ responses to one item was associated with older age. Gender had no bearing on the responses. The study found that urologist patients were quite satisfied with the utilization of telephone consultations. (50). However, older age was independently associated with lesser completed telemedicine visits.
Vulnerable Groups
Remarkably, common sociodemographic characteristics such as race/ethnicity, country of birth, and primary language were not linked to the chances of attending a telehealth appointment (61). Margolin et al., in their study, found no significant differences in patient satisfaction among vulnerable groups (e.g., elderly patients, Hispanic/Latino ethnicity, non-White race patients). The negative consequences of technology hurdles may be felt disproportionately by vulnerable communities, thus aggravating existing healthcare gaps (62). The usage of video for telemedicine appointments was shown to be less common in black and Latinx ethnicity people creating further disparity (63).
When the racial factor was taken into account, more than three-quarters (77%) of encounters were attended by ethnic/racial minorities, and the attended and non-attended encounters had similar racial/ethnic compositions. When other considerations were taken into account, homelessness/unstable housing had no impact on the chances of attending a telehealth visit (p = 0.13) (61). Less video-based telemedicine consultations were connected with the black race, lower household salary, and Latinx ethnicity (63).
Other Factors
Bell et al. (61), in their study, indicated that the married/partnered patients were in a higher percentage of attended encounters (88, 38.6%) than non-attended encounters (18, 19.2%, p = 0.001). Being single/widowed/divorced, having an active substance use problem, and having a new patient consultation were all linked to decreased attendance rates in multivariable analysis. The use of a language other than English as the patient’s chosen language and having Medicaid insurance were both linked to independently lesser completed telemedicine appointments (61).
Family Satisfaction
In a prospective study, Kim et al. (64) examined whether non-medical professionals (NMPs) performing post-operative check-in phone calls within 48 h of outpatient pediatric urological operations could improve patient/family contentment and reduce superfluous service utilization by increasing telephone/email communication and minimizing emergency department visits in 30 days of the process. This study suggested that well-defined perioperative guidelines and protocols can be the more significant factor in influencing patient and family happiness during the perioperative process. Moreover, it was concluded that the patient families undergoing same-day pediatric urology surgery might not be affected by a POPC made within 48 h of surgery. However, a 48-h post-operative consultation with a non-medical professional may help to alleviate post-operative anxiety. The POPCs provided improved educational and emotional assistance to most families in the pediatric age group receiving same-day tonsillectomies (65). Moreover, Gan et al. (66), in their study (66), identified that the families were generally satisfied with video visits (median score of 10/10), indicating that they met their child’s medical requirements satisfactorily. A telehealth visit was strongly recommended by 90% of families. Only 15.6% of the families reported visual or hearing problems, and 7.6% reported internet connectivity problems, suggesting that the great majority of families had no technical concerns.
Challenges
Telemedicine came with its own sets of difficulties, such as software flaws, a lack of video-compatible devices, a lack of highspeed internet, and individual technological fluency (67). Users and service providers alike experienced a variety of technical and connectivity challenges, including the visit’s poor audio and/or video quality and problems in logging into the mobile application (68). Some patient-facing health apps are difficult to use for people with little health literacy (69). Furthermore, in their design and user interface, some digital health products expressly take into consideration digital literacy, age, health literacy, and English proficiency (70, 71).
Recently introduced procedures and workflows such as mandating enrolment in an online patient website have artificially created further hurdles to telehealth, even though vulnerable people are less inclined to utilize patient portals (72, 73). Even though these are excellent techniques to ensure uptake, many healthcare systems do not supply training, teaching, or guidance to patients on using these technologies (72, 74). Moreover, according to some facilitators, the outside technical aspects associated with the technique of teleconsultation include the patient’s motivation, confidentiality, and familiarity with staff, and previous experience (52).
While a video visit is appropriate for most of the visits, the restrictions of remote diagnosis pose a difficulty for specific diagnoses. For example, the testing of an undescended testicle was inconsistent, and clinicians would prefer an in-person review in the future. The necessity for radiographic imaging is yet another issue that arises but is more easily solved. In this situation, some families received studies and mailed or had them transmitted electronically to the clinical team before the scheduled video consultation, facilitating inspection. Coordination of this procedure can be time-demanding for all the parties involved (66).
