
伤口世界

- 星期四, 19 10月 2023
Building the business case for shared wound care: a cost-benefit case for service providers
Chronic wounds are a substantial burden on healthcare systems worldwide, with their management accounting for a significant portion of healthcare budgets. Given the rising prevalence of wounds and the growing strain on healthcare resources, there is an urgent need for more efficient treatment options in wound care.
Authors:
Zena Moore and Sebastian Probst
Zena Moore PhD, MSc, FFNMRCSI, PG Dip, RGN is Professor and Head of the School of Nursing and Midwifery, Director of the Skin Wounds and Trauma Research Centre, Royal College of Surgeons in Ireland, University of Medicine and Health Sciences, Dublin, Ireland;
Sebastian Probst DClinPrac, MNS, BNS, RN is Full Professor of Tissue Viability and Wound Care, Geneva School of Health Sciences, HES-SO University of Applied Sciences and Arts Western Switzerland, Care Directorate, University Hospital Geneva, Switzerland and Adjunct Professor, Faculty of Medicine, Nursing and Health Sciences, Monash University, Melbourne, Australia
* The data set used to create the 3.5 billion hour model (Moore et al, 2022), revealed that globally, 4,011,188,929 hours are spent on dressing changes in the community per year. ALLEVYN LIFE Dressing as part of a shared wound care approach has the potential to release 10.8% (433,208,404) of these hours (Joy et al, 2015; Moore et al, 2022; Rossington et al, 2013; Simon and Bielby, 2014; Tiscar-González et al, 2021).
- 星期三, 18 10月 2023
Paving the way for effective wound care education for the non-specialist — developing five evidence-based wound type specific pathways
The Wound Care Pathway was developed in 2020/21 to provide a practical, evidence-based step-by-step approach towards wound healing (Dowsett et al, 2021). Healthcare providers who use the pathway asked for more detailed guidance for specific wound types. A group of wound care experts, comprised of physicians, nurses and researchers, undertook a process to expand the international consensus on wound healing by developing wound type-specific pathways for diabetic foot ulcers, venous leg ulcers, skin tears, pressure injuries/pressure ulcers and surgical wound dehiscence. The objective was to take complex research evidence and translate it into simple and practical treatment guidance for the non-specialist, for the five most common wound types. The systematic approach to wound care provided in the wound care pathway and in the wound type specific pathways is designed with the goal of achieving a shorter way to wound healing by helping healthcare providers focus on healing wounds not just dressing wounds.
Authors:
Terry Swanson, Kimberly Bain,Caroline Dowsett, Jose Ramon March Garcia, Emily Greenstein, David Keast, Long Zhang, Mark Bain, Hester Colboc and Christoffer Hoffmann
Terry Swanson is Nurse Practitioner
Wound Management, Warrnambool, Vic. Australia;
Kimberly Bain is Senior Partner - Consensus Building, BainGroup Consulting, Canada;
Caroline Dowsett is Nurse Specialist Tissue Viability, East London NHS Foundation Trust London, UK;
Jose Ramon March Garcia is Vascular Surgeon Getafe University Hospital (Madrid), Spain;
Emily Greenstein is Certified Nurse Practitioner at Sanford Health in Fargo, USA;
David Keast is Associate Scientist, Lawson Health Research institute, Canada;
Long Zhang is Vascular Surgeon, Wound Healing Center, Peking University Third Hospital,China;
Mark Bain is Senior Partner, Data Strategy, BainGroup Consulting, Canada;
Hester Colboc is Dermatologist & Gerontologist, Rothschild Hospital, Paris, France;
Christoffer Hoffmann is Senior Medical Specialist, Coloplast A/S, Denmark
- 星期二, 17 10月 2023
运动训练对老年糖尿病周围神经病变患者平衡功能影响的Meta 分析
臧娴,白姣姣,王怡
复旦大学附属华东医院护理部,上海200040
[摘要]目的评价运动训练对老年糖尿病周围神经病变(DPN)患者平衡功能的影响。方法计算机检索Cochrane Library、JBI、MEDLINE、EMbase 、PubMed、 Web of Science、中国生物医学文献数据库( CBM)、中国知网(CNKI) 及万方数据库中(自建库至2017年2月5日)关于运动训练对老年DPN患者平衡功能影响的随机对照试验( randomized controlled tria,RCT), 由2名研究员按纳入和排除标准筛选文献、提取资料并评价质量,然后采用RevMan 5.3软件进行Meta分析。结果共纳人6个RCT, 373例老年DPN患者。Meta分析结果显示,运动训练可延长老年DPN患者的睁眼/闭眼单足站立时间[WMD=3.8, 95%CI (2.38 ~5.22), P<0.0000; WMD= 1.66, 95%CI (0.86 ~2.46),P<0.0001],增加Berg平衡功能量表得分[WMD=1.34, 95%CI (0.93~ 1.75), P<0.000],缩短计时起立一步行测试时间[WMD=-1.37. 95%CI (-1.69~-1.05), P<0000]。结论运动训练可显著改善老年DPN患者的静态和动态平衡功能,临床上应注重对老年DPN患者进行运动训练,从而改善其平衡功能,降低跌倒风险。
[关键词]糖尿病;周围神经病变;运动训练;平衡功能; Meta 分析
Effect of Exercise Training on Balance Function of the Elderly with Diabetic Peripheral Neuropathy: A Meta Analysis
Zang Xian, Bai Jaojao*,Wang Yi
Department of Nursing, Huadong Hospital Afiliated 10 Fudan University, Shanghai, 200040. P. R. China
*Corresponding author: Bai Jiaojiao, E-mail: bjj163163@163. com
[ABSTRACT] Objective To evaluate the effect of exercise training on the balance function of the elderly with diabetic peripheral neuropathy (DPN). Methods Papers with randomized controlled trials (RCT) involving the effect of exercise training on the balance function of the elderly with DPN, published since the setup of the databases to Feb.5 th, 2015, were searched in Cochrane Library, JBI, MEDLINE, EMbase, PubMed, Web of Science, CBM, CNKI and WanFang Data; according to the inclusion and exclusion criteria, the papers were screened by 2 researchers; data were extracted and the meth-
odological quality of the included was asessed. Result In total, 6 RCTs involving 373 elderly with DPN were included; Meta analysis indicated that after exercise training, the elderly with DPN had a longer time of one leg stance with eyes opening (WMD=3.8, 95%CI2.38-5.22, P<0.00001), as well as a longer time of one leg stance with eyes closing (WMD= 1.66,95% CI 0.86-2.46, P<0.0001); and the exercise training increased the scores of Berg balance scale (WMD= 1.34,95%CI0.93-1.75, . P<0.00001) and shortened the time of up and go tests (WMD=-1.37, 95%CI -1.69--1.05,P<0.00001). Conclusion
Exercise training can obviously improve the static and dynamic balance function of the elderly with DPN; more atention should be paid to exercise training in clinic so as to improve the balance function of the elderly and decrease the risk of fllig.
[KEYWORDS] diabetes; peripheral neuropathy; exercise training; balance function;Meta analysis
- 星期一, 16 10月 2023
针灸应用于糖尿病周围神经病变的Meta分析及治疗策略
续畅1
吴汀溪1
宋婧1
杜鑫2
李彬2
黄凤:·
1.首都医科大学附属北京友谊医院药学部,北京100050;2.首都医科大学附属北京中医医院疮疡科,北京100010 【摘要】目的采用Meta分析方法系统评价针灸治疗糖尿病周围神经病变的临床疗效。方法通过检索cNKI、万方、VIP、cBM及PubMed数据库,收集针灸治疗糖尿病周围神经病变的随机对照试验.采用RevMan 5.3软件进行Meta分析。结果共纳入文献7篇,患者累计546例。Meta分析结果显示,针灸可显著的提高糖尿病周围神经病变患者正中神经、胫神经的运动及感觉神经的传导速度。结论针灸治疗糖尿病周围神经病变的疗效确切。
【关键词]针灸;糖尿病周围神经病变;随机对照试验;Meta分析;治疗策略
【中图分类号】R246
【文献标识码】B
【文章编号】1673—9701(2016)22—0074—04
Meta- analysis and treatment strategy of acupuncture in the treatment of diabetic peripheral neuropathy
XU Chang' WU Tingxil SONG Jing' DU Xin2 LI Bin2 HUANG Feng?
1.Department of Pharmaceutical, Beijing Friendship Hospital Affiliated to Capital Medical University, Beijing
100050,China;
2.Department of Speciality of Carbuncle and Ulcers, Bejjing Hospital of Traditional Chinese Medicine Affliated to Capital Medical University, Beijing
100010, China
[Abstract] Objective To evaluate the efficacy of acupuncture in the treatment of diabetic peripheral neuropathy (DPN) by Meta -analysis.
Methods Retrieved from CNKI, Wan -Fang, VIP, CBM, PubMed database, observational studies about acupuncture in the treatment of DPN were included. A Meta -analysis was conducted by using the software of RevMan 5.3.
Results 7 literatures were included and 546 cases were involved. The results of Meta -analysis showed that the acupuncture significantly improved the sensory nerve conduction velocity (SCV) and the motor nerve conduction velocity (MCV) of the median nerve and tibial nerve in patients with DPN.
Conclusion The acupuncture on diabetic peripheral neuropathy has an exact effect.
