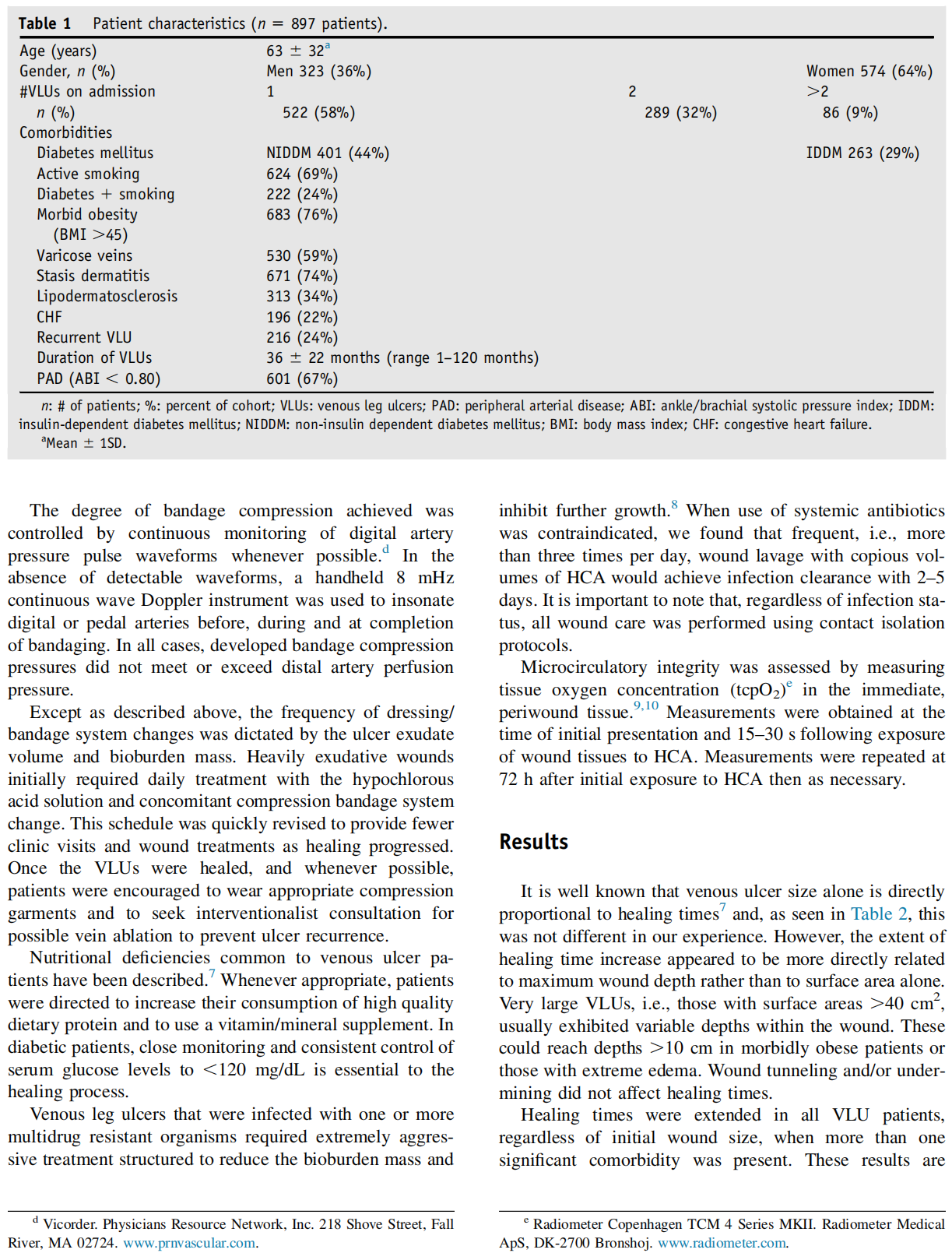
Abstract In order to assess the impact of comorbidities and identify factors that accelerate the healing rate of venous leg ulcers we performed an extensive, retrospective analysis of our experience in a diverse population. From June, 2006 to June, 2014, 897 patients with 1249 venous leg ulcers were treated at Lake Wound Clinics. Treatment protocols utilized the standard regimen of wound cleaning, debridement and compression bandaging. Wound cleaning, autolytic debridement, packing and dressing of venous leg ulcers utilized aqueous solutions of hypochlorous acid (HCA) rather than the standard normal saline. This protocol caused all ulcers to close completely. Comorbidities that delayed healing included uncontrolled or poorly controlled diabetes mellitus, advanced peripheral artery occlusive disease (PAD), active smoking, use of steroid medications and/or street drugs, large initial ulcer size and significant depth. Other factors, including advanced age, recurrent venous ulceration, stasis dermatitis, lipodermatosclerosis, morbid obesity and infection with one or more multidrug resistant organisms did not delay closure. From this experience we conclude that venous leg ulcer care protocols that clean, debride, pack and dress with hypochlorous acid solutions can reduce the effects of some comorbidities while accelerating healing times. Additional benefits are 2016 The Author. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
‘‘Chronic venous insufficiency’’ manifests as a cornucopia of clinical problems. The mildest of these is dependent edema that is readily relieved by elevation. The most severe is venous ulceration. Venous insufficiency is progressive and worsens over time. In the United States, it is estimated that 1% of the adult population, i.e., approximately 3.2 million people, have late stage venous insufficiency and either have, or are at risk for development of, venous leg ulcers.1 Although there are multiple factors that produce venous valvular incompetence in the superficial, deep and perforating veins, the end result is the same. Venous congestion and pooling cause increased




This article is excerpted from the Journal of the American College of Clinical Wound Specialists (2016) 6, 32–7 by Wound World.