Furthermore, given the COVID-19 pandemic, the patient’s satisfaction during the telephone consultation may be overrated (52). The encounter was deemed to have had significant technological challenges if the patient or physician reported on the survey that they had the visit over the phone without video or that the platform did not perform well enough to complete the visit as intended (62). Despite having access to the technology of mobiles, elderly patients, those from poorer socio-economic backgrounds, and those who do not speak English fluently are less inclined to use the health technologies (75, 76).
Barriers to Telemedicine
Despite being shown to be beneficial and successful in healthcare settings, telemedicine has limitations and obstacles. It has yet to gain widespread acceptance in the urological community because of various restrictions including patient and physician acceptability, licensure and responsibility, costs, safety, and concerns with ethical issues. A systematic review of the global challenges to telemedicine adoption found that technology specific concerns were the major barriers to telemedicine usage, with technically challenged employees being the most commonly identified impediment (77).
The pandemic period was difficult for healthcare delivery and resulted in legislative reforms that acted as a spur for us to better comprehend this previously untapped resource. Despite regulatory and legislative improvements aimed at encouraging the use of telemedicine, the financial expense of adopting it may remain a barrier for small practices (78). This implementation will continue to need careful planning, procedures and processes, and rigorous assessment to maintain the long-term viability of telemedicine and telehealth beyond the COVID-19 pandemic. Critics of telehealth use are also concerned that it will have a negative impact on the continuity of care, stating that online interactions are impersonal and unsafe since the virtual physician lacks the advantage of a comprehensive history and physical examination to help in diagnosis and treatment (79, 80).
This is particularly true in cases of chronic illnesses and malignant diseases where a thorough physical examination is of paramount importance even from the perspective of a clinician to guide the investigations and management. Ease of access, ability to use, and the design of interface being used to provide telehealth services continue to be the major technological factors limiting the use of telemedicine.
Future Predictions of Usage of Telemedicine in the Post COVID-19 Situation
The rapid digitalization of our communities has resulted in higher levels of mobile connectivity, including in emerging economies, so a higher uptake of telemedicine is anticipated (81). Telemedicine is better suited for long-term follow-up as well as reports on chronic illnesses, as evidenced by the findings. Moreover, as telemedicine becomes more common in the specialty, validated tools for urology patients and specific patient populations will be helpful in upcoming studies. Patients in the post-radical prostatectomy and PSA surveillance clinics reported considerably higher satisfaction levels. This suggests that telemedicine will be used to some extent when the COVID- 19 epidemic is over (50). Telemedicine can be used effectively in pediatric urology for various visit types, including unfamiliar, return, and post-operative consultations, with comprehensive favorable feedback from the families (66).
However, face-to-face consultations are essential in some circumstances for a safe and full clinical assessment. So, face-to-face appointments, which are superior for breaking bad news and checking acutely ill patients, cannot be replaced by telemedicine. Telemedicine should not be used to treat diseases that require a medical assessment or extensive discussions. Due to privacy concerns, people with sexual health disorders may be less eager to participate in telemedicine (8). Many patients prefer face-to-face appointments over phone consultations for personal reasons, and this should be acknowledged while keeping patient’s and practitioner’s safety in mind. So, as part of a patient-centered approach, the choice of telephone and remote consultations must be made available to the relevant patients (50).
Moreover, to avoid increasingly existing disparities, recognizing people at greater possibility of non-attendance because of reasons such as inadequate digital literacy, insecure housing, or substance use disorder is critical (82). As a result, healthcare organizations will need to minimize technological barriers to increase telehealth availability and acceptance among vulnerable groups. To achieve fair access to telemedicine, physicians and healthcare institutions will need to make informed, integrated, and intentional efforts (61).
CONCLUSION
Telemedicine, which refers to delivering healthcare to the patients who are not at the physician’s exact location, is associated with many benefits and overall patient engagement and satisfaction. It is better suited for long-term follow-up and assessment of long-standing conditions and has played a vital part in the present global COVID-19 pandemic, delivering timely patient service while simultaneously ensuring the social distancing required to avert the transmission of infectious diseases. Being a cost-effective and resource-efficient solution, it also provides additional social support to lonely and anxious patients due to the pandemic.