[Key words] Acupuncture; Diabetic peripheral neuropathy(DPN); Randomized controlled trial; Meta- -analysis; Treatment strategy
- 星期五, 13 10月 2023
A 'QUICK GUIDE ' TO PRESSURE INJURY MANAGEMENT
Published by
Wounds International
A division of Omniamed Communications Ltd
108 Cannon Street
London EC4N 6EU, UK
Tel: +44 (0)20 3735 8244
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
www.woundsinternational.com
© Wounds International, 2023
Suggested citation
Barakat-Johnson M, Ryan H, Brooks M et al (2023) A ‘Quick Guide’ to Pressure Injury Management. Wounds International
All rights reserved ©2023. No reproduction, copy or transmission of this publication may be made without written permission.
No part of this publication may be reproduced, copied or transmitted save with written permission or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any license permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London, W1P 0LP
This document was supported by Mölnlycke Health Care.
The views expressed in this publication are those of the authors and do not necessarily reflect those of Mölnlycke Health Care. All products mentioned in this publication should be used in accordance with the instructions for use and product information supplied with them.
The Australian Pressure Injury Treatment Advisory (PITA) Group was established in June 2021. The advisory group was founded in collaboration with Mölnlycke Health Care and comprises a group of expert clinicians in the field of wound care, including wound care leads and Professors of Nursing, with expertise in pressure injury prevention and treatment. The full list of members of the Australian PITA group is provided below.
Dr Michelle Barakat-Johnson, PhD, MN, RN, Clinical Lead and Nurse Manager Skin Integrity, HAC Pressure Injury Coordinator, Sydney Local Health District; Associate Professor, Faculty of Medicine and Health, University of Sydney; Visiting Research Fellow, School of Human and Health Sciences, University of Huddersfield, UK
Hayley Ryan, PhD(c), MBA, RN, PGCert WM, AICGG, Cert IV TAA; Director, WoundRescue Australia and New Zealand; Chair, Wounds Australia; Adjunct Fellow, University of Technology Sydney; Clinical Nurse Consultant Wound Management
Melinda Brooks, BN, MN, Grad Dip Nrs MACN, RN, Nurse Practitioner, Wound Management; Wound Wise Consulting and Education, Melbourne, Australia
Prof Keryln Carville, PhD, FWA, RN, Professor Primary Healthcare and Community Nursing, Silver Chain Group and Curtin University, Perth, Australia
Kerrie Coleman, PhD(c) MN Clinical (Wound), MNP (Chronic Disease), BNsc, DipApSc, Nurse Practitioner, Skin Integrity Services, Royal Brisbane and Women’s Hospital, Australia
Prof Fiona Coyer, PhD, Professor of Nursing, RN, Discipline Lead, Nursing School of Nursing, Midwifery and Social Work, The University of Queensland; Adjunct Professor, School of Nursing, Queensland University of Technology; Visiting Professor, Institute for Skin Integrity and Infection Prevention, University of Huddersfield, UK
Ann Marie Dunk, PhD(c), BHthSc (Nurs), MN (Research), RN, Clinical Nurse Consultant, Tissue Viability, Canberra Hospital, Australia; Skin Integrity Research Group (SKINT) University Centre for Nursing and Midwifery, Department of Public Health and Primary Care, Ghent University, Ghent, Belgium; Synergy: Nursing and Midwifery Research Centre, University of Canberra, ACT Health, Canberra, Australia
Dr Michelle Gibb, PhD, M Nsg Sci (NP), M Wound Care, BN, CF, Nurse Practitioner, Wound Management; Founder, Director, Wound Specialist Services (Primary Health Care and Aged Care), Brisbane, Australia
Catherine Leahy, Grad Cert STN, Grad Cert ACN, RN, Clinical Nurse Consultant, Wound Prevention and Management, Western New South Wales Local Health District, Australia
Wendy Palm, BN, RN, Manager of Clinical Systems, Resthaven Incorporated, South Australia
Tabatha Rando, MNP, Grad Dip CHN, Grad Cert STN, Dip FLM, Cert IV WAT, Cert WM, RN, Nurse Practitioner, Advance Nurse Consultant, Plastics/Wound Management, Department of Plastic and Reconstructive Surgery, Royal Adelaide Hospital, South Australia
Sarah Sage, BN, RN; MANP, Nurse Practitioner, Cert IV TAA; Dip. Business; GradCert Wound Care; GradCert Health Economics & Economic Evaluation, Coordinator Chronic Wound Service/Wound CNC team, Royal Melbourne Hospital, Melbourne, Australia
Corresponding author
Dr Michelle Barakat-Johnson, Clinical Lead and Nurse Manager Skin Integrity, HAC Pressure Injury Coordinator, Sydney Local Health District; Associate Professor, Faculty of Medicine and Health, University of Sydney; Visiting Research Fellow, School of Human and Health Sciences, University of Huddersfield, UK
Acknowledgements
Medical writers and editors: Sara Rook, Mölnlycke Health Care; Carys Ampofo, independent medical writer.
Project manager: Phil Morrisey, Mölnlycke Health Care. All authors of this work have consulted for Mölnlycke Health Care.
1. FOREWORD
Pressure injuries, also referred to as pressure ulcers, pressure sores, bedsores or decubitus ulcers (Wound, Ostomy and Continence Nurses Society; WOCN, 2017), are a common and preventable health problem. They impose significant health and economic burdens on patients, caregivers and healthcare systems. For the patient, pressure injuries can have a major impact on quality of life and mortality, with personal burdens ranging from pain and discomfort to psychosocial sequelae including stress, anxiety and depression, as well as declines in autonomy, security, spiritual wellbeing and social functioning (Gorecki et al, 2012; WOCN, 2017; European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP) and Pan Pacific Pressure Injury Alliance (PPPIA), 2019a).
Evidence-based pressure injury management can prevent infection, facilitate optimal wound healing, minimise scarring and prevent serious consequences such as morbidity and mortality. Achieving success in pressure injury management requires skill and knowledge. However, a significant challenge faced by clinicians is wound management, which is complicated by the diverse clinical effects and cost efficiency of various treatment methods and preventive approaches for these types of wounds.
In recognition of clinicians’ need for guidance on pressure injury management in Australia, an advisory group of national experts was formed in June 2021. The aim of the group was to develop a simplified clinical decision guide for the assessment and management of pressure injuries that should be used in daily practice alongside existing international guidelines. The advisory group comprised 12 members all with broad and specialised experience in clinical practice and research pertaining to pressure injury prevention and management. The group was named PITA (Australian Pressure Injury Treatment Advisory) group and convened four times, during which a consensus was achieved on the contents of a ‘Quick Guide’ to Pressure Injury Management.
Recognising the importance of aligning with established guidelines, the PITA group ensured that their scope extended beyond treatment alone and therefore actively incorporated assessment and prevention into their agenda and discussions. The PITA ‘Quick Guide’ to Pressure Injury Management follows current clinical evidence, best practice guidelines and implementation documents regarding the treatment of pressure injuries. It supports the current international guideline by providing a practical ‘how to’ guide for clinicians. The intent of this new guide is to provide a simplified and up-to-date resource that is quick and easy-to-use in the assessment and management of pressure injuries. This ‘Quick Guide’ is targeted at all clinicians responsible for the management of pressure injuries.
It is important to note that the recommendations in this ‘Quick Guide’ may not be suitable for use in all circumstances. The Australian PITA group developed this ‘Quick Guide’ based on evidence-based clinical recommendations, but any healthcare professional using it should also refer to the most recent international guidelines and conduct a holistic assessment of the person with a wound.
2. INTRODUCTION
Pathogenesis of pressure injuries
A pressure injury is defined as an area of localised injury or damage to the skin and/or underlying soft tissue that typically occurs over a bony prominence, resulting from pressure or pressure in combination with shear and/or friction (EPUAP/NPIAP/PPPIA, 2019a). Pressure injuries lead to tissue and cell deformation as well as ischemia, lymphatic flow blockage and reperfusion damage (Santamaria et al, 2018; EPUAP/NPIAP/PPPIA, 2019a; Wilson et al, 2019; Gefen et al, 2022). The severity of these injuries is proportional to the magnitude and duration of deformation, and in some cases, they can occur very rapidly (Gefen et al, 2022).
A pressure injury may also be related to the use of a device, in which case it is referred to as a devicerelated pressure injury (DRPI; Gefen et al, 2022).
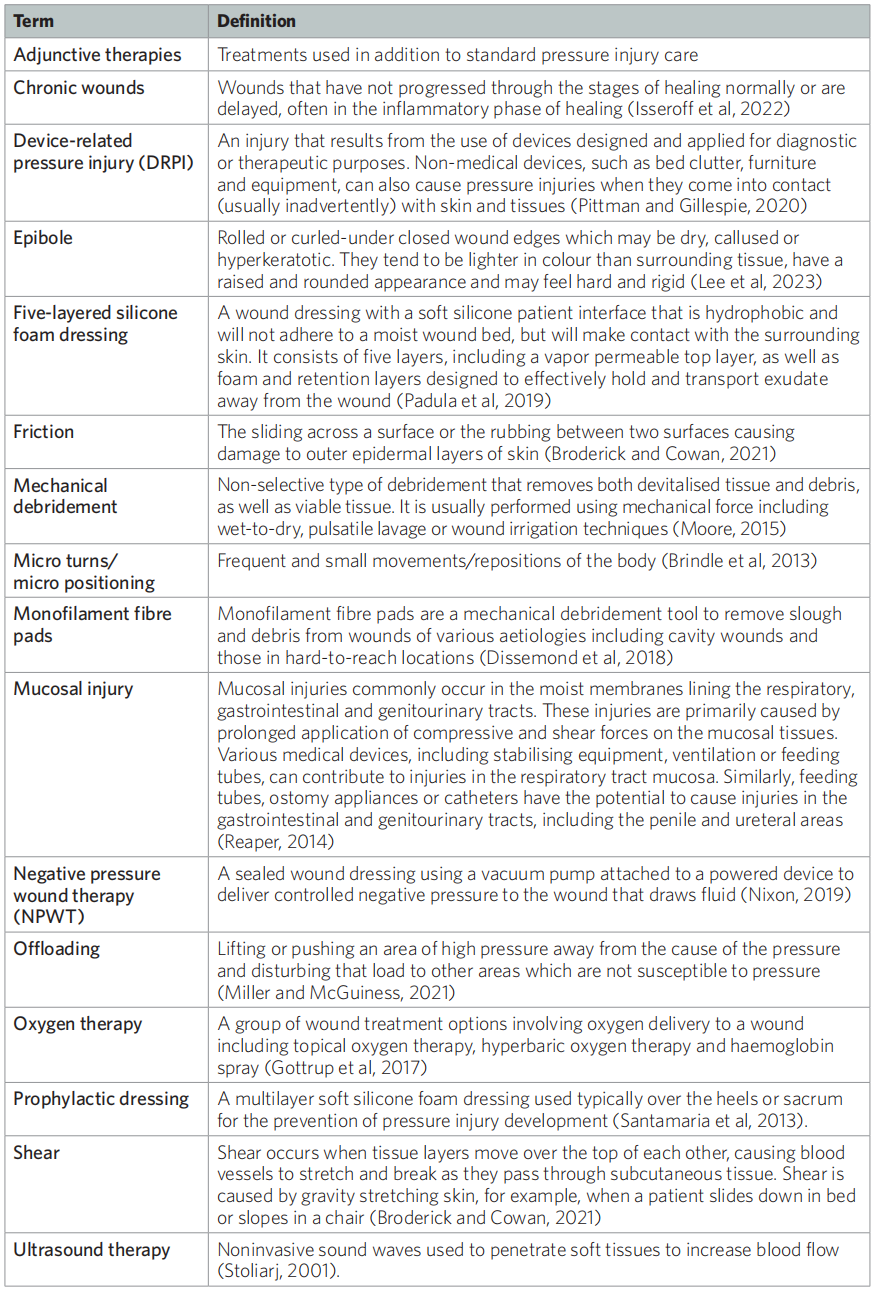
Terminology
As highlighted by the 2019 international guideline on pressure injury/ulcer prevention and treatment (EPUAP/ NPIAP/PPPIA, 2019a), there is ongoing discussion around pressure injury terminology. The original term, ‘gangraena per decubitum’ meaning ‘dead tissue due to lying down’ was coined by Wohlleben in 1777. The associated term ‘decubitus’ was first used to describe wounds related to bed rest. Later in the 19th century, the term ‘bedsore’ was commonly used, followed by ‘pressure sore’ and ‘pressure ulcer’ in the 1980s and 1990s, respectively. While these terms are still commonly used, they do not accurately reflect the aetiology of the injury. The words ‘sore’ and ‘ulcer’ imply an open wound at the skin surface (EPUAP/ NPIAP/PPPIA, 2019a), whereas the NPIAP pressure injury system, the most widely accepted pressure injury classification system, defines a Stage I pressure injury as ‘non-blanchable erythema of intact skin' (Edsberg et al, 2016).
The term 'pressure ulcer' is still widely used in Europe, while 'pressure injury' is now widely adopted in South-East Asia, Australia and New Zealand, with the United States of America following suit (EPUAP/ NPIAP/PPPIA, 2019a). In this 'Quick Guide', the term 'pressure injury' will be used throughout.
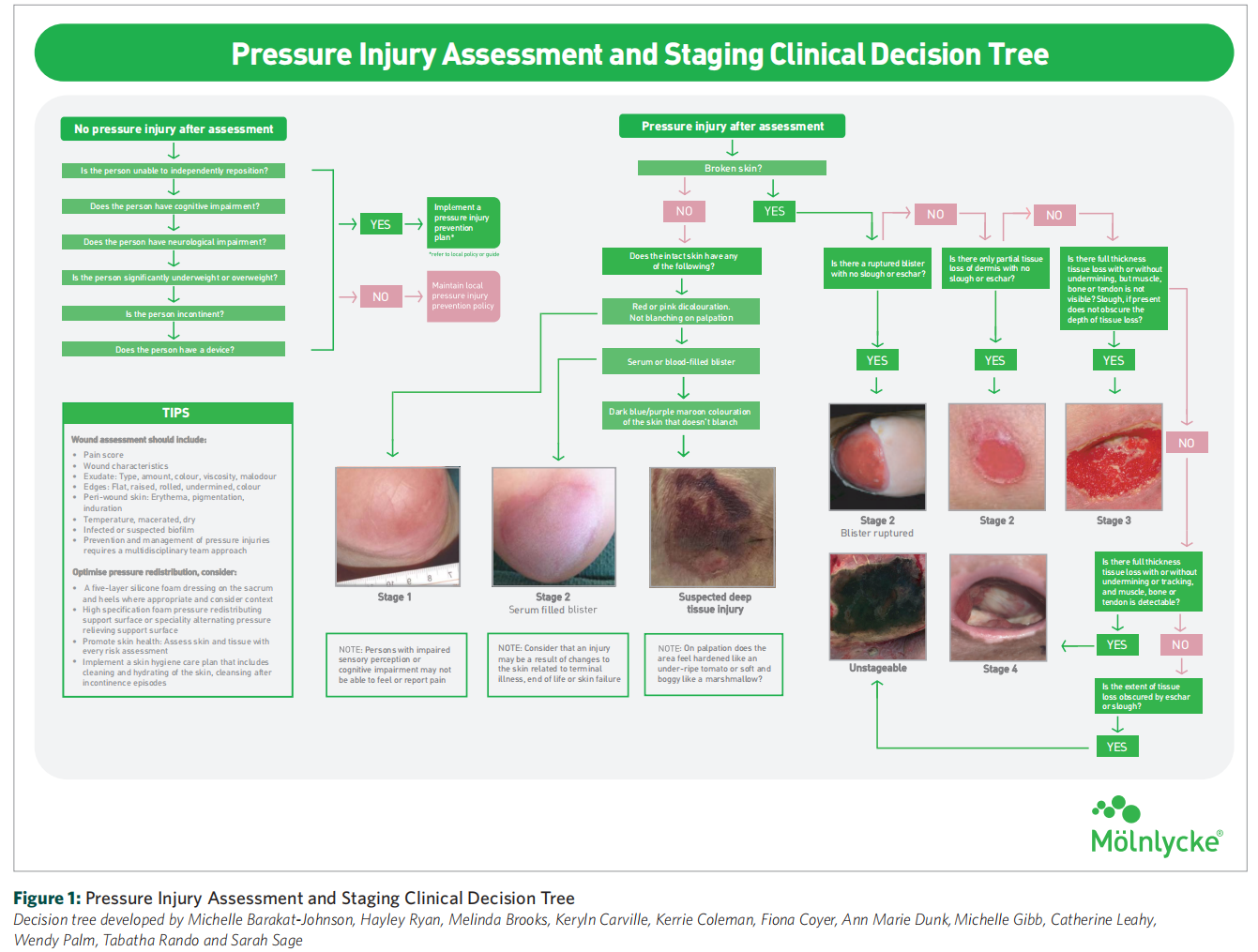
Pressure injury stages
Staging systems are used to classify and describe pressure injuries according to the extent of tissue loss and physical appearance of the injury (Edsberg et al, 2016). While all pressure injuries are serious, their severity can vary in terms of clinical impact and treatment difficulty, ranging from patches of discoloured skin that may heal to deep open ulcers that expose the underlying bone or muscle, which may be very challenging to treat (EPUAP/NPIAP/PPPIA, 2019a).
Pressure injury classification is based on the visual and palpatory identification of various tissue layers, including skin, subcutaneous fat, bone, muscle, tendon and ligament (EPUAP/NPIAP/PPPIA, 2019a). Pressure injuries are categorised into four stages (Stages 1–4), with higher stages indicating more tissue damage and associated economic costs. There are also two additional stages, namely unstageable pressure injury (covered in eschar or slough) and suspected deep tissue injury (Edsberg et al, 2016).
Dark skin tones
It is acknowledged that identifying early changes in skin colour which may indicate a Stage 1 pressure injury or deep tissue injury can be difficult in individuals with dark skin tones (Black and Simende, 2020). These groups are at a higher risk of developing pressure injuries and have been reported to have higher rates of full-thickness pressure injuries and increased mortality associated with these wounds (Bauer et al, 2016). Additionally, there is a frequent use of light skin tone examples in teaching and learning about pressure injuries in undergraduate and postgraduate nurse education (Gunowa et al, 2021). Due to these factors, the PITA group recommends giving additional consideration in the assessment of skin in individuals with dark skin tones.
Impact on the individual
Complications of pressure injuries can be serious and have a negative impact on individuals, their families and healthcare services. These impacts include loss of mobility, independence, privacy, dignity and ability to engage in preferred activities (Jackson et al, 2018), as well as severe pain, increased risk of infection (Edsberg et al, 2016) and delayed wound healing.