However, telemedicine presents its own set of potential hurdles such as software faults, a shortage of video-compatible devices, a lack of high-speed internet, and individual expertise. Besides, the rural section, elderly, ethnic/racial minority populations, and people having minor socioeconomic status, poor-health literacy, and narrow proficiency in English are more susceptible to the technological barriers. But, the choice of having telephone and remote consultations must be made accessible to appropriate patients as part of a patient-centered strategy. Healthcare organizations will need to develop strategies to eliminate technological barriers to improve telehealth accessibility and acceptance among everyone. To achieve fair access to telemedicine, physicians and healthcare institutions will need to make informed, coordinated, and intentional efforts.
AUTHOR CONTRIBUTIONS
NN, DS, BH, and BS contributed to the conception and design of the study. MS, SI, SN, AG, AN, and NK organized the database. SN, AG, AN, DM, KD, and SI wrote the first draft of the manuscript. NN, DM, DS, BR, SN, and BH wrote sections of the manuscript. PC, BR, and BS critically reviewed and edited the manuscript. All authors contributed to manuscript revision,read, and approved the submitted version.
REFERENCES
1. Mechanic OJ, Kimball AB. Telehealth systems. FL: StatPearls Treasure Island. (2020).
2. A Health Telematics policy in support of who’s health-for-all strategy for Global Health Development : Report of the WHO Group Consultation on Health Telematics, 11–16 December, Geneva, 1997. World Health Organization. (1998). Available online at: https://apps.who.int/iris/handle/ 10665/63857 (accessed March 3, 2022)
3. Castaneda P, Ellimoottil C. Current use of telehealth in urology: a review. World J Urol. (2019) 38:2377–84. doi: 10.1007/s00345-019-02882-9
4. Powell RE, Stone D, Hollander JE. Patient and health system experience with implementation of an enterprise-wide telehealth scheduled video visit program: mixed-methods study. JMIR Med Inform. (2018) 6: e10. doi: 10.2196/medinform.8479
5. Brada M, James ND. Phone clinic provides excellent support. BMJ. (1995) 310:738–738. doi: 10.1136/bmj.310.6981.738
6. James ND, Guerrero D, Brada M. Who should follow up cancer patients? nurse specialist based outpatient care and the introduction of a phone clinic system. Clin Oncol. (1994) 6:283–7. doi: 10.1016/S0936-6555(05)80267-5
7. Safir IJ, Gabale S, David SA, Huang JH, Gerhard RS, Pearl J, et al. Implementation of a tele-urology program for outpatient hematuria referrals: initial results and patient satisfaction. Urology. (2016) 97:33–9. doi: 10.1016/j.urology.2016.04.066
8. Viers BR, Pruthi S, Rivera ME, O’Neil DA, Gardner MR, Jenkins SM, et al. Are patients willing to engage in telemedicine for their care: a survey of preuse perceptions and acceptance of remote video visits in a urological patient population. Urology. (2015) 85:1233–40. doi: 10.1016/j.urology.2014.12.064
9. Andino JJ, Castaneda PR, Shah PK, Ellimoottil C. The impact of video visits on measures of clinical efficiency and reimbursement. Urol Pract. (2021) 8:53–7. doi: 10.1097/UPJ.0000000000000149
10. Levine SR, Gorman M.“Telestroke”. Stroke. (1999) 30:464–9. doi: 10.1161/01.STR.30.2.464
11. Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: an acceptable telehealth model for rural patients and health workers. Intern Med J. (2012) 42:780– 5. doi: 10.1111/j.1445-5994.2011.02537.x
12. Donelan K, Barreto EA, Sossong S, Michael C, Estrada JJ, Cohen AB. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. (2019) 25:40–4.
13. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. (2018) 178:745. doi: 10.1001/jamainternmed.2018.1314
14. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. (2016) 375:154–61. doi: 10.1056/NEJMra1601705
15. Jennett PA, Hall LA, Hailey D, Ohinmaa A, Anderson C, Thomas R, et al. The socio-economic impact of telehealth: a systematic review. J Telemed Telecare. (2003) 9:311–20. doi: 10.1258/135763303771005207
16. Whited JD. Economic analysis of telemedicine and the teledermatology paraTelemed J E Health. (2010) 16:223–8. doi: 10.1089/tmj.200 9.0100
17. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol. (2020) 204:144–8. doi: 10.1097/JU.0000000000000750
18. Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer survivors: a systematic review and meta-analysis. Health Informatics J. (2019) 26:1060–78. doi:10.1177/14604582 19863604
19. Rimsza ME, Hotaling AJ, Keown ME, Marcin JP, Moskowitz WB, Sigrest TD, et al. The use of telemedicine to address access and physician workforce shortages. Pediatrics. (2015) 136:202–9. doi: 10.1542/peds.201 5-1253
20. Malasanos TH, Burlingame JB, Youngblade L, Patel BD, Muir AB. Improved access to subspecialist diabetes care by telemedicine: Cost savings and care measures in the first two years of the fite diabetes project. J Telemed Telecare. (2005) 11:74–6. doi: 10.1258/1357633054461624
21. Hjelm NM. Benefifits and drawbacks of telemedicine. J Telemed Telecare. (2005) 11:60–70. doi: 10.1258/1357633053499886
22. Zholudev V, Safifir IJ, Painter MN, Petros JA, Filson CP, Issa MM. Comparative cost analysis: teleurology vs conventional face-to-face clinics. Urology. (2018) 113:40–4. doi: 10.1016/j.urology.2017.07.034
23. Bator EX, Gleason JM, Lorenzo AJ, Kanaroglou N, Farhat WA, Bägli DJ, et al. The burden of attending a pediatric surgical clinic and family preferences toward telemedicine. J Pediatr Surg. (2015) 50:1776– 82. doi: 10.1016/j.jpedsurg.2015.06.005
24. Shin C, Allen AZ, Zhu D, Tellechea L, Watts KL, Abraham NE. Patient satisfaction and savings, and clinical outcomes of televisits in female pelvic medicine and reconstructive surgery at an urban academic center. Neurourol Urodyn. (2021) 40:1834–44. doi: 10.1002/nau.24759
25. Coronavirus Disease (Covid-19) Situation Reports. World Health Organiztion. Available online at: https://www.who.int/emergencies/diseases/ novel-coronavirus-2019/situation-reports (accessed March 7, 2022).
26. Guan W-jie, Ni Z-yi, Hu Y, Liang W-hua, Ou C-quan, He J-xing, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
27. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-COV-2 infection: a nationwide analysis in China. Lancet Oncol. (2020) 21:335–7. doi: 10.1016/S1470-2045(20)30096-6
28. Badalato GM, Kaag M, Lee R, Vora A, Burnett A. Role of telemedicine in urology: contemporary practice patterns and future directions. Urology Pract. (2020) 7:122–6. doi: 10.1097/UPJ.0000000000000094
29. Shiff B, Frankel J, Oake J, Blachman-Braun R, Patel P. Patient satisfaction with telemedicine appointments in an academic andrology-focused urology practice during the COVID-19 pandemic. Urology. (2021)
153:35–41. doi: 10.1016/j.urology.2020.11.065
30. Coronavirus Disease 2019 (COVID-19) daily ... - rki.de. Available online at: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/ Situationsberichte/Nov_2021/2021-11-25-en.pdf __blob=publicationFile (accessed March 7, 2022)
31. Barba M, Manodoro S, Bosio S, Locatelli L, Frigerio M. Telephone interview in urogynecology in the era of covid-19 pandemic. J Turk Ger Gynecol Assoc. (2021) 22:8–11. doi: 10.4274/jtgga.galenos.2020.2020.0131
32. Hollander JE, Carr BG. Virtually perfect? telemedicine for covid-19. N Engl J Med. (2020) 382:1679–81. doi: 10.1056/NEJMp2003539