Prevention
Pressure injury prevention is the most important step in the prevention and management of these difficult to-treat wounds, with the initial stage involving an assessment of the individual's risk status (Boyko et al, 2018; Al Aboud and Manna, 2022). Prevention of pressure injuries involves alleviating risk factors for the individual and minimising episodes of prolonged pressure. This can be achieved by placing pressure redistributing or off-loading devices/dressings at pressure points or by frequently repositioning the patient (Boyko et al, 2018). When developing an individual care plan, it is crucial to consider additional preventative measures, including implementing skincare and hygiene regimens, continence management, using appropriate bed linen to minimise the shear effect, prophylactic dressings, mobilisation support surfaces, as well as optimising nutrition and hydration (EPUAP/NPIAP/PPPIA, 2019a). These preventative measures should be carefully considered and implemented based on each patient's assessment outcomes.
Treatment
When a pressure injury occurs, treatment is critical to promote healing and minimise the risk of complications (Qaseem et al, 2015). While the impact of a pressure injury might exhibit similarities across individuals, the primary concerns will vary from person to person. Hence, addressing these concerns will require involvement of the multidisciplinary team for a holistic care approach (Jackson et al, 2018). As defined by Qaseem et al (2015), a multidisciplinary approach involves nurses, physicians, dietitians, allied health and other members of a care team. Further, this care may be provided in a wide range of settings, including in the community, hospital or residential care and by a variety of healthcare providers (Qaseem et al, 2015; EPUAP/NPIAP/PPPIA, 2019a).
The goal of all treatment options is to minimise the pressure exerted on the wound and reduce moisture while maintaining an aseptic or least septic environment as possible (Zaidi and Sharma, 2022). The choice of treatment options should be according to the stage of the injury and the intended purpose of treatment, such as reducing moisture, removing necrotic tissue and/or controlling bacteraemia (Zaidi and Sharma, 2022). Treatment interventions may include managing underlying risk factors, using support surfaces, providing nutritional support, implementing specific wound care regimens and adjunctive therapies, and, if necessary, performing surgical repair (National Institute for Health and Care Excellence, 2014; Qaseem et al, 2015).
Superficial pressure injuries are typically expected to show signs of healing within two weeks, however, there are cases where this may not occur and the wound may deteriorate (NPIAP/EPUAP/PPPIA, 2014; Westby et al, 2017; EPUAP/NPIAP/PPPIA, 2019a). According to the 2019 international guideline (EPUAP/NPIAP/PPPIA, 2019a), if a pressure injury does not show any signs of healing within two weeks despite appropriate local wound care, pressure distribution and nutrition, a comprehensive reassessment of the individual should be conducted.
There are many treatment options available, including wound dressings and topical agents such as ointments, creams and gels (Westby et al, 2017). However, evidence supporting the effectiveness of specific dressings and topical agents in aiding the healing of pressure injuries is limited (Westby et al, 2017). According to the 2019 international guideline (EPUAP/NPIAP/PPPIA, 2019a), adjunctive therapies may be considered in cases where wounds are not progressing adequately or where chronic osteomyelitis is present (Boyko et al, 2018). Examples of adjunctive therapies include electrotherapy, ultrasound therapy, negative pressure wound therapy (NPWT), oxygen therapy or surgical repair of the wound.
Moreover, many novice clinicians find pressure injury prevention, assessment and treatment interventions confusing and overwhelming due to the plethora of products available (Barakat-Johnson et al, 2019a; Li et al, 2022). Approaches to pressure injury treatment are dependent on the expertise of the individual, with novice clinicians relying on experts to review the wound and provide guidance on wound management (Welsh, 2018). Additionally, access and equity to these products across all clinical settings is highly variable and further complicates decision-making.
Wounds that are not progressing adequately require clinicians to have a thorough understanding of evidence-based interventions and access to resources to avoid further deterioration. The PITA group acknowledges the importance of assessment and prevention as part of pressure injury management; however, there is a lack of clear and useful guidance focusing on pressure injury treatment. Clinicians may also find existing guidelines difficult to use, or with a lack of clear visual aids (Qaseem et al, 2015; Tachibana et al, 2016; WOCN, 2017; Atkin et al, 2019; EPUAP/NPIAP/PPPIA, 2019a; EPUAP/NPIAP/ PPPIA, 2019b; Gefen et al, 2020; Kirman, 2020).
3. PREVENTION AND TREATMENT OF PRESSURE INJURIES: 2019 INTERNATIONAL CLINICAL PRACTICE GUIDELINE
In 2019, the EPUAP, NPIAP and PPPIA published the third edition of the Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The international guideline presents a comprehensive review and evaluation of the best available evidence (at the time of the literature search), followed by 114 recommendations and 62 best practice statements to guide practitioners in risk assessment, diagnosis, prevention and treatment of pressure injuries.
Furthermore, the guideline considers the specific needs of different population groups and emphasises the importance of considering the patient's perspective. It provides recommendations for supporting and involving patients in their care, as well as 20 quality indicators aimed at monitoring the implementation of the international guideline recommendations (EPUAP/NPIAP/PPPIA, 2019a).
One concise publication that summaries the content of the full international guideline (EPUAP/NPIAP/ PPPIA, 2019a) is the Prevention and Treatment of Pressure Ulcers/Injuries: Quick Reference Guide (EPUAP/ NPIAP/PPPIA, 2019b).
4. FURTHER CONSIDERATIONS IN DEVELOPING THE PITA 'QUICK GUIDE'
Risk factors for pressure injury
The risk factors associated with pressure injury development should be carefully considered. Identifying individuals who are at risk of developing pressure injuries through risk screening is a central component of clinical practice (EPUAP/NPIAP/PPPIA, 2019a). It is important to note that an individual's risk of pressure injury may change with alterations in their health status and these changes can occur over time. Therefore, it is important to screen patients upon admission, assess their risk when identified and regularly monitor them, especially when there is a change in their health status (EPUAP/NPIAP/ PPPIA, 2019a). Another significant component in pressure injury prevention, classification, diagnosis and treatment is the assessment of the skin and soft tissues (EPUAP/NPIAP/PPPIA, 2019a). Clinicians use visual inspection and tactile examination to assess the individual's skin appearance, integrity and underlying tissue health. This assessment is not limited to the site of the injury alone; it extends to surrounding areas which might also exhibit early signs of damage.
For patients identified as being at risk of developing pressure injuries or those already experiencing pressure injuries, evidence-based guidelines should be used to ensure that appropriate preventative and treatment interventions are implemented (WOCN, 2017).
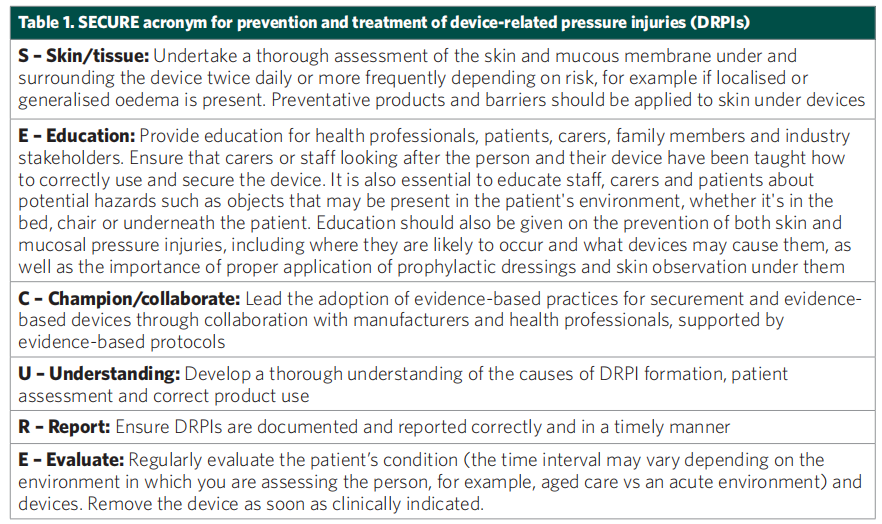
Device-related pressure injury
Devices can include a wide range of items, such as oxygen tubing, endotracheal tubes, bite blocks, orogastric and nasogastric tubes, urinary catheters and faecal containment devices. Device-related pressure injuries (DRPIs) can occur either on the skin or mucous membrane (Gefen et al, 2022). However, pressure injury classification systems are designed for injuries on the skin and are not applicable to the mucous membrane, as the mucosa is anatomically different. Instead, pressure injuries on the mucous membrane are not staged but documented as mucosal pressure injuries.
According to the 2019 international guideline (EPUAP/NPIAP/PPPIA, 2019a), all patients with a device should be considered at risk for DRPIs. It is recommended to inspect the surrounding skin and skin beneath any device at least twice a day, and more frequently if the patient is at high–risk. Additionally, any potential device-related sources of pressure should be removed as soon as medically possible (Galetto et al, 2021). The overall treatment goals for DRPIs occurring on the skin are similar to those for pressure injuries that result from pressure, shear and/or friction.
Critically ill individuals admitted to intensive care are particularly vulnerable to pressure injuries (Lovegrove et al, 2020) due to their limited mobility, compromised cognition and reduced sensation often caused by sedation and the presence of multiple medical devices.
A modified Delphi study (Lovegrove et al, 2020) was conducted to determine the essential preventative interventions for pressure injuries in critically ill patients based on their risk levels, yielding several recommendations. As per the study, all patients should undergo a risk screening within two hours of admission and receive regular risk screening every eight hours. Patients identified as moderate– to high–risk should be provided with an appropriate mattress support surface based on their risk screening, as well as a device to offload pressure from the heels. High–risk patients should also receive nutritional supplements if able to eat orally or parenteral nutritional support if unable to do so. Furthermore, the study suggests using five-layered silicone foam dressings for sacral, heel and trochanteric areas, an active mattress support surface and a pressure-distributing cushion for sitting. The Delphi panel also agreed that repositioning should be performed at least every four hours for low–risk patients and every two hours for moderate– and high–risk patients, irrespective of the mattress device or the use of slide sheets and other resources (Lovegrove et al, 2020).
The SECURE acronym for the prevention and treatment of DRPIs (Gefen et al, 2022) is an excellent tool to help guide a clinician’s assessment and prevention plan [Table 1].
Cost
While directly comparing health economic data across different geographic locations can be challenging, pressure injuries present a substantial financial burden on healthcare systems. They are associated with increased length of hospital stay, readmissions and high financial costs of care (Chaboyer et al, 2016; EPUAP/NPIAP/PPPIA, 2019a).
Pressure Injuries pose a significant cost to the health system (Graves and Zheng, 2014a, 2014b; Norman et al, 2016). In a recent study on costings in Australia, the cost of pressure injuries amounted to AUS$9.11 billion annually with extended hospital stays accounting for AUS$3.60 billion and treatments costing AUS$3.59 billion (Nghiem et al, 2022).
In the US, the cost of a hospital-acquired pressure injury (HAPI) is approximately US$10,708 per person, resulting in a total that exceeds approximately US$26.8 billion (Padula and Delarmente, 2019).
Person-centred care
Within the field of wound care, there is an increasing emphasis on engaging patients in their care. The terms ‘person-centred’ and ‘patient-centred’ are often used interchangeably and have gained significant attention in recent years, supported by emerging evidence in the field of wound management (Gethin et al, 2020). This approach aims to facilitate the implementation of care practices and strategies that are important for patient safety, which may be less effective without full patient engagement (McInnes et al, 2014). It is thought that when patients are actively engaged and involved in their care, the delivery of pressure injury prevention regimens can potentially reduce financial and physical burdens, ultimately improving patient outcomes (McInnes et al, 2014).
This shift towards person-centred care is driven, in part, by the growing public interest in understanding diseases, symptoms and treatment options. With the aid of social media, patient networks and new technologies, individuals are now seeking more information about their own health conditions or those of their family members (Gethin et al, 2020). As highlighted by Gethin et al (2020), this growing interest and engagement in person-centred care has allowed healthcare providers to tap into patients' knowledge and expertise, which is arguably an underutilised resource in care settings. Numerous organisations have embraced this care approach and policy reforms and approaches have been implemented to support person-centred care and integrated health services (Whitty et al, 2017; Gethin et al, 2020).
Person-centred care includes patients as partners in their own care, with a focus on keeping the patient’s individual needs remaining at the centre of the decision-making process (Gethin et al, 2020). Importantly, according to the person-centred care concept, a patient should not be defined by their health condition; and their plans, beliefs, strengths and personality should be carefully considered (Gethin et al, 2020).
From a nursing perspective, person-centred care is a multi-dimensional concept and includes promoting patient participation and autonomy, shared decision-making, shared power, knowledge sharing, caring attitudes and individualising patient care (Lusk and Fater, 2013; Latimer et al, 2014; Gethin et al, 2020). Ultimately, person-centred care aims to establish respectful and collaborative partnerships between healthcare professionals and patients (Latimer et al, 2014).
There are several factors that may hinder patient involvement in patient safety and care. According to McInnes et al (2014), successful patient participation in pressure injury prevention requires ongoing education throughout their admission, effective pain and discomfort management and the establishment of a supportive and collaborative relationship with healthcare staff working in partnership with the patients. Engaging patients in their care can be a complex task, particularly for those with chronic wounds, as it often signifies a wider systemic disease that necessitates an interdisciplinary approach involving several healthcare professionals and services (Norman et al, 2016). This complexity can increase the risk of communication issues and possible treatment failures at various points along the patient's care journey (Lindsay et al, 2017). Moreover, the treatment process for patients with chronic wounds may be made increasingly difficult due to limitations and inconsistencies in patient health literacy, leading to uncertainty about what to expect during their care journey (Lindsay et al, 2017).
Lindsay et al (2017) additionally highlight the core concept of person-centred care and how its application necessitates a holistic approach that considers the individual as a whole, beyond just their wound. Person-centred care is based on individualised care and involves a collaborative approach in which patients are encouraged to be equal partners and healthcare professionals can learn from the patient's experiences (Lindsay et al, 2017). Central to this concept is effective communication, language and terminology, education and patient advocacy (Lindsay et al, 2017).
Latimer et al (2014) investigated patient preferences for involvement in pressure injury prevention, highlighting the complexities and barriers associated with patient involvement. Patient involvement cannot be assumed, as it can range from non-participation to active participation. It is important to recognise that not all patients are able or willing to actively participate in their care; as some patients may prefer or require a more passive role (Latimer et al, 2014). This further highlights the importance of individualising care on a patient-by-patient basis.
Crucially, in order to form effective partnerships, the patient's role must first be clearly defined. Additionally, it is important to identify barriers and challenges to implementing these partnerships and develop strategies, including educational tools, to overcome them (Latimer et al, 2014). A willingness and understanding of how to actively participate, from both the perspectives of the patient and healthcare workers, effective leadership and a cultural shift to reorganise healthcare processes are all fundamental elements of person-centred care (Gethin et al, 2020).
Implementation of care bundles in pressure injury prevention and management
Multicomponent and person-centred care bundles are increasingly recognised as important strategies in pressure injury prevention, with research demonstrating their role and value in nursing care (Chaboyer et al, 2016; Whitty et al, 2017).
Several studies have also highlighted the need for careful consideration in implementing pressure injury prevention and management strategies. Barakat-Johnson et al (2019a) explored the thoughts and experiences of hospital nurses involved in pressure injury prevention and management. They found that difficulties exist when it comes to delivering quality care due to competing priorities and challenges faced at both the organisational and patient levels. The study concluded that pressure injury prevention and management should not be viewed in isolation, as it is only one aspect of patient care. Hospitals must implement measures to support and enable nurses to deliver quality care in pressure injury prevention and management (Barakat-Johnson, 2019a).
Processes used to implement evidence-based practice play a significant role in influencing outcomes (Barakat-Johnson, 2019b). In 2016, Sving et al highlighted the need to increase knowledge about adequate implementation strategies related to pressure injury prevention. As such, they conducted a study to evaluate whether a multi-faceted, unit-tailored intervention using evidence-based pressure injury prevention affects the prevention and prevalence of pressure injury and the nurses’ knowledge and attitudes. The study used the Promoting Action on Research Implementation in Health Service (PARIHS) framework to identify key implementation areas and guide the planning and evaluation of the intervention (Harvey and Kitson, 2016). They found that statistically significantly more patients received pressure ulcer prevention care following the intervention (Sving et al, 2016).
A significant increase in HAPIs over a five-year period in one Australian health district was the catalyst for the use of the PARIHS framework. Barakat-Johnson et al (2019b) demonstrated the importance of the framework in understanding the translation of evidence in a complex health system and how it helped in mapping elements that could potentially influence implementation outcomes.
Tayyib and Coyer (2016) reported on the successful implementation process used to integrate a pressure injury prevention care bundle approach for improving patients' skin integrity in intensive care. The care bundle demonstrated a significant reduction in pressure injury incidence, using the Ottawa model of research use as a consolidated framework for implementing bundled evidence into daily clinical nursing practice (Tayyib and Coyer, 2016).
Barakat-Johnson et al (2019c) also highlighted how patient care planning should incorporate the timely implementation of evidence-based strategies in terms of lowering rates of HAPIs and associated skin conditions. In a study conducted in an Australian local health district, the costs of HAPIs were determined and compared with the costs and outcomes of a program implemented to reduce HAPI incidence. The study found that HAPI intervention-based program resulted in a reduction in HAPI incidence and prevalence within the local health district. Furthermore, the program and its implementation helped reduce costs associated with HAPIs compared to the previous approach to preventing HAPIs in one local health district (Barakat-Johnson et al, 2019c).
5. PRESSURE INJURY PREVENTION, ASSESSMENT AND STAGING (CLINICAL DECISION TREE)
To aid clinicians in the prevention, staging, assessment and determination of care goals for individuals with pressure injuries, the PITA group developed a Clinical Decision Tree [Figure 1, page 11]. This tool will help clinicians create the most appropriate treatment plan and ensure that pressure injuries are appropriately evaluated, reported and documented, taking into account local guidelines and policies.