33. Rodler S, Apfelbeck M, Schulz GB, Ivanova T, Buchner A, Staehler M, et al. Telehealth in uro-oncology beyond the pandemic: toll or lifesaver? Eur Urol Focus. (2020) 6:1097–103. doi: 10.1016/j.euf.2020.0 5.010
34. Miller A, Rhee E, Gettman M, Spitz A. The current state of telemedicine in urology. Med Clin North Am. (2018) 102:387–98. doi: 10.1016/j.mcna.2017.10.014
35. Ellimoottil C, Skolarus T, Gettman M, Boxer R, Kutikov A, Lee BR, et al. Telemedicine in urology: state of the art. Urology. (2016) 94:10– 6. doi: 10.1016/j.urology.2016.02.061
36. Glassman DT, Puri AK, Weingarten S, Hollander JE, Stepchin A, Trabulsi E, et al. Initial experience with telemedicine at a single institution. Urology Pract. (2018) 5:367–71. doi: 10.1016/j.urpr.2017.08.004
37. Gadzinski AJ, Ellimoottil C. Telehealth in urology after the covid- 19 pandemic. Nat Rev Urol. (2020) 17:363–4. doi: 10.1038/s41585-020- 0336-6
38. Galsky MD, Shahin M, Jia R, Shaffffer DR, Gimpel-Tetra K, Tsao C-K, et al. Telemedicine-enabled clinical trial of metformin in patients with prostate cancer. JCO Clin Cancer Inform. (2017)1–10. doi: 10.1200/CCI.17.00044
39. Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Effifficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. (2015) 68:729–35. doi: 10.1016/j.eururo.2015.04.002
40. Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, et al. Telehealth in urology: a systematic review of the literature. how much can telemedicine be useful during and after the covid-19 pandemic? Eur Urol. (2020) 78:786–811. doi: 10.1016/j.eururo.2020.06.025
41. Simonato A, Giannarini G, Abrate A, Bartoletti R, Crestani A, De Nunzio C, et al. Clinical pathways for urology patients during the COVID-19 pandemic. Minerva Urol Nefrol. (2020) 72: 376-83. doi: 10.23736/S0393-2249.20.03861-8
42. Boehm K, Ziewers S, Brandt MP, Sparwasser P, Haack M, Willems F, et al. Telemedicine online visits in urology during the covid-19 pandemic—potential, risk factors, and patients’ perspective. Eur Urol. (2020) 78:16–20. doi: 10.1016/j.eururo.2020.04.055
43. Ferreira R, McGrath M, Wang Y, Sener A, Siemens DR, Braga LH. How to prioritize urological surgeries during epidemics: lessons learned from the toronto sars outbreak in 2003. Can Urological Association J. (2020) 14:E159–60. doi: 10.5489/cuaj.6551
44. Stensland KD, Morgan TM, Moinzadeh A, Lee CT, Briganti A, Catto JWF, et al. Considerations in the triage of urologic surgeries during the covid-19 pandemic. Eur Urol. (2020) 77:663–6. doi: 10.1016/j.eururo.2020.03.027
45. Ling Y, Xu S-B, Lin Y-X, Tian D, Zhu Z-Q, Dai F-H, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J. (2020) 133:1039–43. doi: 10.1097/CM9.0000000000000774
46. Phé V, Karsenty G, Robert G, Gamé X, Cornu J-N. Widespread postponement of functional urology cases during the COVID-19 pandemic: rationale, potential pitfalls, and future consequences. Eur Urol. (2020) 78:4– 5. doi: 10.1016/j.eururo.2020.04.031
47. Kim T, Zuckerman JE. Realizing the potential of telemedicine in Global Health. J Glob Health. (2019) 9:020307. doi: 10.7189/jogh.09.020307
48. Kane-Gill SL, Rincon F. Expansion of telemedicine services. Crit Care Clin. (2019) 35:519–33. doi: 10.1016/j.ccc.2019.02.007
49. Grimes CL, Balk EM, Crisp CC, Antosh DD, Murphy M, Halder GE, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: review of existing evidence. Int Urogynecol J. (2020) 31:1063–89. doi: 10.1007/s00192-020-04314-4
50. Efthymiadis A, Hart EJM, Guy AM, Harry R, Mahesan T, Chedid WA, et al. Are telephone consultations the future of the NHS? the outcomes and experiences of an NHS urological service in moving to telemedicine. Future Hosp J. (2020) 8:e15–20. doi: 10.7861/fhj.2020-0076
51. Huri E, Hamid R. Technology-based management of neurourology patients in the COVID-19 pandemic: is this the future? a report from the International Continence Society (ICS) Institute. Neurourol Urodyn. (2020) 39:1885–8. doi: 10.1002/nau.24429
52. Chesnel C, Hentzen C, Le Breton F, Turmel N, Tan E, Haddad R, et al. Efficiency and satisfaction with telephone consultation of follow-up patients in neuro-urology: experience of the covid-19 pandemic. Neurourol Urodyn. (2021) 40:929–37. doi: 10.1002/nau.24651
53. Heeno E, Biesenbach I, Englund C, Lund M, Toft A, Lund L. Patient perspective on telemedicine replacing physical consultations in urology during the COVID-19 lockdown in Denmark. Scand J Urol. (2021) 55:177– 83. doi: 10.1080/21681805.2021.1906317
54. Tsai H-yi S, Shillair R, Cotten SR. Social support and “playing around.” J Appl Gerontol. (2016) 36:29–55. doi: 10.1177/0733464815609440
55. Nouri SS, Avila-Garcia P, Cemballi AG, Sarkar U, Aguilera A, Lyles CR. Assessing mobile phone digital literacy and engagement in usercentered design in a diverse, safety-net population: mixed methods study. JMIR Mhealth Uhealth. (2019) 7:e14250. doi: 10.2196/pre prints.14250
56. Donovan KA, Walker LM, Wassersug RJ, Thompson LM, Robinson JW. Psychological effects of androgen-deprivation therapy on men with prostate cancer and their partners. (2015) 121:4286–99. doi: 10.1002/cncr.29672
57. Siddiqui NY, Levin PJ, Phadtare A, Pietrobon R, Ammarell N. Perceptions about female urinary incontinence: a systematic review. Int Urogynecol J. (2013) 25:863–71. doi: 10.1007/s00192-013-2276-7
58. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: Results from the epic study. BJU Int. (2008) 101:1388–95. doi: 10.1111/j.1464-410X.20 08.07601.x
59. Coyne KS, Zhou Z, Thompson C, Versi E. The impact on health-related quality of life of stress, urge and mixed urinary incontinence. BJU Int. (2003) 92:731–5. doi: 10.1046/j.1464-410X.2003.04463.x
60. Wadensten T, Nyström E, Franzén K, Lindam A, Wasteson E, Samuelsson E. A mobile app for self-management of urgency and mixed urinary incontinence in women: Randomized controlled trial. J Med Internet Res. (2021) 23:e19439. doi: 10.2196/19439
61. Bell A, Lonergan PE, Escobar D, Fakunle M, Chu CE, Berdy S, et al. A cross-sectional analysis of barriers associated with nonattendance at a urology telehealth clinic in a safety-net hospital. Urology. (2021). doi: 10.1016/j.urology.2021.08.025. [Epub ahead of print].
62. Margolin EJ, Pina Martina LA, Miles CH, Wenske S, McKiernan JM, DeCastro GJ, et al. Telemedicine in management of genitourinary malignancies: Patient and physician perspectives. Urol Oncol. (2021) 39:480–
6. doi: 10.1016/j.urolonc.2021.04.003
63. Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SA, Nathan AS, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640
64. Kim JK, Lee MJ, Chua ME, Ming JM, Lorenzo AJ, Farhat WA, et al. Do post-operative phone calls enhance family satisfaction and outcomes after outpatient pediatric urological surgeries? a prospective study. Pediatr Surg Int. (2020) 37:161–7. doi: 10.1007/s00383-020-04770-5
65. Le T, Drolet J, Parayno E, Rosmus C, Castiglione S. Follow-up phone calls after pediatric ambulatory surgery for tonsillectomy: what can we learn from families? J Perianesth Nur. (2007) 22:256–64. doi: 10.1016/j.jopan.2007.05.004
66. Gan Z, Lee SY, Weiss DA, Van Batavia J, Siu S, Frazier J, et al. Single institution experience with telemedicine for pediatric urology outpatient visits: adapting to covid-19 restrictions, patient satisfaction, and future utilization. J Pediatr Urol. (2021) 17:e1–480.e7. doi: 10.1016/j.jpurol.2021.05.012
67. Gray DM, Joseph JJ, Olayiwola JN. Strategies for digital care of vulnerable patients in a COVID-19 world-keeping in touch. JAMA Health Forum. (2020) 1:e200734. doi: 10.1001/ jama health forum.2020.0734
68. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. (2016) 24:4–12. doi: 10.1177/1357633X16674087
69. Sarkar U, Gourley GI, Lyles CR, Tieu L, Clarity C, Newmark L, et al. Usability of commercially available mobile applications for diverse patients. J Gen Intern Med. (2016) 31:1417–26. doi: 10.1007/s11606-016-3771-6