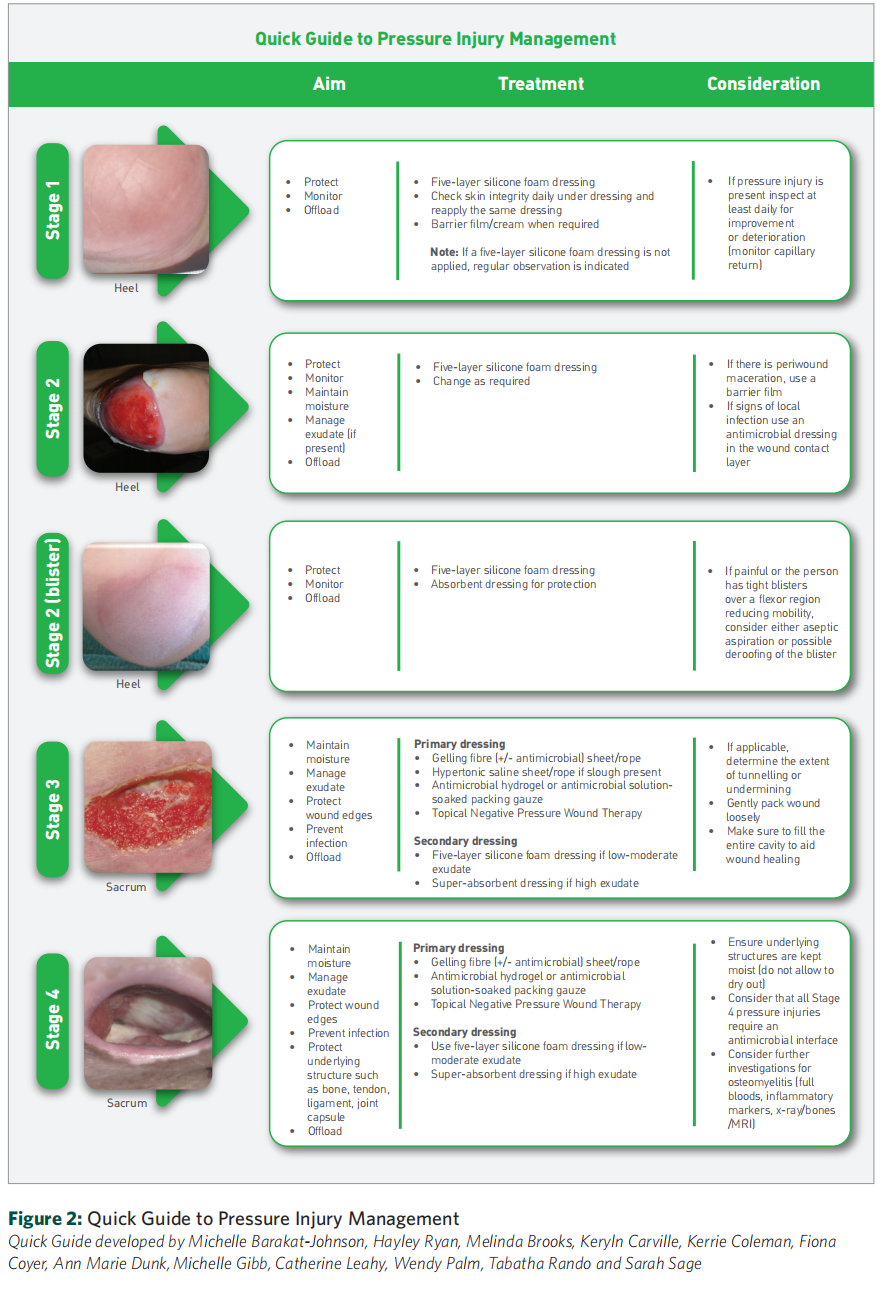
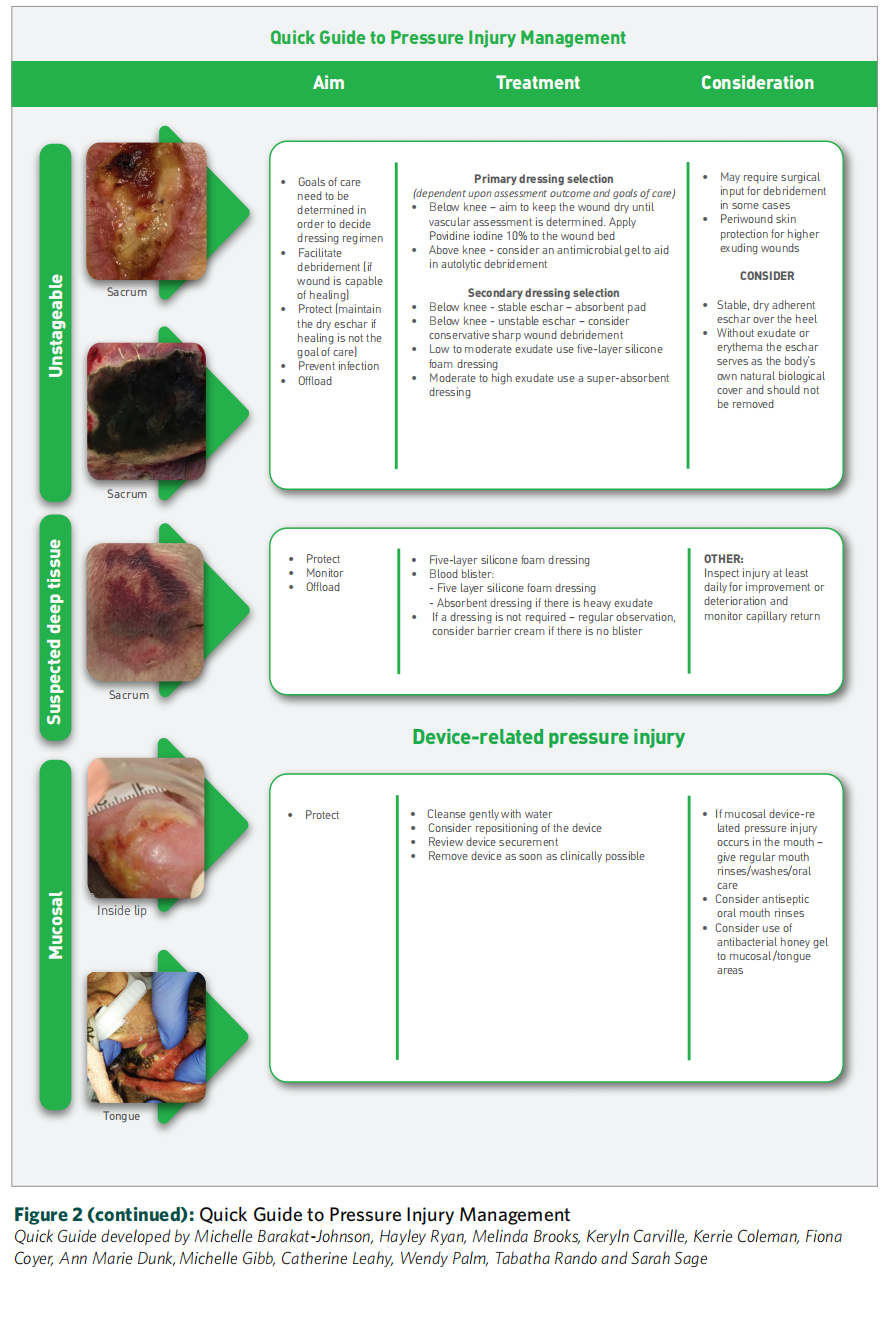
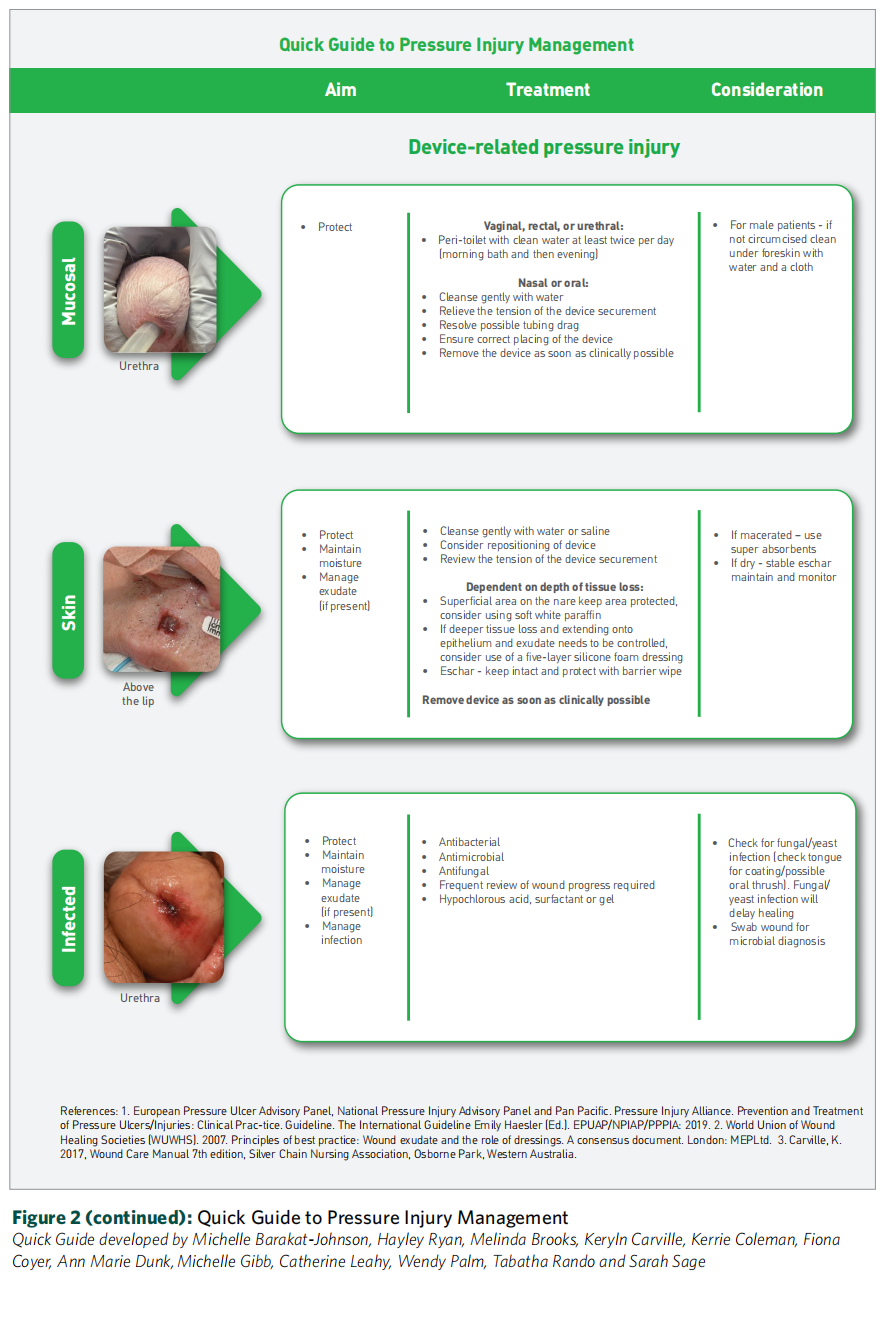
6. QUICK GUIDE TO PRESSURE INJURY MANAGEMENT
The 'Quick Guide to Pressure Injury Management' tool [Figure 2, pages 12–14] aims to support clinicians in formulating the most suitable treatment plan. This guide, developed by the PITA group, takes into consideration treatment aims, patient-related factors, wound characteristics and recommended products. Prevention and management of pressure injuries necessitate a multidisciplinary team approach due to the wide-ranging impact of these injuries. To ensure optimal treatment, the following factors should be taken into consideration [Table 2, page 15].

REAL WORLD PRESSURE INJURY TREATMENT CASE STUDY
Patient presentation:
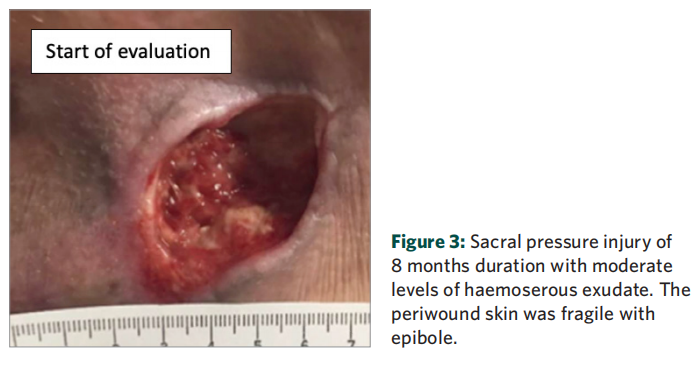
■ A 75-year-old female presented with a painful Stage 4 sacral pressure injury [Figure 3]
■ The patient had a medical history of cerebrovascular accident with left-sided weakness, atrial fibrillation, chronic obstructive pulmonary disease and gout
■ Experiencing poor mobility and unable to self-mobilise, the patient received care at home from her husband and was seen three times a week by community nurses.
Wound presentation
■ Wound measured 12cm2 and had been present for 8 months
■ Wound bed composed of unhealthy granulation tissue
■ No signs of wound infection on clinical assessment
■ Exudate levels were moderate and haemoserous in appearance
■ Periwound skin, despite being fragile and exhibiting epibole, was intact and healthy
■ At baseline, pain at dressing change was rated as 6/10 on a visual analogue scale (VAS; 1 = no pain, 10 = unbearable pain).
Treatment regimen
■ Wound was regularly monitored over a 7-week period
■ Guidance for a Stage 4 pressure injury was followed as per the 'Quick Guide to Pressure Injury Management' [Figure 2, pages 12–14]:
- Dressings were changed every third day
- At each dressing change, wound was mechanically debrided using monofilament fibre pads
- Wound was cleansed using a hypochlorous acid solution
- Wound cavity was loosely packed with gelling fibre dressing secured in place by a five-layer soft
silicone foam dressing
Treatment overview
During the 7-week treatment period, there was a steady reduction in both the area and depth of the wound and an improvement in the condition of the wound bed. Notably, no clinical signs of wound infection were observed throughout the entire treatment course.
After 4 weeks of treatment, the wound area and depth reduced by 50% to 1cm2 . Granulation tissue was observed in the wound bed, as shown in Figure 4. The level of exudate remained moderate with a serous appearance.
At the final evaluation after 7 weeks of treatment, the pressure injury had successfully healed [Figure 5] and fully reepithelialised, while the level of exudate reduced from moderate to none. The periwound skin maintained healthy and intact and the previously observed epibole had resolved.

During the 7-week treatment period, the patient experienced no pain, as the strategies outlined below, in line with recommendations in Table 2, were incorporated into the dressing change procedure.
Additional treatment considerations in line with Table 2 included:
Nutrition: Comprehensive nutrition assessment was conducted and the patient was placed on a high-protein diet to support optimal wound healing. Additionally, the patient was recommended a consultation with a nutritionist
Offloading: Offloading of the sacral wound was achieved using turning and positioning devices
Social: Active engagement of the patient's husband in the treatment plan was instrumental in facilitating care and offloading the wound, as well as providing support during showering and daily activities
Pain management: Patient was provided with specific instructions on positioning her body to minimise pressure on the wound site. Turning and positioning aids were also used to ensure comfort during sleep
Management plan: A well-defined plan was established, involving visits by the wound nurse every three days. Dressing changes were performed during these visits and the plan was continuously reviewed throughout the wound healing journey to ensure optimal progress
Skin health: A comprehensive skin hygiene plan was implemented, incorporating the use of moisturisers and barrier products
Continence: Patient did not experience any issues related to incontinence throughout the course of treatment.
Overall, following the Quick Guide to Pressure Injury Management [Figure 2] played a significant role in guiding the treatment and product selection process, ultimately leading to the successful healing of a pressure injury that was present for 8 months.
References
1. Al Aboud AM, Manna B (2022) Wound pressure injury management. Available at: https://www.ncbi.nlm.nih. gov/books/NBK532897/ (accessed 14.07.2023)
2. Atkin L, Bucko Z, Conde Montero E et al (2019) Implementing TIMERS: the race against hard-to-heal wounds. J Wound Care 23(3a): S1-S50
3. Barakat-Johnson M, Lai M, Wand T, White K (2019a) A qualitative study of the thoughts and experiences of hospital nurses providing pressure injury prevention and management. Collegian 26: 95-102
4. Barakat-Johnson M, Lai M, Wand T, Coyer F, White K (2019b) Systemwide practice change program to combat hospital-acquired pressure injuries. Translating knowledge into practice. J Nurs Care Qual 1-7
5. Barakat-Johnson M, Lai M, Wand T et al (2019c) Costs and consequences of an intervention-based program to reduce hospital-acquired pressure injuries in one health district in Australia. Aust Health Rev 43(5): 516-525
6. Bauer K, Rock K, Nazzal M et al (2016) Pressure ulcers in the United States’ inpatient population from 2008 to 2012: results of a retrospective nationwide study. Ostomy Wound Manage 62(11): 30–8
7. Black J and Simende A (2020) Ten top tips: assessing darkly pigmented skin. Wounds International 11(3): 8-11
8. Boyko TV, Longaker MT, Yang GP (2018) Review of the current management of pressure ulcers. Adv Wound Care (New Rochelle) 7(2): 57-67
9. Brindle CT, Malhotra R, O'rourke S et al (2013) Turning and repositioning the critically ill patient with hemodynamic instability: a literature review and consensus recommmendations. J Wound Ostomy Continence Nurs 40(3): 254-267
10. Broderick VV, Cowan LJ (2021) Pressure Injury Related to Friction and Shearing Forces in Older Adults. Journal of dermatology and skin science 3(2): 9-12
11. Chaboyer W, Bucknall T, Webster J, McInnes E (2016) The effect of a patient centred care bundle intervention on pressure ulcer incidence (INTACT): A cluster randomised trial. International Journal of Nursing Studies 64: 63-71
12. Dissemond J, Eberlein T, Bültemann A et al (2018) A purpose-designed monofilament-fibre pad for debridement of hard-to-reach wounds: experience in clinical practice. Wound care 27(7): 421-425
13. Edsberg LE, Black JM, Goldberg M et al (2016) Revised National Ulcer Advisory Panel Pressure Injury Staging System. J Wound Ostomy Continence Nurs 43(6): 585-597
14. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance (2019a) Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline
15. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance (2019b) Prevention and Treatment of Pressure Ulcers/Injuries: Quick Reference Guide
16. Galetto SGS, Nascimento ERP, Hermida PMV et al (2021) Medical device-related pressure injuries in critical patients: prevalence and associated factors. Rev Esc Enferm USP 55: e20200397
17. Gefen A, Alves P, Ciprandi G et al (2020) Device-related pressure ulcers: SECURE prevention. J Wound Care 29(2a): S1-S52
18. Gefen A, Alves P, Ciprandi G (2022) Device-related pressure ulcers: SECURE prevention. 2nd Edition. Journal Wound Care 31(3 Suppl 1): S1-S72
19. Gethin G, Probst S, Stryja J, Christiansen N et al (2020) Evidence for person-centred care in chronic wound care: A systematic review and recommendations for practice. J Wound Care 29(9b): S1-S22
20. Gorecki C, Nixon J, Madill A et al (2012) What influences the impact of pressure ulcers on health-related quality of life? A qualitative patient-focused exploration of contributory factors. J Tissue Viability 21(1): 3-12
21. Gottrup F, Dissemond J, Baines C et al (2017) Use of Oxygen Therapies in Wound Healing. Journal of Wound Care 26(5): S1-S43
22. Graves N, Zheng H (2014a) The prevalence and incidence of chronic wounds: a literature review. Wound Pract Res 22: 4-12, 4-9
23. Graves N, Zheng H (2014b) Modelling the direct health care costs of chronic wounds in Australia. Wound Pract Res 22: 20-24, 6-33
24. Gunowa NO, Hutchinson M, Brooke J et al (2021) Pressure injuries and skin tone diversity in undergraduate nurse education: Qualitative perspectives from a mixed methods study. Journal of Advanced Nursing 77(11): 4511-4524
25. Harvey G and Kitson A (2016) PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci 11: 33
26. Isseroff RR, Soulika AM, Romanelli M et al (2022) Chronic wounds. Nature Publishing Group 8(1): 50
27. Jackson DE, Durrant LA, Hutchinson M et al (2018) Living with multiple losses: Insights from patients living with pressure injury. Collegian 25(4): 409-414
28. Kirman CN (2020) Pressure injuries (pressure ulcers) and wound care guidelines. Available at: https://emedicine. medscape.com/article/190115-guidelines#showall
29. Latimer S, Chaboyer W, Gillespie B (2014) Patient participation in pressure injury prevention: giving patient’s a voice. Scandinavian Journal of Caring Sciences 28(4): 648-656
30. Lee PL, Loder SJ, Guerrero DT et al (2023) Use of wound edge inversion (epibole) to generate recalcitrant and inflamed diabetic wounds. Wound Repair and Regeneration 31(1): 120-127
31. Li J, Zhu C, Liu Y et al (2022) Critical Care Nurses’ Knowledge, Attitudes, and Practices Regarding Pressure Injury Treatment: A Nationwide Cross-Sectional Survey. Risk Manag Healthc Policy 15: 2125-2134
32. Lindsay E, Renyi R, Wilkie P et al (2017) Person-centred care: a call to action for wound management. Journal of Wound Care 26(11): 662-677
33. Lovegrove J, Fulbrook P, Miles S (2020) International consensus on pressure injury preventative interventions by risk level for critically ill patients: A modified Delphi study. Int Wound J 17(5): 1112-1127
34. Lusk JM and Fater K (2013) A concept analysis of personcentered care. Nursing Forum 48(2): 89-98
35. McInnes E, Chaboyer W, Murray E et al (2014) The role of patients in pressure injury prevention: a survey of acute care patients. BMC Nurs 13(1): 41
36. Miller B and McGuiness V (2021) Brief intermittent pressure off-loading on skin microclimate in healthy adults – A descriptive-correlational pilot study. Journal of Tissue Viability 30(3): 379-394
37. Moore Z (2015) Mechanical debridement: a brief overview. British Journal of Nursing 24(12): 38
38. National Institute for Health and Care Excellence (2014) Clinical guideline [CG179] Pressure ulcers: prevention and management. Available at: https://www.nice.org.uk/ guidance/cg179
39. National Pressure Injury Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance (2014). Prevention and Treatment of Pressure Ulcers: Quick Reference Guide.