70. Lyles CR, Sarkar U. Health Literacy, vulnerable patients, and health information technology use: where do we go from here? J Gen Intern Med. (2015) 30:271–2. doi: 10.1007/s11606-014-3166-5
71. Nouri SS, Adler-Milstein J, Thao C, Acharya P, Barr-Walker J, Sarkar U, et al. Patient characteristics associated with objective measures of digital health tool use in the United States: a literature review. J Am Med Inform Assoc. (2020) 27:834–41. doi: 10.1093/jamia/ocaa024
72. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc. (2019) 26:855– 70. doi: 10.1093/jamia/ocz023
73. Sinha S, Garriga M, Naik N, McSteen BW, Odisho AY, Lin A, et al. Disparities in electronic health record patient portal enrollment among oncology patients. JAMA Oncology. (2021) 7:935. doi: 10.1001/jama oncol.2021.0540
74. Lyles CR, Tieu L, Sarkar U, Kiyoi S, Sadasivaiah S, Hoskote M, et al. A randomized trial to train vulnerable primary care patients to use a patient portal. J Am Board Fam Med. (2019) 32:248–58. doi: 10.3122/jabfm.2019.02. 180263
75. James DC, Harville C, Sears C, Efunbumi O, Bondoc I. Participation of African Americans in e-health and M-health studies: a systematic review. Telemed J E Health. (2017) 23:351–64. doi: 10.1089/tmj.2016.0067
76. Bommakanti KK, Smith LL, Liu L, Do D, Cuevas-Mota J, Collins K, et al. Requiring smartphone ownership for mhealth interventions: who could be left out? BMC Public Health. (2020) 20:1–9. doi:10.1186/s12889-019-7892-9
77. Dubin JM, Wyant WA, Balaji NC, Ong WLK, Kettache RH, Haffaf M, et al. Telemedicine usage among urologists during the COVID- 19 pandemic: cross-sectional study. J Med Internet Res. (2020) 22:e21875. doi: 10.2196/preprints.21875
78. Kane CK, Gillis K. The use of telemedicine by physicians: Still the exception rather than the rule. Health Aff. (2018)37:1923–30. doi: 10.1377/hlthaff.2018.05077
79. Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. (2021) 17:218–21. doi: 10.1016/j.nurpra.2020.09.013
80. Naik N, Ibrahim S, Sircar S, Patil V, Hameed BM, Rai BP, et al. Attitudes and perceptions of outpatients towards adoption of telemedicine in healthcare during COVID-19 pandemic. Ir J Med Sci. (2021). doi: 10.1007/s11845-021-02729-6. [Epub ahead of print].
81. Bahia K, Suardi S. The State of Mobile Internet Connectivity. London: Groupe Spécial Mobile Association (GSMA) (2019).
82. Nouri SS, Khoong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery (2020)
83. Warda H, Hacker MR, Haviland MJ, Hota LS. A telephone call to decrease patient anxiety before urodynamic testing: a randomized controlled trial. Female Pelvic Med Reconstr Surg. (2018) 25:378–82. doi: 10.1097/SPV.0000000000000568
84. Vallasciani S, Abdo B, Rauf Z, Anjum A, Ghulman S, Alghammas H, et al. Telehealth for the assessment of patients referred for pediatric urological care: a preliminary cost savings analysis and satisfaction survey. Telemed J E Health. (2019) 25:756–61. doi: 10.1089/tmj.2018.0159
85. Finazzi Agrò E, Farullo G, Balzarro M, Del Popolo G, Giannantoni A, Herms A, et al. Triage of functional, female and neuro-urology patients during and immediately after the covid-19 outbreak. Minerva Urol Nefrol. (2020) 72:513–15. doi: 10.23736/S0393-2249.20.03909-0
86. Ong CS, Lu J, Tan YQ, Tan LG, Tiong HY. Implementation of a ureteric colic telemedicine service: a mixed methods quality improvement study. Urology. (2021) 147:14–20. doi: 10.1016/j.urology.2020.10.010
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Copyright © 2022 Naik, Hameed, Nayak, Gera, Nandyal, Shetty, Shah, Ibrahim,Naik, Kamath, Mahdaviamiri, D’costa, Rai, Chlosta and Somani. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
This article is excerpted from the Frontiers in Surgery by Wound World.