40. Nghiem S, Campbell J, Walker RM et al (2022) Pressure injuries in Australian public hospitals: A cost of illness study. Int J Nurs Stud 130: 104191
41. Nixon R (2019) Negative pressure wound therapy in the management of wounds. Companion Animal 24 (7): 372-379
42. Norman RE, Gibb M, Dyer A et al (2016) Improved wound management at lower cost: A sensible goal for Australia. Int Wound J 13(3): 303-316
43. Padula WV, Chen YH, Santamaria N (2019) Five layer border dressings as part of a quality improvement bundle to prevent pressure injuries in US skilled nursing facilities and Australian nursing homes: A cost‐effectiveness analysis. International Wound Journal 16(6): 1263-1272
44. Padula WV, Delarmente BA (2019) The national cost of hospital-acquired pressure injuries in the United States. Int Wound J 16(3): 634-640
45. Pittman J and Gillespie C (2020) Medical Device-Related Pressure Injuries. Critical Care Nursing Clinics of North America 32(4): 533-542
46. Qaseem A, Humphrey LL, Forciea MA et al (2015) Treatment of pressure ulcers: A clinical practice guideline from the American College of Physicians. Ann Intern Med 162(5): 370-37
47. Reaper S (2014) A retrospective review of oral mucosal pressure injuries in mechanically ventilated patients. Australian Critical Care 27(1): 54-55
48. Santamaria N, Gerdtz M, Sage S et al (2013) A randomised controlled trial of the effectiveness of soft silicone multilayered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. International Wound Journal
49. Santamaria N, Gerdtz M, Kapp S et al (2018) A randomised controlled trial of the clinical effectiveness of multi‐layer silicone foam dressings in the prevention of pressure injuries in high‐risk aged care residents: the Border III Trial. Int Wound J 15(3): 482-490
50. Stoliarj A (2001) Ultrasound Treatment of Wounds in Microsurgical Wounded and Noncombat Patients. Prehospital and Disaster Medicine 16(2): 123-124
51. Sving E, Högman M, Mamhidir AG, Gunningberg L (2016) Getting evidence-based pressure ulcer prevention into practice: a multi-faceted unit-tailored intervention in a hospital setting. International Wound Journal 13(5): 645-654
52. Tachibana T, Imafuku S, Irisawa R et al (2016) The wound/ burn guidelines - 2: Guidelines for the diagnosis and treatment for pressure ulcers. J Dermatol 43(5): 469-506
53. Tayyib N, Coyer F (2016) Effectiveness of pressure ulcer prevention strategies for adult patients in intensive care units: a systematic review. Worldviews on Evidence-Based Nursing 13(6): 432-444
54. Welsh L (2018) Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. International Wound Journal 15(1): 53–61
55. Westby MJ, Dumville JC, Soares MO et al (2017) Dressings and topical agents for treating pressure ulcers. Cochrane Database Syst Rev 6(6): CD011947
56. Whitty JA, McInnes E, Bucknall T et al (2017) The cost-effectiveness of a patient centred pressure ulcer prevention care bundle: Findings from the INTACT cluster randomised trial. International Journal of Nursing Studies 75: 35-42
57. Wilson L, Kapp S, Santamaria N (2019) The direct cost of pressure injuries in an Australian residential aged care setting. Int Wound J 16: 64-70
58. Wound, Ostomy and Continence Nurses Society (2017) 2016 Guideline for Prevention and Management of Pressure Injuries (Ulcers). An Executive Summary. J Wound Ostomy Continence Nurs 44(3): 241-246
59. Zaidi SRH, Sharma S (2022) Pressure Ulcer. Available at: https://pubmed.ncbi.nlm.nih.gov/31971747/ (accessed 14.07.2023)
The decision to adopt any recommendation must be made by the qualified healthcare professional, taking into consideration available resources and the individual patient's circumstances.
The Australian PITA Group is unable to guarantee the reliability and accuracy of the individual studies referenced in this 'Quick Guide'.
Nothing in this 'Quick Guide' should be considered as medical advice for specific cases.
This 'Quick Guide' is intended for educational and informational purposes only. The information contained within was deemed accurate by the Australian PITA Group at the time of publication.
It is important to note that research, technology and clinical guidance are subject to rapid change, and the recommendations in this 'Quick Guide' may become inconsistent with future advances.
The healthcare professional is responsible for staying informed about research and technological advancements that may impact their clinical decision-making.
This 'Quick Guide' is not intended to endorse any specific product or solution; as such, generic names of products and solutions have been used throughout this 'Quick Guide'.
This 'Quick Guide' does not provide advice on reimbursement regulations.
This 'Quick Guide' is not intended to provide full safety and usage information for products, devices or solutions. Any product, device or solution mentioned should be used in accordance with the relevant manufacturer's instructions for use and any caution statements related to those products, devices or solutions should be observed (including any data related to adverse events).
The views expressed in this publication are those of the authors and do not necessarily reflect those of Mölnlycke Health Care.
AUSTRALIAN PITA GROUP MEETINGS
A group of skin integrity and pressure injury clinical and academic experts were approached by Mölnlycke to form the Australian PITA Group. The group was formed in June 2021 and the first virtual advisory board meeting took place on 10th June 2021. Over a 12-month period, the group participated in a additional three online meetings, culminating in a final face-to-face meeting held in Sydney, Australia, in June 2022.
Throughout this series of formal advisory board meetings, with structured discussions moderated by Mölnlycke Health Care, the Australian PITA group collaborated to develop this 'Quick Guide'. This guide was developed to assist clinicians responsible for managing pressure injuries across various clinical settings, including acute care, residential aged care, and community settings. Its purpose is to assist these clinicians in identifying and implementing evidence-based interventions that align with local standard care and current international guidelines.
This article is excerpted from the A ‘QUICK GUIDE’ TO PRESSURE INJURY MANAGEMENTA ‘QUICK GUIDE’ TO PRESSURE INJURY MANAGEMENT by Wound World.
- 星期四, 12 10月 2023
Pressure ulcers and skin tone
Background
Pressure ulcers are a global threat and present a significant health challenge worldwide (Li et al, 2020). Evidence shows that it is difficult to accurately identify the early stages of pressure ulceration in patients with dark skin tones (Black, 2018); for example, patients with dark skin are more likely to be diagnosed with higher-category pressure ulcers than patients with light skin (Bates-Jensen et al, 2021; Cox and Hawkins, 2023). This is the result of a lack of early identification – e.g. redness can be easy to spot among people with light skin tones, but can be difficult to spot in dark skin tones (Chansky et al, 2017). Unrecognised damage arising from pressure ulcers in people with dark skin can lead to worsening stages; prolonged periods of hospital stay; deterioration in patients’ physical and psychological wellbeing; increased risk of sepsis and death; and elevated costs for healthcare services (Andersson et al, 2023). Therefore, there is a need to improve skin assessment skills among clinicians, as well as guidance on integrating pressure ulcer prevention best practice into all care settings where patients present with diverse skin tones.
